If you’re Gen X or younger, this one hits close to home. The American Cancer Society dropped a 2025 report with a chilling stat: women under 50 are now 82% more likely to be diagnosed with cancer than their male peers—up from 51% in 2002. And it’s not just a US problem. Global models predict a 30% surge in early-onset cancers (cases under 50) by 2030. This isn’t abstract. It’s here. Now. So what’s going on, and—more importantly—what can you do about it?
Rising cancer rates in young adults aren’t just about numbers. They’re about friends, like Charisma McDuffie, who got the breast cancer “survivorship” stamp at 28. About Ryan O’Grady, a healthy 43-year-old math professor, who thought his stomach pain was “just stress” until a colonoscopy changed everything. And about you and me. Because age? It’s not a vaccine. Gen X and millennials are living through a quiet storm in cancer risk—and the solutions? They’re simpler than you might think.
Alarming? Yeah. But Let’s Break This Down.
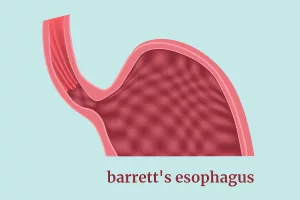
This trend isn’t random—it’s specific. The NIH tracked 33 cancer types from 2010-2019: 14 saw a rise in under-50s. Breast, colorectal, uterine, and pancreatic cancers dominate the list. But here’s the kicker: some cancers like lung and prostate are actually dropping in this age group. So why’s it feel so scary? Because the ones climbing are…
Let’s talk numbers. The David-101 wasn’t written for healthcare jargon.
What Happens if You’re Gen X or Millennial?
Here’s the cold truth: women under 50 now face 82% higher cancer rates than men of the same age. For Gen Xers (born 1965-1980) and millennials (1981-1996), this black-and-white trend line? It’s pink. Colorectal, breast, uterine… these cancers are crashing into our generation like a rogue tidal wave. Ever delayed a doctor’s visit because you thought you were “too young”? So did Ryan O’Grady when his belly pain showed up. It didn’t matter he was 43 and rockclimbing on weekends. Turns out, cancer doesn’t read demographic spreadsheets.
Why Is This Trend a Red Flag for Public Health?
Think of cancer like weeds in a garden. Some we suppress (childhood cancers are declining). Others are mutating—growing stronger in younger soil.
NIH’s 2025 research found colorectal cancer now kills young adults more than any other cancer—surpassing even car accidents for 30-39-year-olds. But here’s the twist: deaths from some early-onset cancers aren’t rocketing (yet). Uterine cancer survival rates dropped—84% for white women, 63% for Black women. Pancreatic? Downright terrifying. Mortality may not mirror diagnosis spikes yet, but biologically, the path is clear: structural shifts in our lives are brewing storms in our bodies. The next question isn’t if we’ve hit a tipping point. It’s how to steer the ship.
| Cancer Type | Annual Increase in Under-50s | 5-Year Survival Disparities (by race) |
|---|---|---|
| Colorectal | 1-2% | 81% (white), 63% (Black) |
| Breast | 18% equity gap in overall cases | Triple-negative in young women: 77% |
| Uterine | 1% annual growth | 84% (white), 63% (Black) |
So… What’s Making Us Sink?
Obesity’s the obvious Darth Vader here. Because inflammation isn’t just for sprained ankles anymore. Dr. Shari Goldfarb from Memorial Sloan Kettering puts it plain: fat tissue screams “GROW” across dozens of cancer pathways. But let’s not stop there. I’ve got a bet to place with my 30-year-old self’s breakfast choices.
Is Obesity the Biggest Villain in This Story?
Picture your cells as grumpy neighbors. Obesity doesn’t just crowd them—it turns their block parties into all-night ragers. Stress, body weight, processed meat… it’s a package deal. Duke Health researchers blame extra estrogen from fat cells for the 1% annual uptick in uterine cancers, especially among non-white women. The body’s not a jukebox—it’s a playlist. And if you’ve got two decades of processed dinners, sitting is the lead single.
What Else Might Be Hiding in Plain Sight?
We’ve got Colorectal cancer rates spiking like a horror movie jump scare. And no, it’s not just burgers. “Ultraprocessed foods are social media for your gut microbiome—addictive, but grossing things out,” Dr. Kimmie Ng from Dana-Farber shared. Other suspects:
- Microplastics in bottles and takeout containers
- Stress—like career escalators and mortgage payments
- HPV-driven oral cancers (especially vulnerable: women born between 1980-2000)
This isn’t Chicken Little stuff. It’s a data-driven Jumanji game—and we need players who understand the rules now. Because the risks are real. Our rewards? Bodyweight management, weekend jogs, and rethinking budget dinner staples. Let’s score this risk factor checklist…
Risk Factor Reality Check
Grab your red pen:
- 3+ alcoholic drinks weekly? Guilty. Next: trade in the margaritas. Even the occasional hangover could speed things up.
