You know those tiny things inside your cells that make energy? Yeah, mitochondria—we all heard about them in high school biology, right? Well turns out, when it comes to cancer, mitochondria and chromosomes have a kinda messed-up relationship. And guess what? That relationship might be the key to new ways of fighting tumors. Let’s dig into how chromosome imbalances in cancer cells are shaking up what we thought we knew. Let’s start at the beginning—because trust me, it gets wild.
The ‘Protein Overcrowding’ That Messes With Your Cells
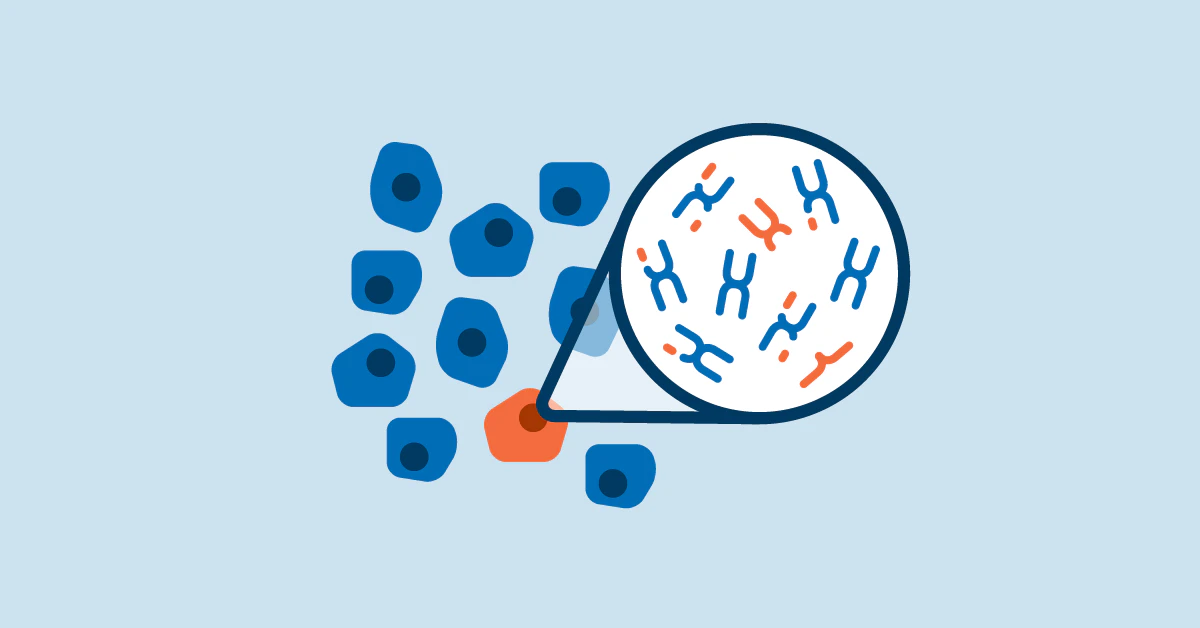
Cancer cells love to play fast and loose with their DNA. Most of them have way too many—or way too few—chromosomes. It’s like… chromosomal traffic all over the place. This is called aneuploidy. But here’s the thing: these imbalances don’t just look odd under a microscope—they mess with the whole cellular system. Because when you have extra or missing chromosomes, you automatically make too much—or not enough—of certain proteins. It’s like baking a cake with 5 cups of sugar instead of 2. The mitochondria—the powerhouse within these cells—suddenly find themselves drowning in chaos.
Why Protein Imbalance Cells Go Haywire
One recent study from RPTU found that protein overflow caused by chromosome imbalances actually slows down mitochondria. Think of it like electrical overload—too many fans running in one room and the circuit breaks. In cancer cells, the more messed-up the protein balance, the harder it is for the mitochondria to function—and sometimes, they just power down entirely.
How Aneuploidy Shapes the ‘Personality’ of a Tumor
Cancer isn’t predictable. Some tumors stay quiet for a while. Others spread like gossip. But oddly, aneuploidy gives tumors their distinct ‘feel.’ Like, some researchers now think that certain imbalances create tumors that are super aggressive—while others trigger self-sabotage. Imagine a group of rebels growing out of control versus one that trips over its own feet. That’s what some chromosome imbalances do to cancer cells.
Chromosome Abnormalities Study Unlocking New Angles
If you’ve ever heard someone say cancer is a game of hormones or viruses, they’re not entirely wrong. But more and more, chromosome abnormalities study is showing that DNA chaos isn’t some random background noise—it’s a driver of the show. It affects which genes overachieve… and which ones vanish under stress. And it changes how a tumor responds to treatment. Yep, the kind of chromosomal chaos in your body might dictate whether a drug can punch the right buttons in a tumor.
