Let’s Start With That Gut Drop
Oh, you know the feeling. That jumpy heartbeat when you’re waiting in that weirdly silent exam room…the crinkle of the paper sheet beneath you…your brain cycling through what-ifs faster than an out-of-control washing machine. Then, the words: HER2-positive breast cancer. Your world tilts. You hear “aggressive.” You hear “spreads fast.” Your mind quietly asks, “Is HER2-positive breast cancer a death sentence?”
I get it. It’s the kind of worry that makes your stomach knot up, like when you forget your wallet at the checkout—only, you know, times a hundred. If you’re here, it’s probably because you—or someone you love—is facing this diagnosis. Maybe you Googled late at night, not ready to talk to anyone yet. Maybe you just want some hope, or honestly—just honesty. So let’s have it. No sugar-coating, but zero gloom-and-doom, either.

Why This Diagnosis Hits So Hard
HER2-Positive “Back Then”: Was It Really a Death Sentence?
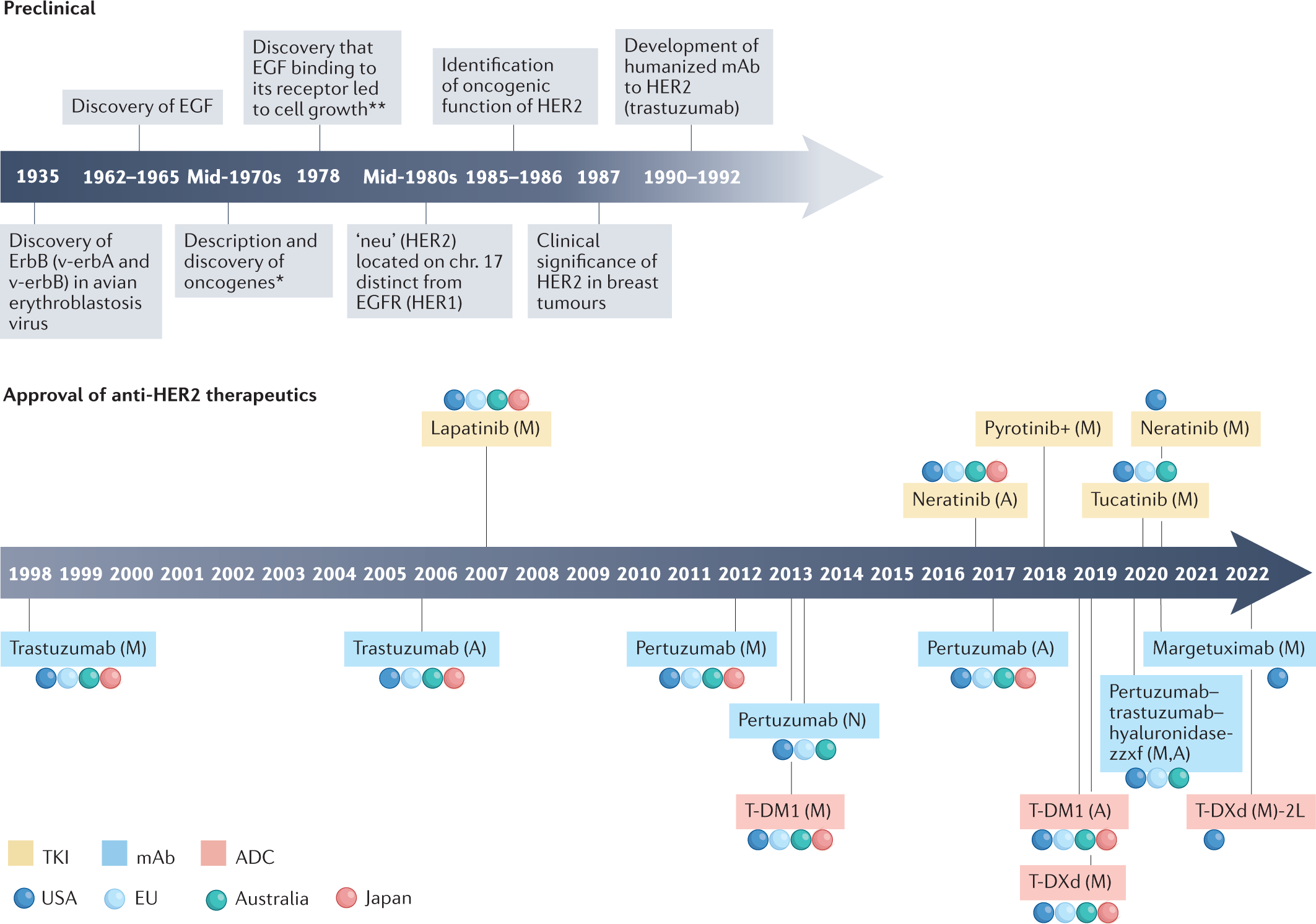
I’m not going to lie: decades ago, a HER2-positive breast cancer diagnosis was sort of dreaded. Doctors, and patients too, would brace themselves for the worst. (Heck, my friend’s aunt—let’s call her Maribel—still tells the story of her late ’90s diagnosis with a shudder. There just weren’t as many options back then, and people knew it.) Back then, HER2-positive breast cancer meant about 20% of breast cancer cases…but it was the fast-moving, pain-in-the-butt kind. It liked to travel, and the tools doctors had seemed basic compared to today.
