You’re a patient named Sarah. You’ve heard the words “non-muscle invasive bladder cancer” enough to repeat them in your sleep. For decades, the go-to treatment has been BCG—a therapy with its roots in tuberculosis vaccines. But now? Researchers say combining BCG with a molecule from fungi could rev its power. Let’s unpack this without letting genetics defeat us in the process.
Or maybe you’re just here because immunotherapy is a buzword your friend mentioned, and you want to know if it’s just hype or something real. Let’s talk. And no, I won’t start by dressing you down with 50 years of lab history. Straight-up: recent science shows potential, but bladder cancer immunotherapy still has bumpy parts. Let’s dig in together.
Bladder Cancer Immunotherapy: More Than Just One Option
So, what is bladder cancer immunotherapy, really? Let’s say it’s your immune system’s personal couch screaming, “Hey, dumb tumor, we see you now!” Here’s the stripped-down version:
- Teaches your body to attack cancer cells
- Key players: BCG therapy, checkpoint inhibitors (like pembrolizumab), and antibody-drug conjugates
It’s not about heroics. It’s about coaxing your immune system out of its confused homeschool mode. Because let’s be real—cancer cells are sneaky little dogs. They blend in. Immunotherapy? It kicks them out of disguise. Check this out—innovative combinations are starting to test this in real-time clinics.
How Does This Therapy Even Work?
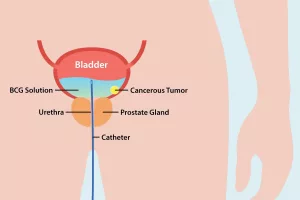
If your bladder’s been invaded by non-muscle invasive cancer, BCG therapy is your gatekeeper. Imagine it’s like hiring a bouncer to tell rogue cancer cells, “You’re not crashing this party.” It’s a live bacteria (don’t freak out—your body trains around it), and it stimulates aggressive immune reactions right in your bladder..
But even with BCG, it’s not foolproof. Some patients see it as the bodyguard of choice; others…well, crickets chirping.
| Therapy Type | Target | Stage Approved | How It Works |
|---|---|---|---|
| BCG | Bladder lining | NMIBC | Bacteria kicks immune system into tumor-busting mode |
| Checkpoint Inhibitors | PD-1/PD-L1 proteins | Advanced/metastatic | Hacks the tumor’s “firewall” so immune cells see it |
| Antibody-Drug Conjugates | Specific proteins (e.g., Nectin-4) | Metastatic | Guided missiles: antibodies deliver chemo straight to cancer cells |
Why This Matters
Your body’s cells are like a crowded traffic jam. Immunotherapy’s job? Add lane markers so your immune cells don’t pile up. For NMIBC patients, BCG hits around a 70–75% positive response rate, but that leaves plenty of room for doubt. And that’s why this 2025 twist? It’s our shot at narrowing the gap even more.
The Evolution of BCG: From TB Vaccine to Tumor Smasher
Guess where BCG came from? The tuberculosis vaccine. Yeah, the one teenage you got if you grew up outside the US. But in 1959, Drs. Old and team stumbled on an observation: injecting BCG into mice made their tumors crack. That lucky break? The spark for what we know as bladder cancer immunotherapy today.
BCG’s 1990 Explosion in Bladder Cancer
Jump to 1976—you’re in a clinic, peeing a bottle of bacteria into your bladder. Mind-numbing? Yeah. But effective? BCG became the first-choice therapy for NMIBC, and by 1990, the FDA gave it the stamp of approval. It’s still the benchmark more than three decades later, which isn’t just nostalgic—it’s functional.
Coffee pun: BCG = the espresso shot for your tumor. Not flash, not overly sweet—just gets the job done for many. Still, like your morning pick-me-up, it works for some people better than others.
BCG’s Current Standing
Tuberculosis vaccine, nonchalant bacteria, and a half-century of relevance—BCG’s still around because it works more than it doesn’t. But let’s call it what it is: imperfect. Some tumors don’t care. Others might respond initially but shrug it off after a few rounds. Sound familiar? We’ll talk about enhanced immunotherapy next—they’re still fine-tuning this thing.
