Let me start with a question: have you ever thought, “I finally survived cancer… why is my body acting up again?” If you have—oh, friend, you are so not alone.
Here’s a story I hear way too often: Someone gets through cancer treatment, breathes that huge sigh of relief, and just when life starts to feel “normal” again, weird symptoms pop up. Achy joints that don’t quit. Skin breaking out in ways it never did before. Mysterious fatigue that no amount of coffee can fix. If you’re nodding along, stick with me. This is for you.
Today, we’re diving deep into the wild, confusing world of autoimmune disease after cancer treatment. Why does it happen? What does it feel like? And more importantly—what can you do about it? Grab a cup of tea (or whatever comforts you most), and let’s make sense of this together. I promise, we’ll keep things real, practical, and maybe even a little hopeful.
Understanding Autoimmune Disease After Cancer Treatment
What Is an Autoimmune Disease, Anyway?
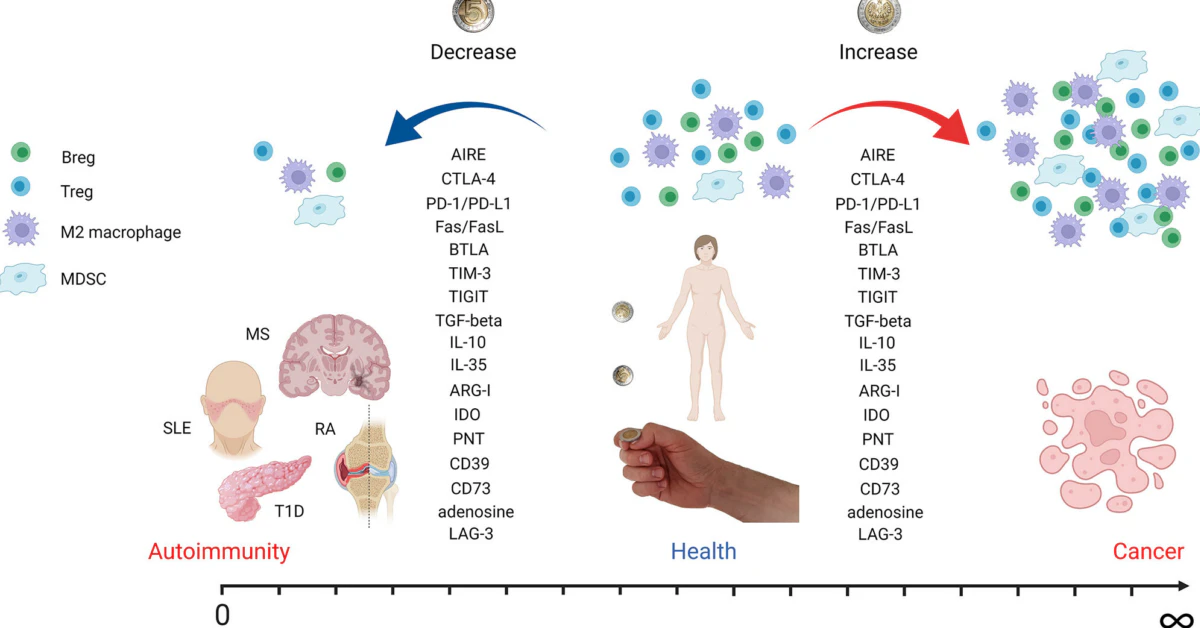
Okay, let’s keep it simple. Imagine your immune system is like a loyal guard dog. Its job? Protect you from invaders—bacteria, viruses, anything that doesn’t belong. But sometimes, after all the drama of cancer treatment, that guard dog gets a bit… confused. It starts attacking your own healthy cells, mistaking them for the enemy. That’s what we call an autoimmune disease.
There are a bunch of these conditions, each with its own quirks. Think rheumatoid arthritis (aching, swollen joints), lupus (fatigue, rashes), myasthenia gravis (muscle weakness), and even something called autoimmune small fiber neuropathy (tingling and pain that just won’t quit). The list goes on, and none of it is fun.
Is Cancer an Autoimmune Disease?