But over the past 20+ years? Wow. Treatment has transformed. New meds, new strategies—patients who once would’ve heard “fatal” now hear “treatable.” Some even hear “potentially curable”, for real. Not kidding. Advances moved us to a whole new place. Read this Longest HER2 breast cancer survivor story if you need a pick-me-up right this second.
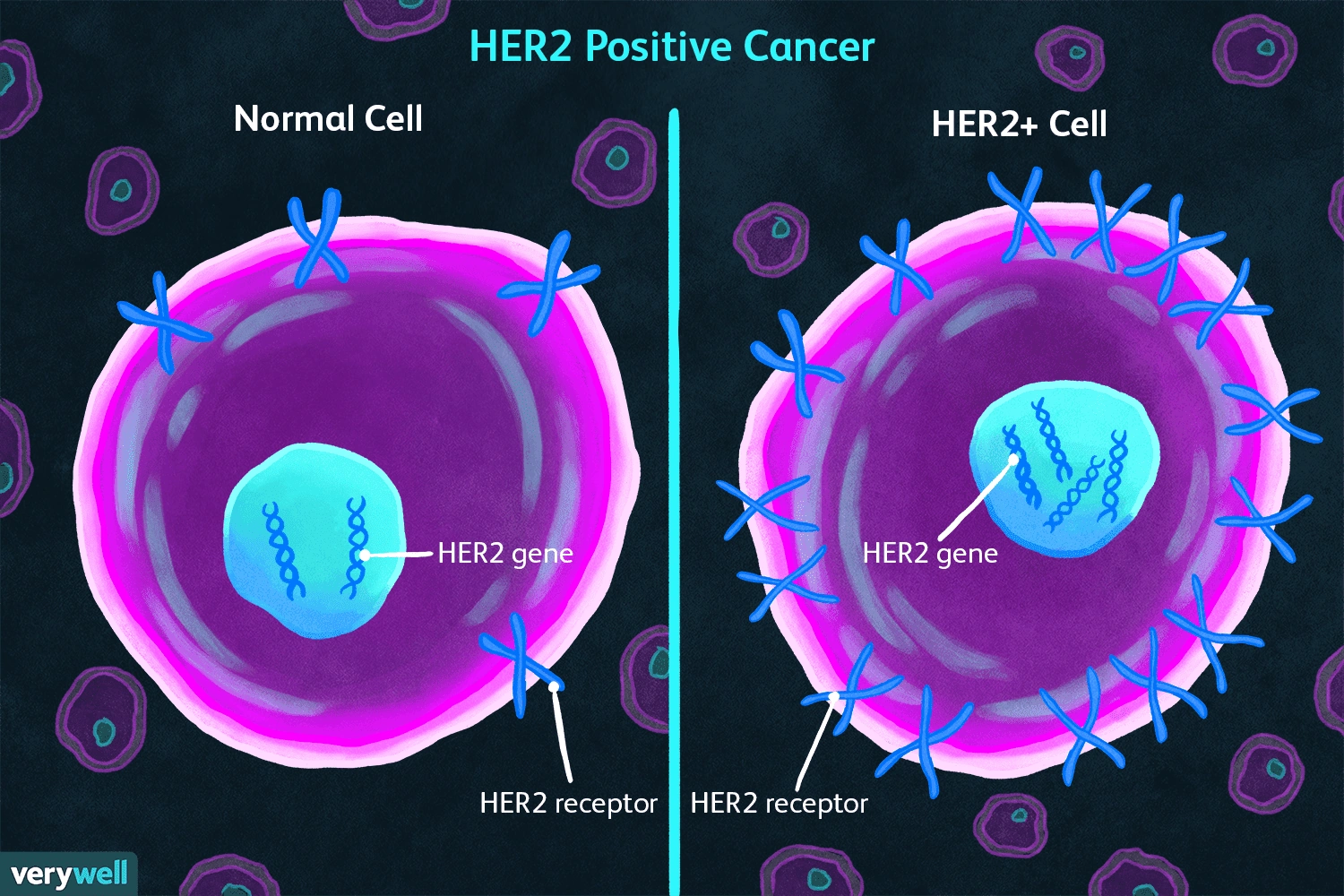
HER2 — Not Just Four Letters, But a Sticky Protein (Let Me Explain!)
