What if it’s not just stress?
Seriously—have you ever had something go wrong in your body, and the first thing everyone (including you) says is, “Oh, you’re just tired, it’s probably nothing”? I’ve been there. It’s messy, frustrating, and sometimes even a little scary. That’s how my journey into the world of myasthenia gravis started. If you’re reading this because you—or someone you love—are chasing answers, trust me, you’re not alone.
Let’s talk honestly about the history of myasthenia gravis, what it really feels like, why it’s sometimes so hard to diagnose, and what new hope is on the horizon. We’re not going “textbook” today—I want to walk you through this like a friend who’s been there. So grab a cup of tea (or coffee, or whatever makes you feel cozy), and let’s dive in.
Understanding the History of Myasthenia Gravis
What is Myasthenia Gravis, Really?
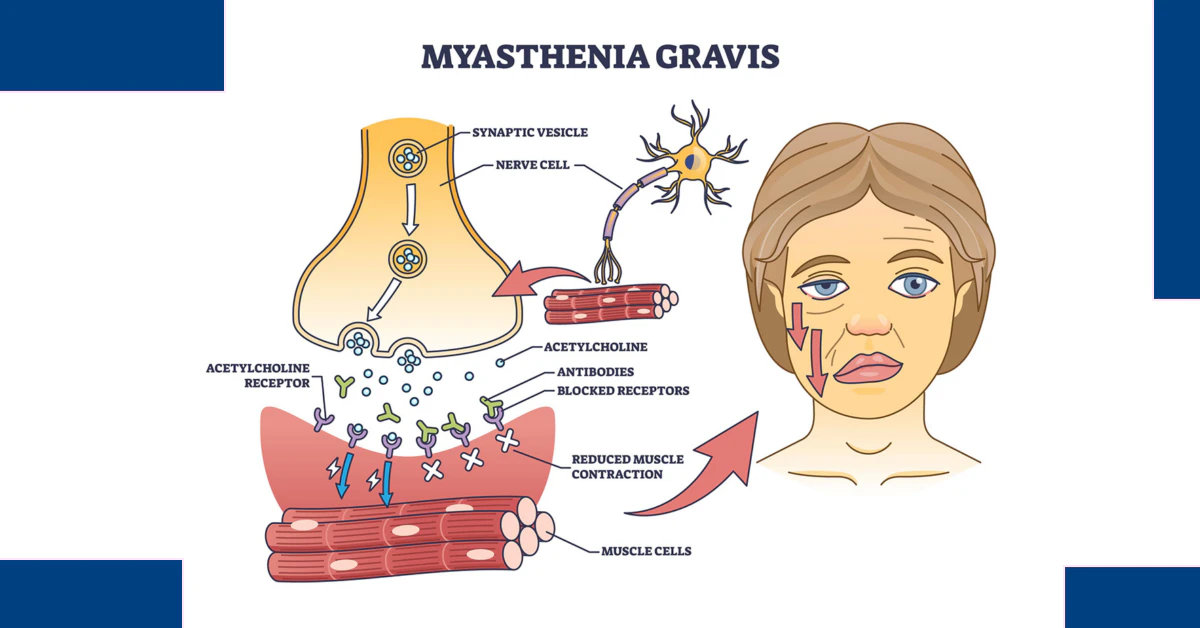
Okay, first things first: myasthenia gravis (MG) is a rare, chronic autoimmune disorder. In plain English, that means your immune system—usually your body’s personal security guard—starts attacking your own muscles by mistake. The result? Muscle weakness that can feel like your body’s batteries are running out, sometimes in the middle of the day.
It’s not just “being tired”—it’s like trying to lift your arms or keep your eyes open after an all-nighter, except you just woke up. This disease doesn’t care how motivated you are. It can hit anyone but is most common in women under 40 and men over 60. But the kicker? It’s often misdiagnosed, dismissed, or just plain missed. That’s part of its long, complicated history.
From Ancient Mysteries to Modern Medicine
The history of myasthenia gravis goes back more than a century—maybe even further, though people just didn’t have a name for it. Early doctors documented strange cases of “muscle fatigue” and drooping eyelids (ptosis), but it wasn’t until the late 1800s that MG started to take shape as a recognized illness. Back then, they didn’t understand the immune system the way we do now. I can only imagine how bewildering it must have been for patients to be told, “It’s all in your head”—when, in fact, it was right there in their bodies.
