Imagine a hospital that learns from every patient visit the way a smartphone learns from every tap—quick, continuous, and ever‑improving. That’s the promise of a learning health system (LHS). Instead of waiting months or years for research to trickle down into practice, an LHS turns everyday clinical data into real‑time knowledge that instantly informs care. In this article we’ll walk through what an LHS really is, the pieces that make it tick, real‑world examples, the sweet spot between opportunity and risk, and a step‑by‑step plan you can start using today.
What Is a LHS?
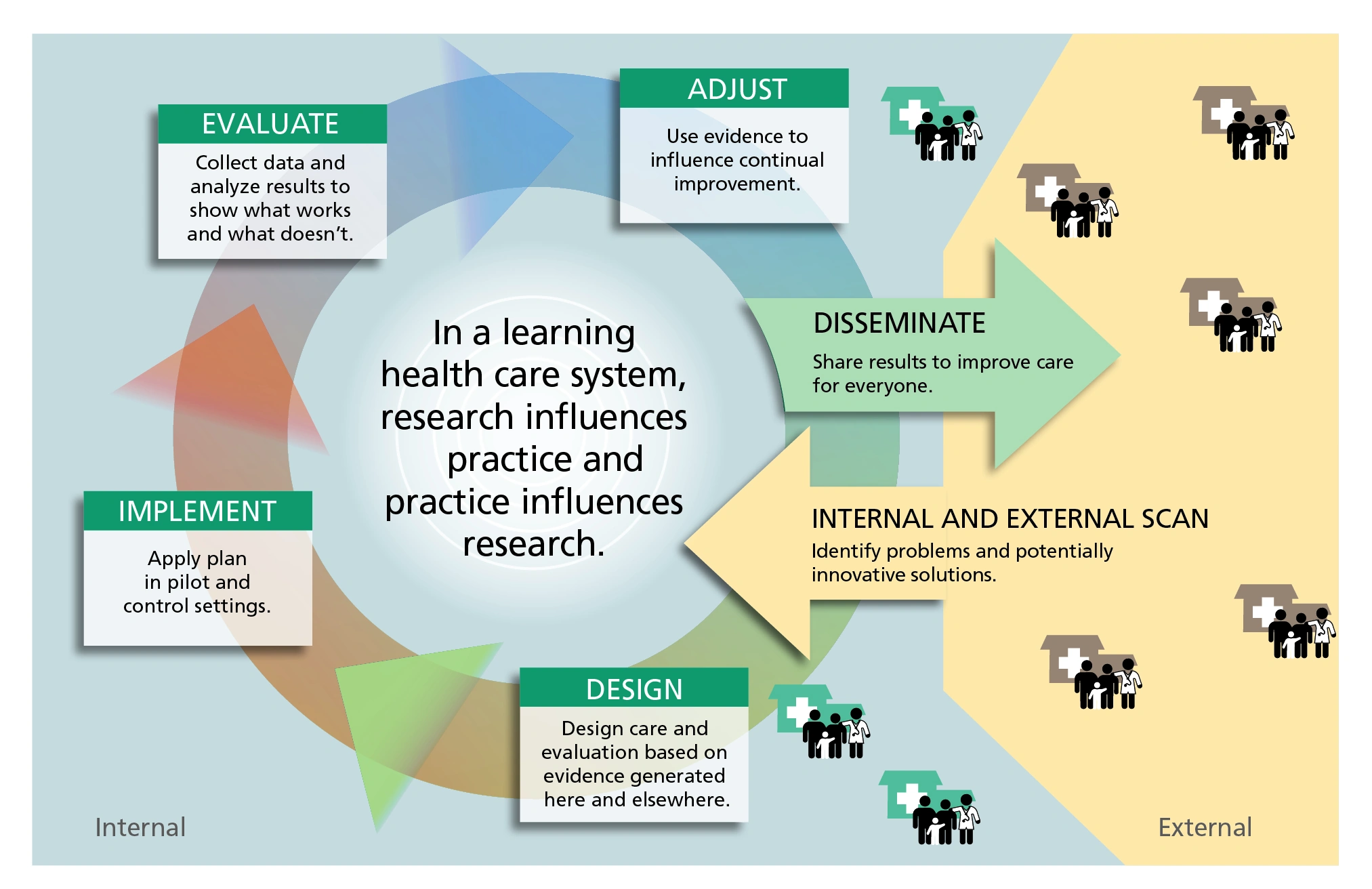
At its heart, a learning health system is a feedback loop that constantly cycles data, evidence, and practice. The concept was first sharpened by Charles Friedman and his colleagues, who described an LHS as a system where “science, informatics, incentives, and culture align for continuous improvement” a study. Think of it like a thermostat: the system reads the temperature (patient data), decides whether to heat or cool (generate an intervention), and then watches the result, adjusting again as needed.
