Ever wonder why your doctor sometimes seems to have a crystal ball? In a nutshell, precision medicine research is giving clinicians that magic edge — matching the right therapy to the right person, faster and safer than ever before. The NIH’s All‑of‑Us program alone is gathering genetic and health data from over 1 million volunteers, and early results already show we can predict which drugs will work (and which won’t) before the first pill is even prescribed. Below, I’ll walk you through what this research really means, why saliva is becoming the “new blood,” and how you can stay ahead of the curve without feeling overwhelmed.
What Is Precision Medicine
Definition & Core Elements
Precision medicine isn’t a buzzword; it’s a disciplined approach that blends three ingredients: genetics, environment, and lifestyle. By analysing a patient’s DNA, the chemicals they’re exposed to, and daily habits, researchers can pinpoint disease pathways that traditional “one‑size‑fits‑all” methods miss. Think of it as swapping a plain‑vanilla ice cream for a sundae custom‑made with your favorite toppings.
How It Differs From “Personalized Medicine”
While the two terms are often used interchangeably, there’s a subtle difference. “Personalized” usually refers to tailoring care based on clinical observations alone, whereas “precision” digs deeper—leveraging molecular data, big‑data analytics, and often AI to forecast outcomes. A quick side‑by‑side table helps clarify:
| Aspect | Personalized Medicine | Precision Medicine |
|---|---|---|
| Data Source | Symptoms, imaging | Genomics, proteomics, lifestyle |
| Decision Tool | Clinician judgment | Algorithm‑enhanced models |
| Scope | Broad adjustments | Molecular‑level targeting |
Quick Fact Box
Key stat: The NIH reports that over 70 % of oncology trials now include a genomic component, a dramatic jump from just 15 % a decade ago.
Key Benefits Overview
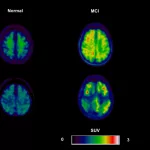
More Accurate Diagnosis & Early Detection
Imagine catching a disease before it even shows symptoms — that’s the promise of saliva molecular biomarkers. Saliva is a treasure trove of DNA, RNA, proteins, and microbes, providing a non‑invasive window into what’s happening deep inside the body. Studies show that a simple spit test can flag early‑stage oral cancers with over 85 % accuracy, sparing patients the anxiety of invasive biopsies.
Tailored Therapies & Reduced Side‑Effects
Pharmacogenomics, the study of how genes influence drug response, is already preventing adverse reactions. For instance, patients with a specific CYP2C19 variant avoid the dangerous clopidogrel bleed risk because their doctors know to prescribe an alternative. The result? Fewer emergency room visits and a smoother recovery.
Population‑Level Insights (Precision Public Health)
Precision isn’t only about individuals; it scales up to communities. A recent Nature study highlighted how geography‑linked genetic risk scores can guide public‑health campaigns, ensuring resources reach neighborhoods that need them most.
Benefits Table
| Traditional Approach | Precision Medicine |
|---|---|
| One drug for all patients | Drug selected based on genetic profile |
| Diagnoses after symptoms appear | Predictive biomarkers enable pre‑symptomatic detection |
| Trial‑and‑error dosing | Optimized dosing using pharmacogenomics |
| Limited data sharing | Secure, consent‑driven data pools (e.g., All‑of‑Us) |
Risks and Ethics
Data Privacy & Participant Confidentiality
When you hand over your genetic code, you’re handing over a piece of your identity. Reputable programs follow HIPAA‑compliant encryption and give participants full control over who sees their data. Still, no system is foolproof, so it’s wise to read consent forms carefully and ask about data‑ownership policies.
Health Disparities & Bias
Unfortunately, most large genomic databases have been overwhelmingly White. The University of Oklahoma’s recent paper in NPJ Precision Oncology showed that colon‑cancer risk markers differ dramatically in American Indian and African‑American cohorts. Ignoring such diversity can leave whole communities behind, perpetuating inequities.
Over‑reliance on Algorithms
Algorithms are brilliant, but they’re only as good as the data fed into them. A false‑positive biomarker could lead to unnecessary treatment, while a missed signal might delay care. That’s why clinicians must pair AI insights with human judgment.