So Chromoscope Imbalances Cause Mitochondrial Breakdowns. What Next?
If you’re picturing cancer cells like overconfident minions speeding up with extra chromosome copies, hold on. This new research flipped that idea upside down. Instead, chromosome imbalances cancer cells have? They actually get weird technical problems. Their mitochondria can’t keep up. And the more messed up the DNA… the sicker those powerhouses get. Which means we might be able to exploit that weakness.
How Damaged Mitochondria Push Cancer to an Unexpected Corner
Here’s the kicker: mitochondria are all about energy and metabolism. When they get hit by chromosomal hiccups, the tumors start getting a little moody. They become sensitive to treatments that shut off cell energy… or they begin crashing faster than a soufflé. The mitochondrial function cancer connection isn’t just a science thing—it’s like finding a backdoor into the enemy base.
Can We Flip Mitochondrial Stress Into Cancer Drug Treatment?
You’ve heard of drugs that stop tumors from dividing? Yeah, but maybe we can push this further. If mitochondrial damage in aneuploid cells can be controlled or even accelerated, there’s this idea we could create DNA-chaos targeted drugs. Some of our early cancer drug treatments—like Gleevec—algone tapped into chromosome-based solutions. But now we know: that was only scratching the surface.
Why Studying Chromosome Imbalances Feels like Playing Whack-a-Mole
Okay so now you’re wondering: “Why don’t we know more about this if it’s such a big deal?” I get it. Cancer research sounds like a clean, slow march forward… but sometimes it feels more like an embarrassing video game from the ’80s. Because of this aneuploidy issue—it’s not a small glitch. It’s a flipping avalanche. Imagine trying to find the culprit in a movie with 3,000 characters. That’s what researchers face—big chromosome chunks with hundreds of gene possibilities at once. It’s so tough to isolate the real bad actors.
Chromosomal Instability (CIN) as Cancer’s Jekyll and Hyde
And then there’s the drama of chromosomal instability—CIN, to its friends. Think of CIN as that Instagram comment section. It’s fine… as long as there’s just a little chaos. But if you crank up the CIN too far, cancer can’t survive. That’s the paradox: sometimes, the more unstable the DNA, the less room there is for cancer to adapt. But when it’s just ‘right,’? It hurts us. Makes it super hard to target. This is why some drugs work at first… and then stop. Your tumor? It’s getting remix ideas from its DNA.
Why Too Much Chromosome Chaos Means ‘Game Over’
Alright, remember that bit about “extra chromosomes being bad”? Yeah, it’s true but only to a point. Some tumors, like colon cancer, actually reach a breaking point—too many chromosomal errors, and the cells get tired. They hit the brakes. Which means maybe certain gene defects will help us identify cancers more likely to respond well to mitochondrial-impacting treatments. That’s the silver lining here: not every chromosome imbalance stacks the deck against us. Some of them actually trap cancer in biological dead ends.
Real-World Case: Philadelphia Chromosome Discovery
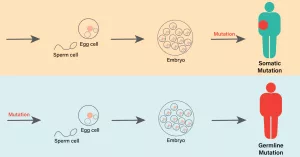
Quick history flash: back in 1960, Peter Nowell and David Hungerford found this weird, bent chromosome in leukemia cells. It later got labeled the Philadelphia chromosome (yes, really, because Jerry and George weren’t doing research then). But here’s why this matters: that discovery was the first strong proof of how chromosome abnormalities shape cancer itself.
| Discovery | Year |
|---|---|
| Philadelphia Chromosome in CML | 1960 |
| p53 Tumor Suppressor Gene Found | 1989 |
| Chromosomal Instability Recognized | 1999 |
Chaos Theory Meets Cancer Medicine
If you’ve ever dealt with a friend who changes the plan literally every 20 minutes, you know the struggle with CIN. Sometimes it’s what makes the tumor habitable for mutations… and other times, it’s like crashing the system. Understanding this means picking the right time to step in—before DNA chaos runs off the rails.
Are Tumor Cells ‘Cheat Sheet Experts?’
Lots of research says yes. Tumors ‘hack’ their chromosomal mess. They keep special genes that help them survive… while junking genes that would normally slow them down. It’s survival math. But even those rogue cells can’t predict where the DNA chaos ends. That’s the unpredictable nature of chromosome imbalances in cancer.
Where Are We Headed—and What’s the Hurdle (Right Now)?
Let’s be honest. We’ve got brilliant minds on this, and we’re closing in. But the study models we use? They’re like stage lights that only show one corner while the rest remains dark. Lab mice and human tissue don’t always mirror each other in the CIN game— and keeping the balance between too-much and just-right is still super flimsy science. But how do we work around this?