Short answer: No, cancer and autoimmune diseases are different beasts. Cancer is when cells grow out of control. Autoimmune disease is when your immune system attacks your body by mistake. But—and here’s the twist—sometimes the treatments for cancer can trip the wires in your immune system. That’s where the stories start to overlap.
➤ Learn Deeper into the Connection Between Cancer and Autoimmune Disease Check out Is Cancer an Autoimmune Disease? Find out now!.
How Cancer Treatments Affect Your Immune System
Let’s be real: cancer treatment isn’t gentle. Chemotherapy, radiation, and especially immunotherapy (the new kid on the block) are lifesaving, but they’re also tough on your body. They’re like dropping a bomb to get rid of the bad guys, but sometimes there’s collateral damage.
For some people, that “collateral damage” means the immune system gets so revved up (or so battered), it starts making mistakes. Your immune system might attack nerves (hello, autoimmune small fiber neuropathy), muscles (myositis), skin, joints, or even organs.
Real Talk: Why Does This Happen?
There’s no single answer—sometimes it’s the specific medication, sometimes it’s how your body reacts, sometimes it’s just dumb luck (and I say that with all the empathy in the world). The point is, if you’re dealing with weird new symptoms after cancer treatment, you are absolutely not imagining things. You deserve answers and support.
How Common Is It?
Here’s a stat that might surprise (or comfort) you: nearly 20% of people who finish cancer treatment end up with some kind of autoimmune issue. That’s one in five. You’re in crowded company, even if it doesn’t feel like it.
Who’s most at risk? Folks who’ve had certain kinds of immunotherapy, or people with a family history of autoimmune disease. But honestly, it can happen to anyone. I’ve seen it in marathon runners, grandmas, and everyone in between.
Recognizing the Warning Signs
What Symptoms Should You Watch For?
Let’s play a quick game. Which of these have you noticed since your cancer treatment?
- Unexplained fatigue (like, “how can I be this tired?” tired)
- Joint pain or swelling that won’t go away
- Numbness, tingling, or burning sensations—especially in your hands or feet
- Digestive drama: cramps, diarrhea, or sudden food sensitivities
- Strange rashes or changes in your skin
- Muscle weakness or droopy eyelids
- Vision changes, dry eyes, or mouth ulcers
If you checked even one of these, it’s worth talking to your doctor. Trust your gut. You know your body best.
When Should You Call Your Doctor?
This isn’t about being a hypochondriac. It’s about being your own best advocate. If you’re worried, ask. Some symptoms are mild and annoying; others, like muscle weakness from myasthenia gravis, can get serious fast. Early action is everything.
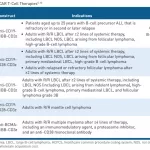
Common Autoimmune Conditions After Cancer Treatment
Here’s a quick look at some of the autoimmune conditions that can show up post-cancer. (Don’t panic! Knowledge is power.)
| Condition | Common Symptoms | Diagnostic Test |
|---|---|---|
| Rheumatoid Arthritis | Joint pain, swelling, stiffness | Blood test (diagnosis code for rheumatoid arthritis), imaging |
| Myasthenia Gravis | Muscle weakness, drooping eyelids | Antibody tests, nerve studies, history of myasthenia gravis |
| Autoimmune Small Fiber Neuropathy | Burning, numbness, tingling in extremities | Skin biopsy, nerve conduction studies |
| Sarcoidosis | Lung, skin, or eye symptoms | Imaging, blood tests, biopsy, can you get disability for sarcoidosis? |
| Crohn’s Disease | Digestive issues, abdominal pain | Imaging, colonoscopy, can you get life insurance if you have crohn’s disease? |
| Myositis | Muscle pain/weakness | Blood tests, muscle biopsy, new treatments for myositis |
| Multiple Sclerosis | Vision problems, numbness, weakness | MRI, nerve tests, life insurance multiple sclerosis |
Doctors may also use the intrinsic factor antibody test for certain autoimmune conditions, especially if you’re dealing with vitamin absorption issues or mysterious anemia.
Expert Strategies for Diagnosis & Management
How Are Autoimmune Diseases Diagnosed Post-Cancer?