- Ultra-processed meals >4 times/week? Guilty, we’re all guilty. But think of it like car insurance—small deductions now avoid system collapse later.
- Tracking family cancer history? GPs we talk to say this is the secret weapon for early cancer detection. Do you know who had what in your family tree?
The Warhol Effect: Why the “Top 4” Are Now Bottom 18
Breast cancer headlines grab hearts. But look closer. Of the 14 cancer increases, four currently dominate emergency rooms.
Why Are Breast and Colorectal Hitting Millennials Hardest?
All right, truth time. Breast and colorectal cancers aren’t playing by the old rules. The NIH tallied 4,800 extra breast cancer cases in under-50s by 2019. And turtles aren’t the only ones going out of order—colorectal cancer incidence jumped 2,100 additional young diagnoses. This isn’t a name change; it’s a redesign of the whole model. Dr. Nancy You from UChicago Medicine calls it the “pre-midlife crisis.” Because at 35, who’s counting polyps or worrying about “dense tissue”? Not anyone I know. Not until their best friend looks exhausted from chemo.
What’s Behind the Uterine Cancer Comeback Tour?
Picture this: your body’s got a built-in surveillance team. But obesity? It’s like hiring a new intern who keeps missing the memo. Cancer incidence statistics show more than 1,200 extra uterine cases in 2019. And those numbers aren’t isolated to “flu season.” Black women? Their bodies often fight two battles: excess weight and unequal access to care. It’s not that they’ve got weaker immune systems. It’s that the entire playing field’s been tilted.
Your Action Plan: Not Another Hippie Health Wave
This isn’t a TikTok fad. It’s a survival wheel. Because early cancer detection? It’s not just for folks with 401k funds. It’s for all of us. Here’s the game plan.
Can Tiny Lifestyle Changes Dent These Rising Rates?
Let’s get practical. Dr. Goldfarb’s patients ask, “I ate kale—why did I still get cancer?” Her answer? There’s no reward for being a Law & Order fan. Prevention’s about fatality over perfection. Try these four permissions:
- Kick one processed food habit. From frozen pizzas to chili in a can—baby steps turn into bodyguard steps.
- Crank up your moving time. Not a gym rat? Walk your dog extra blocks. Park 10 minutes less convenient. Let being “bad at yoga” become “okay at surviving.”
- Check family cancer data. Ever wondered if “Grandma’s breast cancer made the gene lottery suspect”? Time to Google your family reunions.
When Should You Copy 60-Year-Old Screening Guidelines?
Pro Tip: Talkatives who were, “I avoid doctors but trust my curling iron’s burn marks?” Nah. Yale Medicine doctors rally a “when in doubt, screen it out” approach. Back in 2000, mammograms started at 40. Now? Guidelines in some states say 35. Not because rules get looser. Because the data got harder to ignore.
Dealing with Cancer in a Too-Young-to-Be-Old Body
Colorectal cancer in a 28-year-old? That’s not a typo. It’s Ryan O’Grady’s story. After his Disney World gut pain—ignored for 15 months—he joined the 2,100 under-50 colorectal cancer wave. “I thought maybe my gluten intake,” he said. Turned out? Aggressive, fast-moving tumors that didn’t care about low-carb diets.
Are Cancers in Young Adults More Aggressive?
Cancer in youth isn’t the kind that politely arrives with senior discounts. Yale’s Dr. Mariya Rozenblit argues young breast cancer patients often battle triple-negative variants, which sprint through cells like rogue quarterbacks. Treatments? Heavier. Outcomes? Complicated.
When Do Symptoms Become Legit Changes?
Ryan’s story should’ve turned on alarm bells at 38—not 43. He had persistent pain, unexplained weight loss. What did he blame? Travel fatigue. Stress. But ACS’s 2024 book says this delay’s not uncommon in under-50s. Because who’m I calling with this info? Friends in their 30s? Nope. This belongs in your next doc chat. Don’t know where to start? Pick your symptoms.