The MIT Problem Every Lab Dreads
Dig this. You can’t simulate chromosome instability just by dropping a few genes. It’s connected to hundreds of other processes. Removing one could help stopping CIN… or accidentally create genetic time bombs. So far, our tools? Let’s say they’re more makeshift game than F1 racing. But every Einstein in cancer labs is working on this. And progress is coming.
Can Chromosome Testing Give More Treatment Hope — With Less Guesswork?
Picture this: your doctor pulls up a list and says, “Hey, this part of chromosome 5 is tipped. So we can try this therapy that hits the mitochondrial fuel lines of your cancer.” Sounds like sci-fi? It’s not super sci-fi anymore. The Broad Institute is already running huge data models to map which aneuploidy patterns work best with different drug treatments.
Top 5 Data Crunching Hurdles in Aneuploidy Medicine
- High heterogeneity in individual tumors
- Missing CIN-glitch triggers
- Drug response unpredictability
- Lab model limitations
- Time lag from research to clinical testing
Are We Learning to Play Cancer’s Weakness?
It’s a play on counter-intuition. If we can’t fix chromosome imbalances, maybe we can create drugs that make them worse. Sounds silly, but some believe that tipping CIN just a bit harder can make cancer cells so stressed they commit suicide. Like when your OneDrive glitches and suddenly everything freezes—except a little coding in the gene world could trigger the same.
Gleevec’s Hidden Lesson—Targeting The Chromosome Rulebreakers
We’ve seen it before. Take Gleevec—the chronic myeloid leukemia wonder drug. Officially, it hit the “Philadelphia chromosome” proteins. But really, Gleevec nailed the 9-22 fusion, which kept the tumor’s mess under control. That’s the promise researchers are chasing now: chromosome chaos-fueled therapies that can target structural DNA errors—not just isolated gene ones.
What Your Mitochondria Wishes You’d Know
Look, your mitochondria were not built for drama. They expect smooth sailing. So when chromosome mistakes flood with protein imbalances, they literally say—“I’m shutting down.” But weird twist: not all humans react the same. Some tumors adapt. Others die. Which means—drugs that target mitochondria might work better in some people than others. That’s the frontier now: matching chaos traits to mitochondrial weaknesses drug-wise.
Hoping vs. Knowing—Why Merging Science Doesn’t Fit in Textbooks Yet
Confession: we’re still in the “what if” stage. Chromosomal instability research dances between incredible potential and, well, practical roadblocks. We’ve uncovered so much that it’s feverishly frustrating to not apply it yet. Here’s what patient’s hope calm but factual science translates to… soon.
Open Questions – 5 Big Ones
- Is CIN leverageable in all cancers? Or just some?
- Why do some tumors adapt better to gene instability?
- Will protein imbalance monitoring in blood predict recurrence?
- Can we safely increase mitochondrial stress without harming normal cells?
- What tissue types are most vulnerable to chromosome numbers going haywire?
Chromosomal Research: A Marathon, Not a Sprint
The takeaway? Chromosome imbalances cancer isn’t just a minor geek niche. The way tumors shake up DNA could be the best way to beat drug resistance, refine treatments, or even predict which tumors might respond and which won’t. Some early trials (still in progress) are showing that driving up CIN can boost immune response in certain breast cancers—meaning your body naturally revs up to attack the glitch.
Bottom line? Some of the toughest buzz today lies in balancing that “just right” amount of instability. Too much? The cells die—but then so does your approach. Too little? No interest in pushing them toward collapse. But with all the private credit hanging around broad genetic screens, this kind of research isn’t evaporating anytime soon.
Final Thought: The Beauty of the Chromosomal Mystery
When Theodor Boveri first floated the idea of chromosomal damage in cancer, it was 1902. 120+ years later, some of us still didn’t know if it was obsession or coincidence. Now? We’re chasing real-world answers. Aneuploidy in cancer cells? It’s not just a symptom. It’s a teammate. A bully. A double agent. But now that scientists are watching that DNA dance more closely than ever, we might finally be holding … not all the cards, but a heck of a poker hand.
So next time your family asks why mitochondria matter? Or why any of this DNA play matters—you have a new story to tell. Because we’re not just fighting cancer now. We’re learning how tumors use their own DNA against themselves. And we’re starting to flip that script. Maybe tomorrow, we’ll outplay them for good.
Got questions? Hit me in the comments. Or if you’re studying this somewhere? Tell me your war stories. We’re all in this together, yeah?





















Leave a Reply
You must be logged in to post a comment.