Fast forward to today: doctors know that MG is caused by a breakdown in communication between nerves and muscles, thanks to antibodies blocking the receptors needed for muscle contraction. It’s a classic example of an autoimmune condition—a family of diseases that also includes things like rheumatoid arthritis (and yes, there’s a diagnosis code for rheumatoid arthritis), lupus, and even super-rare things like autoimmune small fiber neuropathy. Each of these diseases has its own story, but they all share that “betrayal by your own body” feeling.
Myasthenia Gravis After Cancer Treatment—Is That Possible?
Here’s a twist: did you know it’s possible to develop an autoimmune disease after cancer treatment? It’s wild, but true. Some people, after surviving cancer, end up with new autoimmune problems like MG. Why? Well, cancer treatments—especially fancy new immunotherapies—can sometimes “wake up” the immune system so much that it gets a little confused about what’s friend and what’s foe. It’s like your immune system got a double shot of espresso and now it can’t sit still. I’ve talked to folks who’ve faced this double whammy, and their stories are both heartbreaking and inspiring. It’s a reminder that our bodies—and our medical journeys—don’t always follow the script.
Recognizing Symptoms & Getting Diagnosed
What Does Myasthenia Gravis Feel Like?
If you’re here because you—or someone you care about—have been Googling “why do my eyelids droop?” or “why do I keep choking on my food?”, you’re not alone. MG symptoms can be sneaky. One day you’re fine; the next, you can’t smile properly or hold your head up. The most common signs include:
- Drooping eyelids (ptosis) or double vision
- Muscle weakness that gets worse with activity and better with rest
- Trouble swallowing or speaking
- Difficulty breathing (in severe cases)
- General fatigue that doesn’t match your activity level
Sounds vague, right? That’s part of the problem. It’s easy to dismiss these things as “just stress” or “getting older.” But if you notice these symptoms, especially if they come and go or get worse as the day goes on, it’s worth pushing for answers.
The Diagnostic Rollercoaster
Let’s be honest: getting a diagnosis for MG can be… a ride. It took me months—lots of doctor visits, blood tests, and more than a few “are you sure it’s not just anxiety?” conversations. The process can involve:
- Blood tests to look for antibodies (like the intrinsic factor antibody test—though that’s more common for other autoimmune diagnoses, it’s sometimes part of the work-up for overlapping symptoms)
- Electromyography (EMG), which tests muscle response to nerve stimulation
- Sometimes imaging, like CT scans, to check for a thymoma (a tumor of the thymus, which can be related to MG)
And here’s where experience matters: you want a doctor who listens. Who really listens. Because you know your body best, and sometimes you need to advocate for yourself—gently, but firmly. Don’t be afraid to ask, “Could this be myasthenia gravis?” and insist on seeing a neurologist if the answers aren’t adding up.
Autoimmune Confusion: It’s Not Always What It Seems
Autoimmune diseases are like a family reunion where nobody gets along. They can mimic each other, overlap, and confuse even the best doctors. MG can look like autoimmune small fiber neuropathy (which affects the tiny nerves in your skin and organs), or be confused with things like multiple sclerosis, lupus, or even certain cancers. It’s enough to make your head spin.
And speaking of cancer, people often ask, is cancer an autoimmune disease? The answer is no—but there’s a weird connection. Some autoimmune diseases can increase cancer risk, and certain cancer treatments can trigger autoimmune responses (remember that “immune system double shot” from earlier?). So if you’re living with an autoimmune disease after cancer treatment, or you’re just worried about what’s going on in your body, don’t give up. Keep asking questions. Keep looking for answers. You’re not being a hypochondriac—you’re being smart.
Living with Myasthenia Gravis: Treatment & Daily Life
Old-School Approaches: What’s Worked So Far
Once you finally get that MG diagnosis, the next step is figuring out how to manage it. For years, treatment was pretty straightforward: anticholinesterase medications (which help nerves talk to muscles), steroids, and sometimes immunosuppressants. Each comes with its own pros and cons. For some, these meds bring dramatic improvement; for others, it’s a balancing act, managing side effects versus benefits.
| Treatment | How It Helps | Possible Downsides |
|---|---|---|
| Anticholinesterase meds | Boosts muscle strength | Stomach upset, cramps |
| Steroids (like prednisone) | Reduces immune attack | Weight gain, mood swings, long-term risks |
| Immunosuppressants | Dampens immune system | Infection risk, liver issues |
Some people also benefit from surgery to remove the thymus gland (thymectomy), especially if a thymoma is present. Everyone’s MG journey is unique. What works for your neighbor might not be your magic ticket, but don’t lose hope. There’s more out there.