2025 Big News: Enhanced Immunotherapy With a Fungal Twist
Imagine this: A team at the McGill University Health Center, led by Dr. Maziar Divangahi, drops a bombshell study suggesting a fungi-derived molecule could supercharge BCG therapy. Naps, stress breaks—hard pass. Let’s dive into what this means:
Fungi + BCG = Better bladder Cancer Fight?
Here’s the experiment: BCG therapy was already decent. But when paired with this natural molecule from fungi, the immune response gets rowdy. It’s like inviting a wrestling buddy to your workout group. Tumors? End up buried in a dogpile of immune vigilance.
Downside? It’s early. This isn’t your neighborhood pharmacy shelve stuff—yet. But pre-clinical tests in mice have made ripples. Let’s not start downing champagne just yet—though for some patients? This could be the breakthrough their bodies have been waiting for.
Risks and Projections
We’ve seen it: one size never fits all. Sure, combing a fungal molecule adds armor. But does it overbake your treatment? Up to your doctor, not your intuition yet.
- Early hypothesis: less fatigue, fewer severe reactions
- Reality check: not yet definitively safer than standard BCG
What’s clear is this—it opens doors. Could patients with weak BCG responses finally have real options? Maybe 2026 gives us the answer. But for now, it’s like chef’s kiss toward a longer average remission window.
Bladder Cancer Immunotherapy Sucks When It Doesn’t Work
Because here’s what they won’t tell you: immunotherapy doesn’t always play fair. Some patients? Hall-of-fame response. Others? The crickets again. What gives? Let’s dissect the messy parts of being cut from microbial battle:
Why Your Body Might Not Kick Back
Take Billy, a patient with NMIBC. He tried BCG twice. Response? Zero. Why? His tumor microenvironment was like a fortress. It coughed up debris bits. It dodged immune scouts. His bio map? Not alliance-friendly.
A 2020 study highlighted that about 30% of patients don’t respond to BCG. Imagine being caught in that lottery? Not fun.
Key Efficacy Factors
Tumors are rebels. Resistance forms because of multiple factors:
- Tumor heterogeneity (cancer clones hang out in like-minded clubs)
- Prior treatments muddled his immune system
- Immunosuppressive tumor microenvironment
Side Effects? Some We Hate, Others Just Annoying
Let’s say it plain: immunotherapy can be a harsh workplace boss. For some patients, it’s fatigue and minor burns. For others? It can trigger organ inflammation you cannot ignore.
What To Watch Out For
| Side Effect | Mild (manageable) | Action Required |
|---|---|---|
| Bladder irritation | Burning, urgency | Take your pain reliever and nap. But if blood stays? Recheck |
| Organ inflammation | Coughs, low fevers | Call doctor immediately. Pneumonitis or hepatitis swells the danger zone |
| Rare neurological | Headaches, strange numbness | Drop everything. It’s uncommon but sobering |
Price Tag? Sometimes It Hurts
If BCG is affordable, most folks breathe. But switch to checkpoint inhibitors or ADCs? Your wallet crinkles. Pembrolizumab costs around $5,000 a dose without insurance. That’s everyone’s math skills because not every patient fits gold-standard BCG profiles—sometimes combo therapy is the only way forward.
Who Actually Benefits from Immunotherapy? Numbers, Stages, and Question Marks
“Bladder cancer immunotherapy” might sound like a universal solution—but it’s not. Success depends on your stage, specific markers, and how well your body nods back to the commands this therapy calls out.
NMIBC vs. Muscle-Invasive: Therapy’s Dividing Line
Bladder cancer spans stages. NMIBC stays put—a win for preservation. Role of BCG here? Almost a stage-spliced heavy-hitter that wins 55-65% of high-risk papillary tumors, and a cozy 70-75% for those carcinomas in situ (“carcinoma in situ,” that aggressive looker your doctor’s eyes dread).
Muscle-invasive or advanced? Then it’s like trailing through a minefield. That’s where checkpoint inhibitors or conjugates pull weight after chemo fails.
