So here’s the truth: Around 20% of long-term smokers who get annual LDCT scans avoid dying from lung cancer. But the catch? False positives are real messy. Experts aren’t screaming “screen everyone!”—they’re urging balance. Because saving lives isn’t just about finding tumors.
Still confused? You’re not alone. Screening isn’t simple. Let me walk you through what no one’s telling you upfront… without the jargon or fearmongering.
Who’s Eligible? Let’s Cut Through the Fog
First things first: Screening isn’t for everyone. It’s for folks aged 50–80 with a >=20 pack-year smoking history who still smoke or quit within the last 15 years.
Okay, but what the heck is a “pack-year”? Simple: 1 pack/day x 20 years = 20 pack-years. Smoked 2 packs/day for 10? Same thing. The math isn’t scary—it’s just about tracking how much you’ve inhaled over the years. (And if you’re non-binary or hate math, here’s a visual guide to make sense of it.)
If you’re still healthy enough for treatment? Screening makes sense. But if serious health issues are holding you back? Or you’d skip surgery either way? This might not be your fight.
And here’s the kicker: It’s not just the U.S. moving this way. Australia kicked off their high-risk screening program in July 2024, mirroring global efforts to catch lung cancer early. (Although experts are raising eyebrows about rural access in their country—wait for it.)
The Big Upside: Catching It Before It Screams “I’m here”
Lung cancer is the stealthy type. It doesn’t cough, wheeze, or throw up red flags. By the time you notice something’s off, it might’ve already packed its bags and hopped to other organs.
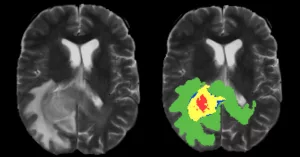
That’s where LDCT scans shine. These aren’t your average chest X-rays. The top-level National Cancer Institute trials showed they slash mortality by up to 24% in high-risk smokers.
But here’s the thing:
Eligibility rules are shifting. In 2021, yes, the USPSTF expanded screening to ages 50–80 with 20 pack-years. (This isn’t old news—it’s barely three years old.) You’re no longer excluded for “only” 20 years of smoking instead of 30. Good for younger quitters who thought they’d dodged the cancer bullet… but might still need the scan.Harms You Need to Know About
Still with me? Let’s get honest. Screening isn’t all sunshine. Ever had a blood test scare? Now imagine that for your lungs.
False positives—they’re a mood killer. Around 1 in 4 LDCT results show “abnormalities” that are not cancer. (Thanks, National Lung Screening Trial.) The aftermath? More scans, biopsies, and that gut-wrenching wait for answers.
Overdiagnosis is the quiet storm. Some cancers caught on scans are so “calm,” they’d never hurt you. But once found, pressure kicks in to “do something.” (One study called this the healthcare version of a gift that keeps on giving.)
And the radiation doses? They’re low. But if you smoke and need repeat scans? It’s like getting soaked in a drizzle over years. Risky, or just normal weather? Real talk: Total exposure is less than standard CT scans, but higher than an X-ray.
What the Scan Reveals (and What It Doesn’t)
Imagine lying on a machine that whooshes, buzzes, and wraps your chest in brackets. No pain involved. Just minutes of mature silence. But afterward? That result can change your life—maybe.
Returns to negative: Breathe easy… but schedule your next scan. (And if you’re still smoking, here’s your push to stop—resources for that.)
Positive result? Drs will talk nodules larger than 6mm. Some might be smoke-related scar tissue. Others? Why you’re grateful they ordered the test. (No need for panic—most turn out non-cancerous.)
Indeterminate results? That’s when you hear “come back in 3–6 months.” It’s cancer limbo—annoying, but necessary. (TRUST ME, I’ve been there. More on that in a bit.)
Quick Comparison: Screening Roads
| Method | Mortality Reduction | False+ Rate |
|---|---|---|
| LDCT | 20–24% | 10–23.3% |
| Chest X-ray | No significant reduction | 5–10% |
Ever wonder why some people are excluded despite smoking for decades? (Here’s the cut:: screening works best for “healthy high-risk” patients. If you’ve got COPD doing the heavy lifting, the risks of follow-up might outweigh the upside.
Real Talk: Stories from Screened Smokers
Here’s where science goes personal. John, 63, smoked two packs/day for 35 years. When his scan lit up, he panicked. “Turns out, it was a granuloma,” he laughs now. “But that hour waiting in the clinic? Pure torture.”
Maria, 58, had two scans showing suspicious nodules. Biopsies turned up empty. “Worth the stress? Yeah,” she says. “Because if it’s not cancer, you’re free to focus on quitting. And if it is… you’ve got a shot.”
These stories aren’t about gloom. They’re about data with a face. If you’re eligible, watchful wait or action? It’s your call. And that’s something no algorithm gets right—only you and your doctor.
What’s Next: Your Move, Not Google’s
You’ve got your summary, your numbers, and even a table. Now what?
If you smoke: This is your sign. Seriously. Screening isn’t a free pass to keep puffing. (Experts back this—for every year you quit after age 50, lifespans tick out by two.)
If you quit: Your risk’s dropping, but it’s not gone. Screening still applies—and yet, the American Cancer Society’s 2023 guidelines give a clearer window for folks like you.
If you’ve never smoked: We’ve got nothing. Not yet. (Around 10% of cases occur in non-smokers, but criteria don’t cover them. Way too much mystery left.)
At the end of this? You’re not a diagnosis. You’re armed with reliable facts. Whoever you are, make that call with your doctor. No tab-fishing. No lies. Just a conversation that’s worth having.





















Leave a Reply
You must be logged in to post a comment.