Ever wondered if a simple spit could tell you whether you’re on the brink of a health issue? It might sound like a sci‑fi plot, but researchers are turning saliva into a crystal‑ball for diseases ranging from gum trouble to cancer. In the next few minutes we’ll unpack what saliva disease markers are, why they matter, and how you can start using this painless tool to stay a step ahead of illness.
What Are Markers
In plain language, saliva disease markers are tiny clues hidden in your spit – proteins, DNA fragments, metabolites, and microbes – that change when your body is fighting an infection, inflamed, or even growing a tumor. Think of them as the “tweets” your body posts, only you can read them with the right lab test.
Unlike blood draws, collecting saliva is as easy as chewing gum. The fluid is a cocktail of hormones, enzymes, antibodies, and microbes, making it a snapshot of both oral and systemic health. A 2021 Frontiers review highlighted that saliva contains “hormones, growth factors, enzymes, antibodies, microbes and their products,” all of which can be harnessed for early disease detection according to the study.
So, why does this matter to you? Because early detection often means simpler treatment, better outcomes, and—let’s be honest—fewer doctor‑office trips.
Major Categories
Scientists usually sort salivary biomarkers into four buckets. Knowing which bucket a marker belongs to helps you understand what it tells about your body.
| Category | Typical Markers | What They Indicate |
|---|---|---|
| Inflammatory Cytokines | IL‑1β, IL‑6, IL‑8 | Acute inflammation, infection, possible tumor activity |
| Enzymes & Tissue‑Remodeling | MMP‑8, TIMP‑1, lysozyme | Periodontal breakdown, bone turnover, wound healing |
| Metabolites & Hormones | Cortisol, glucose, lactate | Stress response, metabolic disorders (e.g., diabetes) |
| Nucleic Acids | cell‑free DNA, miRNA‑21, miRNA‑31 | Genetic mutations, cancer risk, precision‑medicine profiling |
For instance, a 2013 PLOS ONE study found that salivary IL‑8 levels were twice as high in people who had a history of tumor disease, hinting at its utility for cancer screening according to the research.
Clinical Applications
Now that we have a feel for the “what,” let’s explore the “so what.” Below are the most exciting ways clinicians are already using saliva disease markers.
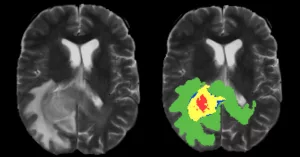
Oral Pathology
Periodontitis, peri‑implantitis, oral lichen planus, and even precancerous leukoplakia leave molecular footprints in saliva. A landmark study from 2009 showed that patients with high salivary MMP‑8 were far more likely to experience disease flare‑ups than those with low levels according to the authors. In practice, a dentist can order a simple saliva test, receive a risk score, and tailor cleaning intervals accordingly.
Systemic Disease Screening
Saliva doesn’t just whisper about your mouth; it shouts about the rest of you. Elevated cortisol may flag chronic stress; abnormal glucose hints at diabetes; a pattern of miRNAs can raise the saliva cancer risk. A 2015 Oral Biology review argued that “saliva offers an attractive, non‑invasive alternative for systemic disease screening” because it mirrors blood‑borne biomarkers without the needle according to the authors.
Treatment Monitoring
Imagine finishing a course of antibiotics and having a quick spit test to confirm the infection is really gone. Or tracking a chemotherapy patient’s tumor response through miRNA levels in their morning saliva. These real‑time snapshots are already being piloted in few forward‑thinking clinics.
Benefits & Risks
Every superhero has a kryptonite, and saliva diagnostics are no exception.
Benefits
- Non‑invasive: No needles, no bruises.
- Low cost: Collection kits cost pennies compared to lab draws.
- Convenient: You can collect at home, even while watching Netflix.
- Real‑time data: Because saliva reflects the current state of your glands, you get up‑to‑the‑minute information.
Limitations & Risks
- Variability: Food, drinks, and the time of day can shift marker levels.
- Sample handling: Improper storage degrades DNA and proteins.
- Standardization gaps: Not all labs use the same cut‑off values, which can lead to inconsistent results.
Experts suggest using standardized collection kits, fasting for at least 30 minutes before sampling, and storing specimens on ice until they reach the lab. These best‑practice steps dramatically cut down false‑positive noise.
How To Collect & Analyze
Ready to try it yourself? Follow this “DIY” guide (but remember, a professional interpretation is essential).
Step‑by‑Step at Home
- Rinse your mouth with water—no brushing or mouthwash for 30 minutes.
- Sit comfortably, tilt your head slightly forward, and let saliva pool in your mouth.
- Spit gently into a sterile tube until you have about 2 mL of fluid.
- Seal the tube, place it on ice, and ship it to a certified lab within 24 hours.
Lab‑Based Analysis Methods
Different markers need different tech:
- ELISA – great for cytokines like IL‑6.
- Luminex – multiplexes many proteins at once.
- qPCR – detects DNA/RNA fragments, perfect for viral loads or miRNA panels.
- Next‑gen sequencing – the heavyweight for comprehensive saliva molecular biomarkers research.
If you’re curious about which platform suits your need, a recent Metabolites 2023 article recommended starting with ELISA for single‑marker checks, then graduating to multiplex or sequencing when you want a broader health picture according to the authors.
Emerging Research & Future Directions
Saliva diagnostics are still in their teenage years, but the future looks dazzling.
Multi‑omics Panels
Scientists are now merging proteomics, metabolomics, and genomics into a single “saliva‑omics” panel. Such panels can predict disease risk with accuracy rivaling traditional blood tests, while keeping the process painless.
Artificial Intelligence
Machine‑learning models trained on thousands of saliva profiles can spot patterns invisible to the human eye. A 2023 AI‑driven study achieved 92 % accuracy in distinguishing early‑stage oral cancer from healthy controls according to the researchers.
Point‑of‑Care Devices
Imagine a pocket‑sized device that reads your saliva and flashes a risk score on a smartphone. Prototype sensors using nanotech are already in clinical trials, aiming for market release by 2027.
Roadmap to Adoption
- 2025‑2027: Validation of multi‑omics panels in large cohorts.
- 2028‑2030: Regulatory clearance for AI‑based diagnostics.
- 2031+: Widespread insurance coverage, integration into routine health checks.
Quick Takeaways
Here’s a concise checklist you can keep on your fridge (or phone) the next time you think about health monitoring:
- Identify the health question (e.g., “Am I at risk for gum disease?”).
- Choose a reputable saliva‑testing lab that offers the needed marker panel.
- Follow the standard collection protocol – no food, no drink, 30‑minute fast.
- Ship the sample promptly, keep it cool.
- Discuss results with a qualified clinician; use them to tailor prevention or treatment plans.
- Stay updated on emerging panels, especially if you’re interested in precision medicine research.
Conclusion
Saliva disease markers are turning a humble bodily fluid into a sophisticated health radar. From spotting early gum inflammation to flagging hidden cancers, the science is solid, the process is painless, and the future promises even more power in a pocket‑size kit. While we must respect the current limits—variability, the need for standardized labs, and professional interpretation—the benefits far outweigh the drawbacks for anyone who values early, actionable insights into their health.
If you’ve ever felt uneasy waiting for test results, imagine swapping that anxiety for a quick, at‑home spit test that tells you whether you’re on track or need a deeper look. That’s the promise of saliva diagnostics, and it’s arriving sooner than you think. Take a moment today to explore the options, talk to your dentist or physician, and see how a simple swish could become your new health‑checking habit.























Leave a Reply
You must be logged in to post a comment.