Are We Missing Biomarkers? A Pothole for Predictability
Like guessing Spotify tastes from playlist skips—this remains a skillset the research world can’t nail yet. Some tumors shed markers PD-L1 or TMB (Tumor Mutational Burden). Others? Blank-faced. There’s no simple G-code patch. So—imagine aiming arrows blindfolded.
What Predicts a Response? Current Certainty
| Marker | Clarity Level | Key Research Findings |
|---|---|---|
| PD-L1 Expression | Mix | Explains 40-60% of responses, but not consistent |
| TMB (Tumor Mutational Burden) | Improving | Higher TMB often means better immunotherapy chance |
| New Neoantigens | Early research | Key holy grail investigators are chasing |
Cancer Immunotherapy’s Red Flag: Resistance, Biomarker Gaps, and When It Triggers a Breakdown
Here’s salt to the wounds: immunotherapy doesn’t just let you down quietly. Sometimes it revs your immune system to knight-level aggression and then your tumor builds a forcefield. That’s resistance—primary and acquired.
Primary vs. Acquired Resistance: Same Fight, Two Sides
- Primary resistance: Doesn’t work from round one
- Acquired resistance: Initially works, new tumor strategies trip you up
Depression as a side effect? How your mind feels. Treatments alone won’t deal with this mind-body response. MDPI chased this, not just for immediate damages but to gain ground on deeper cancer biology.
Antibiotic parallel: it’s like infection-killers knowing how to spin your calendar. Immunotherapy? The same, with cancer cells as skilled defectors.
So—is there a crystal ball? Not yet. One day. Maybe.
Real Emotion: Side Effects Can Be Scary
You start treatment, and voilà: your bladder’s tight. Your lungs? Suddenly need a security check. Some reactions burn out in days. Others—like hepatitis or pneumonitis—blow the budget of your daily life hustle. The safety paradox: your therapy forgets boundaries and treats your organs like open pasture. (Not cool.)
Immunotherapy side effects aren’t about laziness. You beat a treatment’s parameters for survival, and that leads to serious after-effects. So discuss what’s too much early—TRUST the warning light.
The Next Frontier: Combinations, Clinical Trials, and Biomedical Sweat
Mosquitos bite harder in their swarm than one-by-one. Similarly, immunotherapy’s future doesn’t lie in isolation—it’s combos we’re rooting for. What does 2025’s crystal ball say? Check these directions:
Combination Therapies: What’s in the Mix?
It’s like gourmet cooking: throw two strong flavors and lets see the explosion. BCG + the fungal boost we mentioned earlier? One way researchers psyche bold moves.
Or combine immunotherapy with PART inhibitors to double-cross tumor pathways.
But with combos, side effects often stretch into messier territory. Fatigue dials up. Organ inflammation ushers in more intense rounds of checks. Real balance required.
Refining Clinical Trials: The Less-Stiff Way
Traditional trial design works for pills and placebos. But immunotherapy thoughts? Different beast. We’re moving toward:
- Biomarker screening before trial entry—effective filtering
- Adaptive trial formats—letting the data call the next play
This shift pushes patients into better responses faster while limiting roadblocks. The future of ADCs loves flexible testing, especially for accuracy. Nobody explains immunotherapy better than cravings met. Even research is like that.
Conclusion: Hope Needs Realness Attached
wew what a journey. We started with BCG’s birth from tuberculosis vaccine, climbed through its immune-buzzing legacy, checked out the 2025 fungal molecule twist, and heaved sighs over its side-effect landmines.
Immunotherapy? Hope and skepticism tangled. It’s not the savior, but it’s not the road block either. Checked delays include unpredictable response people, pricing mood swings, and the daily sprinkle of potential toxicities.
If you’re facing this, your doctor’s job is critical. Ask them fat fees, miracle odds, and whether any trials could work for your case. The mission isn’t about one-size-fits-all—it’s about adding personally-tuned confronts against cancer’s lobes.
Stay curious, but real about it. Whether you’re newly diagnosed or several rounds in, the marriage of science and openness makes all the difference. So what’s next for you or someone you care about? We’d love to hear your questions—drop one in a comment or whisper it like strangers on the subway tapped post content.


















Leave a Reply
You must be logged in to post a comment.