Yes – IBS (Irritable Bowel Syndrome) is a chronic illness. It won’t simply walk away on its own, but with the right tools you can keep the flare‑ups at bay and live a life that feels normal again.
In the next few minutes I’ll walk you through exactly why IBS is considered chronic, what the most common IBS symptoms look like, and practical ways to manage IBS through diet, lifestyle, and treatment. Think of this as a friendly coffee chat, not a textbook.
What Is IBS
Definition in plain language
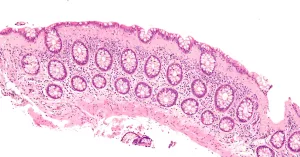
IBS is a functional gastrointestinal disorder – that means the gut looks fine on a scan, but it doesn’t behave the way it should. Muscles in the intestines may contract too hard or too weakly, nerves become overly sensitive, and the brain‑gut conversation gets a little…mis‑wired.
Why doctors label it “chronic”
When a condition drifts on for months or years, showing up repeatedly, we call it chronic. IBS symptoms tend to linger for six months or more and often re‑appear throughout life. The “chronic” label isn’t about danger; it’s a reminder that ongoing management—not a single cure—is the key.
How IBS differs from an acute gut issue
A stomach bug, food poisoning, or a one‑off infection usually resolves in a week or two. IBS, on the other hand, can bounce back weeks, months, even years after the initial trigger. It’s a bit like that friend who keeps calling—you learn to set boundaries, not ignore them.
Key Stats at a Glance
| Statistic | Source |
|---|---|
| Prevalence ≈ 5‑10 % worldwide | About IBS |
| ~ 2/3 of sufferers are female | IBS Impact |
| US healthcare costs > $1 billion annually | About IBS |
IBS Symptoms Overview
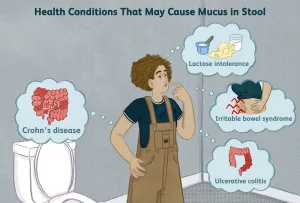
Core IBS symptoms
- Abdominal cramping or pain that often eases after a bowel movement
- Bloating and excess gas
- Diarrhea (IBS‑D), constipation (IBS‑C) or alternating both (IBS‑M)
- Feeling of incomplete evacuation
Red‑flag signs that aren’t IBS
If you notice any of these, it’s time to call your doctor right away:
- Blood in stool or black “tarry” stools
- Unexplained weight loss
- Fever, night‑time diarrhea, or persistent vomiting
- Severe anemia or joint pain
How symptoms can change over time
Many people describe a “boom‑or‑bust” pattern: a week of near‑normalcy followed by a sudden flare‑up. Stress, hormonal shifts, or a new medication can trigger the next wave. Understanding this rhythm helps you plan ahead—like keeping a symptom‑tracker handy.
Symptom‑Checklist (print‑friendly)
| Symptom | How Often? | Typical Triggers |
|---|---|---|
| Cramping pain | — | Stress, certain foods |
| Diarrhea | — | Caffeine, spicy meals |
| Constipation | — | Low fiber, dehydration |
| Bloating | — | FODMAPs, carbonated drinks |
Managing IBS Effectively
IBS diet that actually works
The low‑FODMAP approach is the gold standard for many folks. FODMAPs are short‑chain carbs that ferment in the gut, producing gas and pulling water into the colon. Cutting them down for a few weeks can give you a clear picture of what your gut tolerates.
Sample 7‑Day Low‑FODMAP Meal Plan
- Day 1: Breakfast – oatmeal made with lactose‑free milk, strawberries; Lunch – quinoa salad with cucumber, carrots, olive oil; Dinner – grilled chicken, zucchini, rice.
- Day 2: Breakfast – scrambled eggs, spinach; Lunch – rice noodles with shrimp and ginger; Dinner – baked salmon, roasted carrots, mashed potatoes (no butter).
- …continue for the week, rotating proteins and low‑FODMAP veggies.
Feel free to tweak the plan—just keep a note of any symptom spikes. If you’re unsure where to start, a registered dietitian can personalize it for you.