So what is HER2 anyway? It’s a protein. Human epidermal growth factor receptor 2. (Mouthful, right?) Its job is to help cells grow. But if you’ve got too much of it…your cells act like they’ve downed five energy drinks—growing, dividing, and refusing to stop. That’s why HER2-positive cancers usually spread faster. Still, knowing your HER2 status helps doctors pick the best “smart bombs” for treatment. Just finding out is the first step to fighting it ruthlessly and, honestly, more intelligently than ever before.
Survival Rates: Hope Hiding in the Fine Print?
Okay, Is HER2-Positive Breast Cancer a Death Sentence or Not?
Let’s say it loud: Today, HER2-positive breast cancer is NOT a death sentence. The numbers—actual research—back this up. If you catch it early (before it’s decided to go sightseeing in your lungs or bones), survival rates are over 90% when people get that killer blend of chemo and targeted antibody “smart drugs”. The medical name-dropping here is trastuzumab and pertuzumab, but think of them as your personal bouncers. Get diagnosed early, get those meds, and suddenly, you’re in a way better place than anyone was in the ’90s or even early 2000s.
And what about those “oh no, it spread” times? Guess what? Even with late-stage, treatments are helping people live longer—years, not just months—sometimes managing it like a chronic thing, not an emergency. If you want the details, stats, stories: check out HER2 breast cancer life expectancy. It’s proof that things are still changing in a good way.
Quick Table – Survival, Then vs. Now:
| Era | Outlook | Main Game-Changer |
|---|---|---|
| Pre-2000s | 2–3 years (avg late stage) | No targeted options |
| Now | 90%+ survival (early stage) | HER2 blockers, better combo meds |
So if anyone tries to tell you HER2-positive = automatic “bad news,” you can gently nudge them toward these stats. Science doesn’t mess around.
But Wait…What About My Specific Case?
Here’s the thing—prognosis is personal. Doctors look at stage (how much it’s spread), grade (how “wild” the cells look), tumor size, whether hormone receptors are present, and yes, your own health vibes. That’s why survival stats are averages—not rules. (In real life, I once met a woman who celebrated her 10th “cancerversary” at a bakery near my old apartment. She said, “Statistics never included my attitude—and I’m stubborn!”) But yes, if your tumor is tiny, hasn’t crashed any lymph node parties, and you tackle it early, your odds rock. Larger or higher-grade? It needs more aggressive tools, but still: that doesn’t mean a death sentence.
And even with low-grade, node-negative HER2-positive tumors (which, weirdly, sometimes act sneakier), today’s focus on careful testing plus “smart drugs” is changing survival odds there too. It’s complex…but fair to say: “not a death sentence” has become the rule, not the exception based on expert guide info.
The Treatments: Old School vs. The New Class
Chemo, Antibodies, “Smart Drugs”—What’s Actually Happening in There?
Let’s geek out for a second (don’t worry, I’ll make it clear). Twenty-five years ago, it was chemo…full stop. Now? It’s chemo plus HER2-busting antibodies and targeted medicines. First came trastuzumab (Herceptin). Hugely impactful—suddenly, people who’d been told to “get their affairs in order” were hearing things like “stable,” “remission,” or even “no evidence of disease.” Who knew a monoclonal antibody could sound so romantic?
