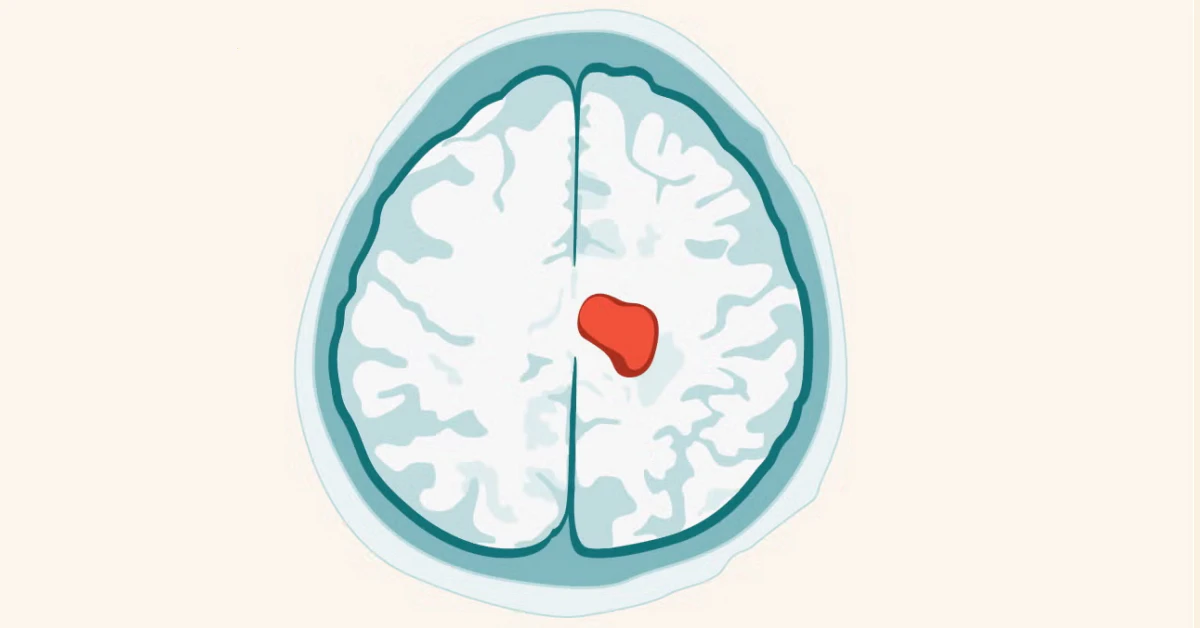
Okay, let me break this down like I’m explaining it to a friend. You’ve got a brain tumor? Suddenly, the first question isn’t just about treatment—it’s, “How the heck is this thing behaving?” Here’s the straight truth: tumors don’t all grow the same way. Some expand like balloons pressing against your brain (awful, right?), while others dig in like invasive weeds. And yeah, both can be life-changing. The tricky part? Understanding which path your tumor might take could mean the difference between catching it early or scrambling to keep up. Let’s unpack this.
Understanding Tumor Behavior
This isn’t a “one-size-fits-all” situation. When doctors talk about brain tumor growth, they’re watching a movie, not a still image. Will the tumor slowly squeeze? Or will it send feelers into parts of your brain, refusing to behave? Here’s what you need to know.
What Does Brain Tumor Growth Actually Look Like?
Imagine a slow, sneaky balloon inflating in a tight space like your skull. That’s non-invasive, pressure-based growth. It’s not harmless—it can crush nerves, squish healthy tissue, and mess with your brain’s “WIFI signal”—how it communicates. But treatment might buy you time here. Now picture invasive growth. Those tumors spread root-like structures, infiltrating quietly until… BAM. Seizures, speech trouble, or weakness pop up like a horror movie jump scare. Even the smartest scanners can miss these until they’ve embedded. Why does this matter? Because how a tumor grows drives every decision your care team makes. Stanford’s neuro-oncology team has seen both patterns up close, and they’ll tell you: location + behavior = not just symptoms but your care roadmap.
Can A Tumor Change Gears from Slow to Aggressive?
You bet it can. Remember IDH mutations? Think of them as a faulty cruise control setting. Early-stage gliomas might lob around at “low speed” while hiding rogue growth signals. But at some point, like a rogue software update, they flip switch and go full grade 4. Broad Institute researchers call this the “ticking time bomb”—those cells suddenly evolve, acquire new mutations, and shed their docile masks. If your doctor mentions “genetic profiling,” they’re not just showing off. They’re predicting whether your tumor’s about to shift character. That’s why treatments like vorasidenib target IDH early—it’s like defusing the timer.