New Hope: Treatments on the Horizon
The world of MG treatment is changing—fast. There are new treatments for myositis and other autoimmune diseases that are now being explored for MG, too. Monoclonal antibodies (like rituximab and eculizumab) are opening new doors for people whose MG just won’t budge. Clinical trials are happening all around the world, offering hope for those who haven’t responded to traditional therapies.
And this is where sharing stories matters. I was part of a clinical trial, and while it felt a little scary at first, it was also empowering. I met people who’d been searching for answers for years—and suddenly, we were part of something bigger than ourselves: science, hope, and maybe, just maybe, a step closer to a cure.
Day-to-Day Life: It’s Not All Doctor Visits
Living with MG is more than just medication. It’s about listening to your body, setting boundaries, and finding support. Some days you’ll feel like a superhero; other days, getting out of bed is the win. That’s okay.
- Build a support team—family, friends, doctors, online communities
- Learn your triggers. Maybe it’s heat, maybe it’s stress (yeah, the irony isn’t lost on me), maybe it’s skipping meals
- Give yourself permission to rest—no guilt allowed
- Stay curious about your own journey. What helps? What hurts? Keep notes, talk about it, share your experiences
Sometimes, you’ll need to explain MG to new people—at work, at school, even to strangers. It’s exhausting, but it also spreads awareness. You never know who needs to hear your story. And if you’re struggling, please reach out. Support groups can be a lifeline; you’ll find people who just “get it,” no explanations needed.
MG and Your Future: Insurance, Disability, and Real-World Hurdles
Can You Get Life Insurance or Disability with MG?
Let’s talk turkey: navigating insurance with MG can feel like running an obstacle course blindfolded. Questions like can you get life insurance if you have Crohn’s disease or life insurance multiple sclerosis come up a lot in autoimmune communities, and MG is no different. The answer? It depends—but it’s not impossible.
Some insurers are more understanding than others. They’ll look at your current health, treatment plan, and history. If you’re stable and managing well, you might get coverage (though sometimes at a higher rate). It’s similar with disability: yes, can you get disability for sarcoidosis, MS, and MG? Sometimes, but you’ll need documentation. Lots of it. Keep track of your symptoms, treatments, and how MG affects your daily life. Don’t be afraid to ask your doctor for help filling out forms. Advocacy organizations can also be a huge help here—don’t go it alone.
Navigating the Paperwork Jungle
Here’s my advice: don’t be afraid of paperwork. It’s tedious, but it’s your right. Keep copies of everything—doctor’s notes, test results, medication lists. If you’re denied coverage or disability, appeal. Again and again, if you have to. Persistence pays off, and you deserve support. Connect with advocacy groups; they know the ropes and can offer real-world tips that make a difference.
And if you’re feeling overwhelmed, remember: you’re not alone. There are more people out there with MG than you might think, and every voice matters. Sharing your story—online, in a support group, or even just with another patient—can spark hope and change.
Wrapping It Up: You’re Stronger Than You Think
So, what have we learned on this wild ride through the history of myasthenia gravis? It’s not just an old, mysterious disease—it’s a living, breathing challenge that real people face every single day. From confusing symptoms to misdiagnoses, from old-school treatments to cutting-edge research, MG is a journey. And it’s one that can feel lonely—but it doesn’t have to be.
If you’re reading this and nodding your head because some part of it sounds familiar—don’t ignore it. Don’t brush it off as “just stress.” Reach out. Ask questions. Demand answers. And if you ever feel alone, remember: there’s a whole community out here, and we’re rooting for you.
So, what’s your story? Share your experiences, your questions, your wins and losses. Let’s keep the conversation going—because together, we’re stronger than any autoimmune disease could ever be.






















Leave a Reply
You must be logged in to post a comment.