Then you get pertuzumab, and newer “conjugate” meds like T-DXd, which basically attaches chemo directly to the antibody, delivering a punch much more precisely. There are even oral therapies (TKIs like lapatinib) for cases where, well, things like to change things up. The combo approach is strong enough that in some recent trials, people stopped meds and STILL stayed cancer-free for months, sometimes longer. (Can we just have a round of applause for medical research?)
Real Talk—How This Feels in Real Life
If you hang out in cancer circles, you’ll hear stories everywhere. Yvonne’s is one: she was diagnosed with metastatic HER2-positive disease, which had spread to basically half her organs. She started that combo therapy—yes, the “infusions become a part of life” thing—but guess what? Tumors shrank to 3% and didn’t come back. She’s not alone. For every scary stat you read, there’s a person whose results blow old expectations out of the water. Don’t believe me? Just read a few testimonials on Longest HER2 breast cancer survivor—these real humans are living, laughing, and definitely not following old “prognosis” rules.
Living With HER2-Positive: It’s a Whole Vibe
This isn’t just about survival, either. Quality of life matters. Plenty of folks, even with metastatic cancer, are busy—raising kids, hiking, traveling, learning how to Zumba. (My neighbor went from diagnosis to Pilates instructor in three years. She claims her “superpower” is out-dancing the odds. Insert friendly eye-roll here.) For earlier stages, many go back to their routines after active treatment—work, family, whatever makes your heart beat.
Stories Change Everything
Why Real Stories Matter (And How They Give Hope)
Let’s be honest, most of us aren’t inspired by textbooks. We’re inspired by the person who stands up and says, “Yes, I had stage 4 HER2-positive cancer and here’s how I’m still here.” The Longest HER2 breast cancer survivor page is bookmarked on my phone, not for stats, but for hope (and okay, sometimes for perspective when I’m having One Of Those Days). Their stories make the stats feel like a challenge, not a threat.
And don’t sleep on support groups, fitness clubs, or yoga studios—so many survivors show up to mentor newbies on how to eat, exercise, and laugh through tough days. The way HER2 is managed now, you’re not alone, you’re in pretty fierce company.
Quick Comparison – Then vs. Now
| Decade | What People Heard | Reality Now |
|---|---|---|
| 1990s | “Aggressive, two years tops” | Some folks now thriving 10, 15+ years out |
| 2020s | “Tough…but treatable” | 90% survival possible early; many with mets living life |
What About Wellness, Health, and Real-Life Moves?
Is Fitness Still Part of the Picture?
Absolutely. Plenty of women (and men!) use exercise, food tweaks, and self-care as power tools in their arsenal. Maybe you decide to walk, run, try barre classes…even just stretching on a tough day counts. Wellness is more than a buzzword; it’s a way to nudge your mental and physical health upward, bit by bit. (Tip from cancer yoga circle: “If you can breathe, you can do this class.” Someone always brings snacks too, which helps…a lot.)
No, You Don’t Need to Be a Superhero
You’ll have days when you want to sleep, days when you want to scream, days when you want to eat cake in the car. (Been there, more than once.) That’s normal. There’s no “right way” to fight. Your story matters regardless of whether you climb a mountain or climb into a blanket fort. Leverage what helps—you’ve got options, and you’re not on a clock.

Want more encouragement and numbers? Check out HER2 breast cancer life expectancy for a realistic, up-to-date look at what’s ahead. It makes a difference when you see facts that match what real people are living.
So…Is HER2-Positive Breast Cancer a Death Sentence? Let’s End With the Truth
The old image—HER2-positive equals fatal—is outdated. Seriously. Modern science teamed up with unstoppable survivor spirit, and suddenly, that “sentence” became just one chapter in a much bigger book. Early, aggressive, or somewhere in-between, today’s HER2-positive breast cancer is treatable, manageable, and—sometimes—beatable. Even cases that once looked dire now come with a plan, a timeline, and, for many, a second act.
If you just got the diagnosis: Take a beat, ask questions, and gather your loved ones. Read other people’s stories. Let yourself be mad, sad, or wildly hopeful—whatever. But please, don’t let fear write the ending. Explore more about HER2 breast cancer life expectancy and give yourself the chance to believe in new possibilities. Maybe you’ll even want to share your story someday among the Longest HER2 breast cancer survivor crowd…now, wouldn’t that be something? You’re not alone. You never were.
























Leave a Reply
You must be logged in to post a comment.