Fighting the “Wait-Until-You’re-Older” System
Imagine a world where your doctor goes, “Hmm, maybe get a colonoscopy.” Basic, right? Wrong. More than your coworkers dismissing stomach aches as “too much pizza.” Many win exams if you push—and prove family history or symptoms compile too much data to ignore. But here’s the good: more programs like MSK’s $350 million Young Adult Pavilion focus on Eartha Kitt’s generation, not just Frank Langella’s.
Why’s the Medical Community Playing Catch-Up?
Short answer: habits in healthcare lag behind research J curves. Longer answer? Old guidelines won’t end up in 2025’s ERs where millennials check in with colon pain. Take action. Use phrases like, “can we reassess my screening age?” Sometimes the system works—but you’ve gotta pry cracks in it first.
Vaccines and Screenings You Can’t Afford to Skip
If your GP’s underestimating prevent today’s risks, you need two tools in 2025:
- HPV Vaccine – Not just for teens. Docs now push it even if you’re 30 and HPV-negative.
- Colonoscopies – Guidelines lifted from 50->45 in 2020. Plot twist: If your aunt had precancer at 48? Ask for pre-45.
Is Your Environment Hemorrhaging Cancer Risk?
We’ve got 2025 water that contains microplastics like “vegetable soup.” And air pollution rooting in cities. Recent Dana-Farber models project 40% of young adults worry about these invisible exposures. But let’s break down how to combat them without turning into a prepper.
Are Microplastics and Pollution Silent Culprits?
Back to gut microbiome popcorn-type analogies. Because your intestines aren’t ECUAR pop-ups. They’re more like 15-year loans with runoff effects. According to the PROSPECT study, dietary changes (hello, home cooking) reduce colorectal risks 18%, even for those with polluted ZIP codes.
Racial and Income Gaps: Cancer’s Inequality Nightmare
There’s a human issue within these trends—you can’t just “exercise more” if gyms are 30 miles away and you’re trying to survive 50+-hour workweeks. Duke Health didn’t mince words: uterine cancer death disparities mirror societal health equity failures. Black women’s 63% 5-year survival isn’t biological weakness—it’s a system not prioritizing their concerns.
Why Do Marginalized Communities Stay at Higher Risk?
It’s not just access. Think about how many fams from lower-income neighborhoods hear stuff like, “That’s just the way the cookie crumbles,” instead of, “Why are our parks rotting?” Major, NIH’s 2025 report showed that Black women’s cervical cancer rates aren’t genes—it’s unequal access to Pap smears and HPV vaccines. Solution? Not just “educate patients,” but “tackle data gaps.”
Predictions, Not Doomscrolling
Let me leave you with something actionable. Callapsing your risk factors doesn’t mean quitting your job to hike Machu Picchu daily. But NCI’s pharmacologic trials promise better blood draw detection for early cancers by 2027. MSK isn’t just doing research. They’re building a whole hospital wing devoted to this demographic invasion. So what’s your part in this timeline? One tiny win. Today.
What’s the Roadmap for Cutting Early-Onset Rise?
Four tracks ahead:
- Preventing environmental crack-ins (microplastics, urban smog)
- Fine-tuning screening rules (your dog activity’s not triggering colonoscopies at age 40 as of 2025)
- Clipping risk factor spikes (obesity, processed playlists on Netflix Food Network)
- Opening clinics like Yale’s for early cancer planning (genetic flags, symptom charts, TGPUs if you need them)
TGPS: Type-A puns aside, Triple-Negative Prevention Units (yes, docs use that term now). Know your screenings. Start one pain point with small wins.
Conclusion: You’re the Feature, Not the Bug
Rising cancer rates aren’t inevitable. They’re warning labels—but for entire generations. When Duke’s data showed uterine cancers worsening, or the NIH noted 4,800 anal diabetes Ms. Charisma hates the word “health sprint.” But here’s the deal:
This isn’t about perfection. It’s about spotting symptoms before they become life-sized models. About having one scan before your 39th birthday to dodge Ryan’s calendar surprises. You’ve got the power—hell, the scientists even blamed poor screening adherence over the 2,100 extra colorectal cases. But it starts with one change. A better snack. A slower breath through traffic lights. A scary question typed into WebMD when midnight strikes.
And if you’re wondering how to talk to your GP about this? Save this article. Print something. Visit—even if you feel like a bother. Gen X and millennials didn’t choose this curveball. But we can choose how to swing back.
So tell me: When’s the last time you asked your doctor “Do I need to be screened early based on my family?” Meditate on that. Maybe tomorrow.






















Leave a Reply
You must be logged in to post a comment.