Crohn’s disease is an autoimmune disorder that leads to symptoms such as abdominal pain and diarrhea. Irritable bowel syndrome (IBS) can produce similar complaints and may also cause constipation.
A number of gastrointestinal (GI) disorders, including IBS and Crohn’s disease, share overlapping symptoms, which can complicate making an accurate diagnosis.
Crohn’s disease and another illness called ulcerative colitis are grouped together as inflammatory bowel disease (IBD) because they involve long-term inflammation of the digestive tract.
Although the names sound alike, IBS is a distinct condition that can cause many of the following symptoms:
- abdominal discomfort
- diarrhea
- constipation
The exact cause of IBS is unknown, but clinicians suspect multiple contributors — such as food sensitivities and disturbances in the gut microbiome — may play a role.
Continue reading to explore how IBS and Crohn’s disease overlap and where they differ.
Crohn’s disease vs. IBS symptoms
Many symptoms of Crohn’s disease and IBS overlap.
IBS symptoms
IBS symptoms often come and go, flaring on some days and easing on others. For many sufferers, certain foods act as triggers.
The most common symptoms of IBS include:
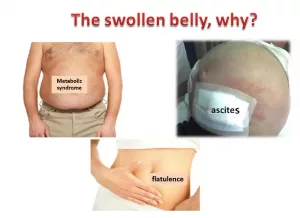
- bloating
- abdominal pain
- diarrhea
- constipation
Other possible symptoms are:
- excess gas
- mucus in the anal area
- fatigue
- nausea
- lower back pain
- frequent urination
- episodes of bowel incontinence
Clinicians often subtype IBS as:
- IBS-C if at least a quarter of stools are hard and lumpy while fewer than a quarter are loose
- IBS-D if the reverse is true
- IBS-M if you experience both stool types at least a quarter of the time
Crohn’s disease symptoms
Symptoms of Crohn’s disease may be persistent or recur in cycles lasting weeks to months.
The most common symptoms include:
- diarrhea
- abdominal cramps
- unplanned weight loss
- fatigue, which can be severe
Other potential signs include:
- fever
- nausea
- joint aches or pain
- eye redness or discomfort
- skin changes, such as painful, inflamed bumps
- mouth ulcers
- anemia
- loss of appetite
Read more about the symptoms and warning signs of Crohn’s disease.
What causes Crohn’s disease vs. IBS?
While Crohn’s disease has been linked to inherited genes, IBS likely arises from a mix of different factors.
IBS causes
The precise cause of IBS remains unknown. Some contributors that might influence its development include:
- traumatic early-life events, including physical abuse
- depression, anxiety, or somatic symptom disorders
- prior infections
- small intestinal bacterial overgrowth (SIBO)
- food intolerances or sensitivities
- certain genetic predispositions
- an altered gut microbiome
Crohn’s disease causes
The exact cause of Crohn’s disease isn’t fully understood either. However, researchers suspect a genetic component, since it appears more frequently in people with affected family members.
Crohn’s symptoms arise from an autoimmune reaction in which the immune system attacks normal tissues in the GI tract.
Who gets Crohn’s disease vs. IBS?
Below are known risk factors for both Crohn’s disease and IBS.
IBS risk factors
Risk factors linked to IBS include:
- female sex
- younger age groups
- previous GI infections
- anxiety or depressive disorders
Crohn’s disease risk factors
A family history of Crohn’s disease increases a person’s likelihood of developing it compared with those without such a history.
Other factors associated with elevated risk include:
- smoking
- exposure to air pollution
- use of nonsteroidal anti-inflammatory drugs (NSAIDs)
- certain infections
How Crohn’s disease and IBS compare with ulcerative colitis
Crohn’s disease and ulcerative colitis are both inflammatory disorders that fall under the umbrella term IBD. The primary distinction between them is where and how inflammation appears.
Crohn’s can inflame any part of the GI tract from mouth to anus, whereas ulcerative colitis affects the lining of the large intestine and rectum, producing inflammation and ulcers.
When to see a doctor
See a clinician if gastrointestinal symptoms are causing significant distress. It’s particularly important to seek medical advice if you have persistent diarrhea that:
- is very severe or happens frequently
- persists for longer than 7 days
- contains blood
How are Crohn’s disease and IBS diagnosed?
Initial evaluation for GI conditions typically includes:
- a review of your personal and family medical history
- a physical exam checking for signs such as bloating, abdominal tenderness, or pain near the liver or spleen
- laboratory testing, including blood work and stool studies
IBS is usually diagnosed by excluding other disorders. Physicians may suggest removing specific foods from your diet to see if symptoms improve.
Additional tests doctors might order when evaluating IBS include:
- endoscopic examination of the intestines
- X-rays of the upper GI tract (GI series)
- CT imaging
How are Crohn’s disease and IBS treated?
Although symptoms can overlap, treatment strategies for Crohn’s disease and IBS differ substantially.
IBS treatment
Common approaches to managing IBS include:
- increasing dietary fiber
- avoiding foods that trigger symptoms
- boosting physical activity
- staying well hydrated
- managing stress
- getting enough restorative sleep
- using appropriate medications such as antidiarrheals, laxatives, antispasmodic agents, or tricyclic antidepressants for pain relief
Find out more about home-based measures for IBS and see how they may help with ibs and brain fog.
Crohn’s disease treatment
Treatment for Crohn’s disease commonly involves:
- periods of bowel rest
- medications
- surgery
Surgical options may include removing affected sections of the bowel to relieve symptoms or reduce the chance of recurrence.
Medications can’t cure Crohn’s disease but may control inflammation and symptoms.
Drugs often prescribed include:
- corticosteroids such as prednisolone
- immunosuppressants like azathioprine (Imuran, Azasan), mercaptopurine (Purinethol), or methotrexate (Jylamvo, Maxtrex)
- biologic agents such as adalimumab (Humira), infliximab (REMICADE)
- vedolizumab (Entyvio)
Can Crohn’s disease or IBS be prevented?
There’s no known way to prevent Crohn’s disease, although adhering to medical advice can help you control the condition.
IBS might be partly preventable through lifestyle changes, including:
- preparing meals at home using fresh ingredients when possible
- keeping a symptom-and-food diary
- reducing stress
- exercising regularly
- trying probiotics for about a month to assess benefit
- limiting tea and coffee to under three cups daily
- cutting down on foods that trigger your symptoms
Takeaway
IBS and Crohn’s disease are two distinct conditions that can both produce abdominal pain and diarrhea.
Crohn’s disease results from an immune attack on healthy GI tissues, whereas IBS is associated with multiple factors, including food intolerances and disruptions in gut bacteria.
If you’re experiencing ongoing GI symptoms that disrupt your daily life, consult a healthcare professional. They can help determine the cause and suggest appropriate treatment options.



















Leave a Reply
You must be logged in to post a comment.