Lifestyle tweaks that calm the gut
- Stress‑reduction: Simple breathing exercises (inhale 4‑sec, hold 4, exhale 4) can lower the gut’s “fight‑or‑flight” response.
- Sleep hygiene: Aim for 7‑8 hours a night, keep a regular bedtime, and limit screen time 30 minutes before sleep.
- Regular movement: Even a 20‑minute walk after meals helps propulsion and reduces gas buildup.
Quick “Stress‑to‑Gut” Routine (2 minutes)
1️⃣ Sit tall, close your eyes. 2️⃣ Inhale through the nose for 4 seconds, hold 4, exhale slowly through the mouth for 6. 3️⃣ Repeat three times, then stretch your arms overhead. You’ll feel a subtle release in the belly.
Medical options for IBS treatment
When diet and lifestyle aren’t enough, medicines step in:
- OTC helpers: Fiber supplements (psyllium), anti‑diarrheals (loperamide), antispasmodics (hyoscine).
- Prescription choices: Rifaximin for IBS‑D, eluxadoline for mixed symptoms, low‑dose tricyclic antidepressants for pain modulation.
- Mind‑body therapies: Cognitive‑behavioral therapy (CBT) and gut‑directed hypnotherapy have shown solid results in reducing pain and anxiety.
When to talk to your doctor
Schedule an appointment if:
- Symptoms linger > 3 months despite self‑care.
- You experience any red‑flag signs listed earlier.
- Medications cause side‑effects or you need prescription options.
- You feel overwhelmed and could use a referral to a dietitian or therapist.
Living With IBS
The emotional side of chronic illness
Living with a chronic condition can feel like being on an emotional roller‑coaster. Anxiety, frustration, even occasional sadness are normal. The good news? You’re not alone, and there are ways to keep the mood swings in check.
Finding your support network
Connecting with others who “get it” makes a huge difference. Online forums, local support groups, or even a trusted friend who listens without judgment can become your safety net. A quick search for “IBS support groups” will reveal many options, and the community often shares practical tips you won’t find in textbooks.
Work, school, and travel hacks
- Tell your employer: Under the ADA you can request flexible breaks or a nearby restroom.
- Plan ahead for trips: Pack a “IBS kit” with your meds, a small bottle of water, and wipes. Identify restrooms on the venue map before you arrive.
- Social events: Eat a safe snack beforehand, and give yourself permission to step away if a flare‑up hits.
Real‑world story: turning limits into possibilities
Meet Maya, a 32‑year‑old graphic designer who once dreaded client meetings because of unpredictable IBS‑D episodes. After working with a gastroenterologist, she switched to a low‑FODMAP diet, started a nightly meditation habit, and negotiated a “flex‑hour” at work. Six months later she reports a 70 % reduction in flare‑ups and feels confident taking on bigger projects.
Trusted Resources
If you want to dive deeper, these reputable sites keep the information up‑to‑date:
- American College of Gastroenterology’s IBS guidelines (search “ACG IBS”).
- About IBS – patient‑focused articles and a symptom‑checker.
- IBS Impact – research summaries and advocacy updates.
- Chronic Pain Fighter – great read on stress and IBS interaction.
All the sources above have been vetted by medical professionals, so you can trust the facts you’re reading.
Conclusion
Let’s recap the three big take‑aways:
- IBS is a chronic illness that needs ongoing attention—not a one‑time fix.
- Identify your personal triggers—whether they’re foods, stressors, or medications—and use diet, lifestyle, and, if necessary, medication to keep them under control.
- Living well with IBS means balancing body and mind. Build a support network, communicate your needs, and celebrate the small victories along the way.
If any part of this resonated with you, feel free to share it with a friend who might be struggling, or drop a comment below with your own tips. Together we can turn the “chronic” label from a burden into a roadmap for a healthier, happier life.






















Leave a Reply
You must be logged in to post a comment.