Hey there! If you’ve landed on this page, you’re probably wondering, “What exactly is Velcade?” In short, Velcade (generic name bortezomib) is a proteasome‑inhibitor—a targeted cancer drug that works differently from the classic chemotherapy you might have heard about. Knowing the drug’s class helps you understand how it attacks blood‑cancer cells, what side effects to expect, and why doctors choose the dose they do. Let’s dive in together and make sense of this sometimes‑confusing topic.
Quick Answer Overview
Velcade belongs to the proteasome inhibitor family, a subset of antineoplastic agents that block the cell’s protein‑recycling machinery. It’s not a traditional chemotherapy or an immunotherapy; think of it as a “precision strike” that zeroes in on cancer cells while sparing many healthy cells.
| Aspect | Velcade | Traditional Chemotherapy | Immunotherapy |
|---|---|---|---|
| Drug class | Proteasome inhibitor (targeted therapy) | Cytotoxic agents | Checkpoint inhibitors, CAR‑T cells |
| How it works | Blocks proteasomes → protein buildup → cancer‑cell death | Kills rapidly dividing cells (cancer & some healthy) | Boosts immune system to recognize cancer |
| Typical side‑effects | Peripheral neuropathy, fatigue, nausea | Hair loss, nausea, low blood counts | Immune‑related inflammation, infusion reactions |
| Administration | IV or sub‑cutaneous injection | IV, oral, intrathecal | IV infusion, sub‑Q, oral tablets |
According to Drugs.com, Velcade’s unique mechanism makes it especially effective for certain blood cancers while often producing a different side‑effect profile than standard chemo.
How Velcade Works
Imagine a bustling factory inside each cell. Its “recycling center” – the proteasome – breaks down worn‑out proteins so the cell can reuse the pieces. Cancer cells, especially the ones in multiple myeloma, rely on this recycling system more than normal cells because they churn out abnormal proteins at a frantic rate.
Velcade slides into the proteasome like a wrench in a gear, preventing it from doing its job. The resulting protein buildup stresses the cancer cell, ultimately triggering programmed death (apoptosis). Normal cells, which don’t depend on the proteasome as heavily, survive the blockade much better.
Myeloma.org explains the proteasome pathway in a very clear way, noting that when the “trash‑can” is jammed, the cell simply can’t keep up and collapses according to their research. That’s why Velcade is such a powerful tool in the fight against blood‑cancer.
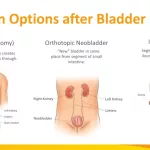
Approved Blood Cancer Uses
Velcade has earned a solid reputation for treating two main blood malignancies:
- Multiple Myeloma – both newly diagnosed patients and those whose disease has relapsed.
- Mantle Cell Lymphoma – especially after at least one prior therapy.
Within these diseases, Velcade can be used in several contexts:
- Induction therapy (the first round of treatment for newly diagnosed patients)
- Stem‑cell‑transplant conditioning (helps shrink the tumor before the transplant)
- Consolidation and maintenance (keeps the disease under control after the heavy‑lifting phases)
- Rescue therapy for relapsed or refractory disease
Oncologists love Velcade because it can be combined with many other agents – dexamethasone, lenalidomide, rituximab, and even traditional chemo – creating a “team” approach that hits the cancer from multiple angles.
Dosage and Administration
Getting the dose right is a balancing act. The standard regimen, as outlined in the FDA label (NDA 021602), is 1.3 mg/m² administered either intravenously (IV) or sub‑cutaneously (SC) twice a week on Days 1, 4, 8, and 11 of a 21‑day cycle. After four doses, patients get a 10‑day rest period before starting the next cycle.
IV vs. Sub‑cutaneous
Both routes are effective, but they have distinct pros and cons that can influence a patient’s choice.
| Factor | IV Injection | Sub‑cutaneous Injection |
|---|---|---|
| Administration time | Quick push (3‑5 seconds) | Longer injection (1‑2 minutes) |
| Injection‑site reactions | Rare | More common (redness, mild pain) |
| Patient comfort | Often done in clinic | Can be self‑administered at home |
| Dose adjustment | Same as SC, but monitor for infusion reactions | May need less pre‑medication |
Many patients prefer the SC route because it reduces clinic visits, but it’s always a good idea to discuss personal preferences with your oncology team.