Here’s the deal: diagnosing autoimmune disease after cancer treatment isn’t always straightforward. It’s a bit like piecing together a jigsaw puzzle, with some pieces missing and others upside-down. But you don’t have to do it alone.
Doctors will typically start with a deep dive into your medical history (yes, even the weird stuff), a physical exam, and then order blood tests—often looking for specific antibodies. Sometimes you’ll need imaging studies or a skin or muscle biopsy. If you hear the words “intrinsic factor antibody test,” don’t panic—it’s just one of the many clues doctors use.
Pro tip? If your symptoms are stubborn, ask for a referral to a specialist: a rheumatologist (for joints and connective tissue), a neurologist (for nerve stuff), or an immunologist (for the big-picture immune questions). You deserve answers from someone who gets it.
Why Early Diagnosis Matters
I get it—nobody wants more doctor appointments. But the sooner you get a clear diagnosis, the sooner you can start feeling better. I’ve met people who waited months, even years, thinking their symptoms were “just stress” or “getting older.” Don’t be that person. You’re worth more than that.
Treatment Options & New Advances
Here’s where hope starts to glimmer. Treatments for autoimmune diseases have come a long way. Some are old standbys—like steroids or immune-suppressing medications. Others are brand new, targeted therapies that can make a world of difference, especially for things like myositis or multiple sclerosis. If you’re curious about, say, new treatments for myositis, ask your doctor what’s available or in clinical trials.
The big challenge is balancing your cancer recovery with managing a new autoimmune disease. Sometimes that means working with a whole team—oncologist, rheumatologist, neurologist, nutritionist, and more. It can feel overwhelming, but you are building your own dream team. And hey, you’re the MVP.
Personalized Care Plans: What to Ask Your Doctor
- What’s the most likely cause of my symptoms?
- Which tests do I really need?
- Are there new or experimental treatments available?
- How will this affect my cancer follow-up?
- What side effects should I watch for?
- Can I connect with others who’ve been through this?
Living Well After Diagnosis
Okay, let’s talk real life—not just doctor’s offices and test results. Living with an autoimmune disease after cancer treatment isn’t the end of the story. It’s a new chapter. And you get to write it.
Lifestyle Changes That Really Help
- Diet: Anti-inflammatory foods are your friends. Think colorful veggies, berries, omega-3s (salmon, walnuts), and less processed junk.
- Movement: Gentle exercise (yoga, walking, swimming) can ease pain and boost mood. Listen to your body—rest is important, too.
- Stress Management: Meditation, deep breathing, journaling, therapy—find what calms your mind. Your immune system loves a peaceful brain.
- Sleep: Prioritize it. Healing happens when you rest.
And don’t underestimate the power of a good support group. Whether online or in person, connecting with others who “get it” can be life-changing.
Navigating Insurance & Disability
This is where things can get, well, complicated. Getting life insurance with multiple sclerosis or figuring out if you can get disability for sarcoidosis isn’t always straightforward. The same goes for questions like, can you get life insurance if you have Crohn’s disease?
Here’s my best advice: advocate for yourself, keep detailed records, and don’t be afraid to ask for help. Social workers, patient advocates, and even your doctor’s office can often point you in the right direction.
Finding the Right Care Team
Look for practitioners who listen, explain things clearly, and treat you as a whole person—not just a list of symptoms. Trust your gut. You deserve a care team that’s on your side.
In a Nutshell: You Are Not Alone, and There Is Hope
Let’s be honest: facing an autoimmune disease after cancer treatment can feel impossibly unfair. Like, “haven’t I been through enough already?” If you’ve ever felt that way, I see you. You’re not overreacting. You’re not being dramatic. You’re being real.
But here’s what I want you to remember: There is help. There are answers. You can still thrive, laugh, love, and live a beautiful life—even if your body is throwing you curveballs. Take it one step at a time. Ask questions. Demand answers. Connect with others, and never, ever lose hope.
If you have questions, want to share your story, or just need a little encouragement, drop a comment below. We’re all in this together. And honestly, that’s the best kind of medicine there is.

















Leave a Reply
You must be logged in to post a comment.