How does this differ from a traditional health system? In a classic setup, electronic health records (EHRs) sit on a shelf and researchers pull data out once in a while. In an LHS, the EHR becomes a live sensor feeding an analytics engine that produces AI‑driven predictions, guideline updates, and alerts—all in the same workflow.
Why real‑time patient insights matter? Because the moment a trend emerges—say, rising readmission rates for heart failure—an LHS can flag it, suggest a change, and measure the impact almost immediately. This rapid cycle shrinks the lag between discovery and delivery, which directly translates into improving patient care.
Core Components
Building an LHS isn’t a magical switch; it’s assembling a few sturdy LEGO bricks. Below is a quick rundown of the five pillars that keep the system humming.
| Component | What It Does | Key Example |
|---|---|---|
| Data Infrastructure | Collects, stores, and standardizes clinical data. | Robust electronic health records that feed a secure data lake. |
| Analytics & AI Engine | Turns raw data into actionable predictions. | Machine‑learning model that predicts sepsis 6 hours before symptoms appear. |
| Learning Cycle | Generates evidence, updates practice, and measures outcomes. | Guideline‑driven order sets that auto‑update based on recent trial results. |
| Governance & Trust | Ensures privacy, fairness, and accountability. | Data‑use consent framework aligned with HIPAA and GDPR. |
| Workforce Development | Equips clinicians and analysts with the right skills. | Micro‑credential programs on data literacy and AI ethics. |
Each piece talks to the others. For instance, without solid governance, AI models might drift into bias; without a skilled workforce, the best algorithms will never reach the bedside.
Success Stories
Stories are the best way to see theory in action. Let’s peek at a few institutions that have turned the LHS dial up to eleven.
Kaiser Permanente Washington (KPWA) launched its LHS in 2017 and built a “logic model” that guided every decision. During the COVID‑19 surge, the model helped the health system roll out vaccine eligibility criteria within days, slashing appointment‑booking time by 15 % and boosting early‑vaccination rates among high‑risk groups.
Ontario’s SPOR Support Unit introduced a national Action Framework that couples research with daily operations. By leveraging real‑time patient insights, the province identified neighborhoods with the highest asthma ER visits and deployed targeted home‑ventilation programs, cutting those visits by 8 % in one year.
Wake Forest’s Academic Learning Health System illustrates how an LHS can serve multiple missions—research, education, and patient care. By embedding research questions into routine cardiology visits, they increased trial enrollment from 4 % to 20 % without extra staffing.
These examples show that an LHS isn’t reserved for tech giants; community hospitals, academic centers, and even regional health authorities can reap the benefits.
Benefits vs. Risks
Any powerful tool comes with a flip side. Let’s weigh the good against the not‑so‑good, so you can make an informed decision.
Clinical & Operational Benefits
- Speedy evidence uptake: New guidelines become practice within weeks, not years.
- Cost savings: Reducing duplicate tests and unnecessary admissions can shave millions off the bottom line.
- Patient safety: Real‑time alerts catch adverse events before they spiral.
Potential Pitfalls
- Algorithmic bias: If the training data under‑represents certain groups, predictions can be unfair. Transparent model cards and periodic bias audits are a must.