Adjusting the Dose
Dosage may need to be lowered if you experience:
- Severe peripheral neuropathy (numbness or tingling that doesn’t improve)
- Grade 3‑4 blood‑cell suppression (low platelets or neutrophils)
- Significant liver impairment
- Any life‑threatening reaction such as an allergic response
Never skip a dose without talking to your doctor; dose reductions are often enough to keep you on therapy safely.
Benefits and Risks
Like any powerful medication, Velcade brings a mix of advantages and potential downsides. Let’s break them down so you can weigh the scale yourself.
Common Benefits
- High response rates – many patients achieve at least a partial remission, especially when Velcade is paired with dexamethasone.
- Targeted action – tends to spare many healthy cells, leading to a different side‑effect profile than traditional chemo.
- Versatility – works in first‑line settings, after relapse, and as maintenance.
Typical Side Effects
Most side effects are manageable with medication, dose adjustment, or supportive care:
- Peripheral neuropathy – tingling or burning in the hands/feet; early detection is key.
- Fatigue – common with most cancer treatments.
- Gastrointestinal upset – nausea, vomiting, or diarrhea.
- Blood‑cell changes – low platelets (thrombocytopenia) or neutrophils (neutropenia).
Serious Risks
While rare, some adverse events demand immediate medical attention:
- Severe allergic reactions (hives, swelling of the face or throat).
- Reversible posterior leukoencephalopathy syndrome – sudden headache, visual changes, or seizures.
- Life‑threatening infections related to low blood counts.
- Tumor lysis syndrome – a rapid release of cancer‑cell contents that can strain the kidneys.
Monitoring labs (CBC, liver enzymes) before each dose, and keeping an eye on any new symptoms, helps catch issues early. Your care team will walk you through when to call the clinic.
Real‑World Perspective
It’s one thing to read a textbook; it’s another to hear a story from someone who’s actually been on the journey. Below is an anonymized snapshot from “John,” a 58‑year‑old father diagnosed with multiple myeloma three years ago.
“When my oncologist first mentioned Velcade, I was scared of another “chemo” round. He explained it’s a “targeted drug,” and that gave me hope. The first two weeks felt rough – I had a buzzing sensation in my feet, and my blood counts dropped, so we cut the dose a bit. After the dose adjustment, my neuropathy eased, and by month 4 I saw my M‑protein drop dramatically. I’m now in remission and even give the sub‑Q injection at home on Tuesdays and Fridays. It feels like I’ve got my life back, even if I have to schedule my clinic visits.”
Dr. Elena Ramirez, a board‑certified hematology‑oncologist at a major cancer center, adds, “Velcade’s ability to combine with other agents makes it a cornerstone of modern myeloma therapy. The key is individualized dosing and proactive neuropathy management” (personal communication, 2024).
Clinical trial data reinforce these anecdotes. In the pivotal Phase III trial that led to FDA approval, 38 % of patients achieved a partial response or better, and the median overall survival extended beyond five years for many participants (FDA label).
Talking to Your Doctor
Empowerment starts with the right questions. When you sit down with your oncologist, consider asking:
- “Will I receive Velcade IV or can I self‑inject sub‑cutaneously?”
- “What lab tests will we run before each dose?”
- “How can we prevent or treat neuropathy early?”
- “If I develop a serious side effect, what’s the plan for dose reduction or temporary hold?”
Bring a list of all current medications (including over‑the‑counter and supplements) because Velcade can interact with certain drugs, especially those that affect liver enzymes. Having a clear written plan – when to call, when to come in, and what symptoms are red‑flags – makes the whole experience less daunting.
Wrapping It Up
So, what’s the takeaway? Velcade is a proteasome‑inhibitor, a targeted cancer medicine that blocks a crucial protein‑recycling system inside malignant cells. It’s approved for multiple myeloma and mantle‑cell lymphoma, can be given IV or sub‑cutaneously, and usually follows a 21‑day cycle. While it brings impressive response rates, it also carries side effects—most notably peripheral neuropathy—that need vigilant monitoring.
Understanding the drug type helps you ask smarter questions, spot warning signs early, and collaborate with your care team more effectively. If you’re considering Velcade, talk openly with your oncologist about the benefits, the risks, and how the therapy fits into your overall treatment plan. Together, you can map a path that balances efficacy with quality of life.
Have you or a loved one experienced Velcade? What challenges or successes stood out for you? Share your story in the comments—your experience could be the guide someone else needs. And if any part of this article sparked a question, don’t hesitate to reach out. We’re in this conversation together.





















Leave a Reply
You must be logged in to post a comment.