Beyond the ‘Scan and See’ Mindset
How Do Tumors Hide for Years?
This one kills people softly. Benign tumors like meningiomas often grow so slowly, they become part of your brain’s furniture. Duke Tisch Center’s studies show some patients live for years before symptoms like subtle memory gaps or random headaches tip them off. For invasive tumors, think of cancer cells as stealthy ninjas—they’ll probe brain highways silently until they’re entrenched. The hard truth? Your brain ain’t wired with pain sensors. So a tumor can set up camp for what feels like foreveruntil you trip over a symptom that ordinary medication can’t fix.
Should We All Rush for Brain Scans?
Short answer: Nah. These silent tumors are rare, but let’s talk red flags—consistent visual disturbances, unexplained seizure debuts around age 30, constant nausea. If scans uncover a slowpoke tumor, your care team might say, “Let’s watch it dance…” instead of diving into 90’s chaos. The NHS suggests checking symptoms you can’t ignore, but let’s be real: if you’re Googling “brain tumor growth symptoms,” you’re probably wondering if it’s time to call the doc. Pro tip? Document those weird one-off episodes. Your diligence might save a neurosurgeon 10 years in the future.
What Fuels the Shift to Aggressive Growth?
Some tumors are programmed to morph. IDH mutations open the door, but invading normally calm tumors? They’re breaking rules now. Radiation might be part of the “how”—UCLA’s recent work shows that treatment like forskolin (PNAS Forskolin Study) plus radiation doesn’t just kill cancer cells—it can force them to “become something else.” But not all triggers come from outside. Stress, immune system shifts… even your body’s own chemistry might push these tumors faster into dangerous territory. Cleveland Clinic doctors don’t sugarcoat it: genetics stack, environment layers, and sooner or later—the IVB drip becomes a critical care unit. But have hope. This isn’t a life sentence; it’s a reason to build a better game plan.
Invasive vs. Non-Invasive: Cheating the Game
Why Invasive Tumors Are Medical Headaches
Non-invasive? Think of them like benign “dumbbells” you might lift surgically. Invasive, though? Those things act like malware. No part of your brain is safe when they turn invasive. Johns Hopkins breaks it down: non-invasive tumors often behave, while invasive ones refuse to follow menus—notorious for returning even after surgery. And guess what? They’re tougher than grandma’s meatloaf to treat with radiation or chemo. Why? Their roots go where scalpels and therapies can’t reach safely. That’s why research into tumor “identity switches” at Broad Institute matters—it could buy time.
Brain Tumor Growth Paths: Two Roads Diverged
| Growth Pattern | How It Plays Out | Treatment Challenges |
|---|---|---|
| Non-Invasive | Balloons press against tissue. Symptoms like chronic headaches, blurry vision, personality changes come earlier | Removal is surgery-center open road. Recurrence? Not guaranteed |
| Invasive | Roots spread quietly. Symptoms like seizures, focal neurological issues show up late | Difficult to excise fully. Often rebounds quicker. Radiation & “identity switch” drugs under study |
Tumor Location: The Neighborhood Matters
Your tumor’s address dictates everything. Grow near the brain’s busy crossroads? Even benign ones can drop house size bombs on your quality of life. Grow in a sleepy cerebral suburb? You might not notice for ages. Example? Mayo Clinic warns that acoustic neuromas, even benign, often start as hearing loss or balance quirks—years before anyone thinks, “Is this a tumor?” Location plays chess, not checkers, with your diagnosis timeline.
Real People, Real Stories
Maria’s Story: The Tumor That Refused to Bother Her
Maria was 32 before her “benign tumor” made itself known. It grew near her frontal lobe’s “backyard,” letting her off with mood swings and fog for nearly seven years. Her doctor joked, “This thing was hiding in plain sight…” An MRI finally caught it wrapping around a blood vessel. Because it wasn’t sending invasive feelers, they couldn’t wait over a year until it grew spine-like roots downtown. Her story? Early symptoms can ghost you—until location + growth makes you question everything.