- Data‑security threats: A breached data lake can erode trust fast. Adopt “privacy‑by‑design” encryption and strict access controls.
- Change fatigue: Overloading clinicians with alerts can cause “alert fatigue.” Start small, iterate, and celebrate quick wins.
Ethical & Legal Considerations
Secondary use of patient data demands clear consent, and emerging AI regulations (like the FDA’s “Algorithmic Change Protocol”) require documentation of model updates. Aligning with these rules protects both patients and your organization.
Measuring Success
Key performance indicators for an LHS often include data completeness, learning cycle time (how quickly a new insight reaches practice), and patient‑reported outcome scores. A simple dashboard that shows these three metrics can keep everyone on the same page.
Build Your LHS
Ready to roll up your sleeves? Here’s a practical, six‑step roadmap that you can start today—no PhD in data science required.
1️⃣ Assess Current Infrastructure
Take inventory of your existing EHR, data warehouses, and analytics tools. Do you have the data you need (lab results, social‑determinant fields, device feeds)? Create a checklist and flag gaps.
2️⃣ Define Clinical Priorities
Gather physicians, nurses, and administrators for a “pain‑point” workshop. Prioritize projects that are high‑impact but low‑complexity—think “reduce readmission for heart failure” or “automate medication reconciliation.”
3️⃣ Establish Governance
Draft a “Learning Health System Charter” that outlines data‑use policies, consent processes, and accountability structures. Appoint a Data Stewardship Committee with representation from IT, compliance, and frontline staff.
4️⃣ Build the Analytics Engine
If you’re comfortable with open‑source tools, consider TensorFlow or PyTorch for model development. Otherwise, partner with a vendor that offers a plug‑and‑play AI platform. Set up a CI/CD pipeline so models can be retrained and redeployed automatically when new data arrives.
5️⃣ Pilot, Evaluate, & Scale
Launch a 6‑month pilot on your chosen clinical priority. Track adoption rates, outcome changes, and user feedback. Use the measurable constructs from the KPWA logic model (e.g., “time from insight to action”) to determine success. Refine and repeat.
6️⃣ Institutionalize Learning Culture
Close the loop by celebrating successes in staff meetings, offering micro‑credentials on AI in healthcare, and embedding learning goals into performance reviews. When learning becomes part of the everyday language, the system sustains itself.
Tip: Sprinkle short “learning moments” into daily huddles—ask, “What did we learn from yesterday’s data?” This simple habit keeps the feedback loop alive.
Future Trends
What will LHS look like in the next decade? Here are a few exciting directions.
AI‑Driven Digital Twins
Imagine a virtual replica of your patient population that runs “what‑if” scenarios in seconds. Researchers are already using federated learning to train models across multiple hospitals without moving the data.
Regulatory Landscape
Lawmakers are drafting a “Learning Health System Act” that would provide reimbursement incentives for organizations that demonstrate measurable learning cycles. Keeping an eye on policy changes will help you align funding sources.
Financing & Value‑Based Contracts
Payors are starting to reward providers for outcomes that stem from rapid learning—think lower readmission penalties when an LHS proves its interventions work.
Equity‑Focused LHS
When real‑time data highlights disparities (e.g., higher asthma attacks in low‑income neighborhoods), an LHS can mobilize community resources swiftly. This aligns perfectly with the goal of improving patient care for everyone.
Conclusion
Learning health systems turn every patient interaction into a source of knowledge, and every piece of knowledge back into better care. By combining solid data infrastructure, smart analytics, strong governance, and a culture of continuous learning, health organizations can accelerate improvement, cut costs, and deliver safer, more personalized care.
If you’re curious about where to start, try the quick‑win of mapping one clinical problem to a data source, then follow the six‑step roadmap above. Remember, an LHS is not a destination—it’s a journey you take with your whole team, one insight at a time. Let’s keep the conversation going: what challenge in your organization could become the first learning loop? Share your thoughts, and feel free to reach out if you need a sounding board.
























Leave a Reply
You must be logged in to post a comment.