Dave’s Dilemma: When the ‘Harmless’ Went Rogue
Dave had a low-grade astrocytoma. No big deal, right? Then he started having leg weakness at 40. The WHO’s grading system said grade 2, no rush. But slow “progress” turned into aggressive infiltration—grade 4 status with symptoms racing. His treatment team at Cleveland Clinic discovered the shift happened as his tumor cells invaded where they hadn’t before. Bottom line? Dave’s case shows how watch-and-wait isn’t always safe unless you’ve got regular scans.
Keeping Upgrades Under Control
How Do Doctors Test for Tumor Upgrades?
MRI’s the MVP here, but they’ve got secondary tech like functional brain scans and diffusion studies. Your neurologist might pop a Ki-67 test into the mix—this little test points out how much your tumor’s dividing fast. Sometimes they use genomics, dissecting mutation changes. The takeaway? Tracking growth isn’t a guessing game anymore. UCLA Health says, “Don’t wait—it might cost 20% on your life expectancy…”
Do Tumors Respond to Treatment Differently?
Like a chameleon in treatment. Aggressive ones hit your team with issues—some cells go “dormant”, hiding from radiation. Others evolve, kind of like “resistance superheroes.” The Tisch Brain Tumor Center’s current strategy involves combining therapies so tumors can’t game the system. One patient, Laura, shared how this kept her tumor stable for months where previous treatments failed. Her words: “No one wants to play cat and mouse with brain cancer, you know?” Treatment personalization isn’t hot air—it’s the real deal.
What Role Do Biomarkers Play?
No soapbox talk here—just facts. Biomarkers are like your tumor’s party DJ. They set the pace for growth. UCLA’s research found biomarker-driven strategies reprogram these tumor tracks. Their study (grab it via PNAS) took pre-clinical mice and manipulated growth markers—the knock-on effect? Tumors didn’t just sit still; they became less aggressive. Your doctor might discuss MGMT, EGFR, or IDH status like menu options. It’s not jargon—those markers guide your care cocktail.
Lifestyle, Care, and Late-Stage Twists
Can Lifestyle Choices Influence Tumor Evolution?
Here’s the catch. There’s no “cure” with kale and meditation. But stress does strange things. If you’re worried about progress, take the reins wherever you can. Avoid skip-day-for-chemo stress. Build strong immunity—support systems matter if your body’s fighting genetic switches. Check out what Broad’s scientists say about stress and mutations. Yeah, it’s complicated—but steering clear of added strain can’t hurt.
How Does Growth Affect End-of-Life Planning?
Nobody said this part was easy. For tumors that refuse to sit still, palliative care becomes essential. Discuss what’s next with your family, your team. Some focus on treatment “extension,” while others turn to quality of life strategies. Broad Institute discusses location-based progress and issues like “Grade 4 glioblastoma survival’s around 15–18 months…” Kinda brutal, but real decisions happen with that info. Choose care that fits—whether it’s match-the-biomarkers chemo or the “soft landing” approach.
Partnering With Your Care Team
What Questions Snap Crackle Pop
- “Is my tumor non-invasive or aggressive?” Check diagnostics ASAP.
- “Could our family history explain this rogue biology?” Open the floor—maybe you’ve got a hereditary factor.
- “How often should I scan for progression?” Don’t wait till you trip on sewage lines of seizure.
- “Are my current symptoms tied to tumor growth?” Plain communication keeps surprises small.
Start here. These aren’t nosy—they’re the questions your Cleveland Clinic or Mayo Clinic team expect you to ask. And you should. Don’t leave your future on uncertainty’s doorstep.
When Do You Need a Second Opinion?
If your team drops a “just watch it” approach thickly cloaked in uncertainty—especially with growth patterns emerging—consider a second opinion. Like shopping around for a mechanic you trust, but for your brain. Not a questioning of your doctor’s skills (probably not), more like having extra eyes on your tumor. At the same time, plenty of patients at Stanford have caught unnoticed issues during second opinions. In some cases, a new biomarker focus is all it takes. Never feel alone.
Make Your Next Move
Your journey with a brain tumor starts with understanding its habits, but ends with action. Whether tumors push, spread, or leave bad dreams in their wake, your care team will sculpt your approach, treatment by treatment. Keep asking—and don’t stop reading. Brain tumor care is evolving faster than last year’s iPhone, and knowledge is your superpower. Got questions? Find someone to chat—they’ve got answers long paths forged by clinics like Mayo and Tisch.





















Leave a Reply
You must be logged in to post a comment.