Balancing Act Checklist
- Ask: Who owns my genetic data?
- Verify: Is the lab CLIA‑certified?
- Check: Does the test consider my ancestry?
- Discuss: What happens if a result is “uncertain”?
Saliva Research Frontier
Why Saliva?
Saliva is cheap, painless, and can be collected at home — all without needles. It contains DNA, RNA, proteins, and the oral microbiome, making it a multi‑dimensional snapshot of health. That’s why researchers are calling it the “new blood.”
Key Applications
Saliva disease markers are already being used to monitor stress hormones, track diabetes progression, and even predict cardiovascular risk. Check out this deep dive on saliva disease markers for a real‑world look.
When it comes to cancer, the story gets even more exciting. A handful of saliva cancer risk studies have identified micro‑RNA signatures that flag malignant transformations months before imaging can.
Example Study Summaries
- Nature Communications (2022): Discovered genetic signals linking pneumonia susceptibility to certain psychiatric disorders, suggesting a saliva‑based genetic test could guide both antibiotics and mental‑health interventions.
- Duke’s OneDukeGen (2023): Integrated saliva DNA with electronic health records to predict heart‑failure risk, achieving a 30 % improvement over traditional risk scores.
Mini‑Guide: How a Saliva Test Works
- Spit into a sterile tube (no food or drink for 30 minutes).
- Seal and ship the tube at ambient temperature — many labs provide prepaid packaging.
- Lab extracts DNA/RNA, runs next‑generation sequencing, and reports results within 2‑3 weeks.
- Your physician reviews the report, discusses actionable steps, and integrates findings into your care plan.
Research Programs Overview
| Program | Scope | Notable Findings | Relevance to You |
|---|---|---|---|
| All‑of‑Us (NIH) | +1 M volunteers, diverse ethnicity | Genetic variants linked to drug metabolism | Explains why some meds work for you and others don’t |
| OneDukeGen (Duke) | 100 k participants, integrated DNA/clinical data | Cardiometabolic risk prediction improves 30 % | Shows how your health record can become a predictive tool |
| TOPMed (NHLBI) | 200 k genomes, focus on heart, lung, blood | Identified new loci for asthma severity | Helps researchers create better inhaler strategies |
| Saliva Pilot Studies | 5 k+ saliva samples worldwide | Early detection of oral cancer via miRNA | Means a simple spit test could one day replace a painful biopsy |
These programs are not isolated silos; they share data (with consent) to accelerate discovery. So when you read a headline about a new cancer drug, chances are it’s already being tested in one of these massive cohorts.
Clinician Integration Tips
Building a Multidisciplinary Team
Precision care works best when doctors, genetic counselors, data scientists, and pharmacists sit at the same table. In my clinic, we hold a 30‑minute “genomics huddle” every week to review any new test results and decide on next steps together.
Decision‑Support Tools
Modern EMRs now embed algorithmic alerts. When a patient’s chart shows a CYP2D6 variant, the system automatically suggests an alternative antidepressant dose. It’s like having a second set of eyes that never sleeps.
Practical Workflow for Saliva Tests
- Order the test directly from the EHR.
- Provide the patient with a pre‑paid kit and simple instructions.
- Lab sends a secure PDF report to the physician portal.
- Schedule a follow‑up to interpret results and discuss lifestyle tweaks.
Quick‑Start Checklist
- Identify patients who could benefit (e.g., recurrent infections, unclear drug response).
- Confirm insurance coverage for genetic testing.
- Document consent clearly in the chart.
- Set up a post‑test counseling session.
- Update the care plan based on actionable findings.
Future Tech Trends
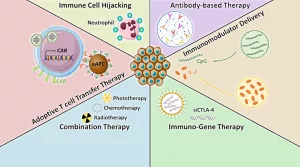
Multi‑omics Integration
Beyond DNA, researchers are layering proteomics, metabolomics, and even microbiome data to create “digital twins” of patients. These virtual avatars can simulate how a new drug will behave before anyone ever takes it.
AI & Machine Learning
According to a 2023 NIH roadmap, AI models trained on the All‑of‑Us dataset can predict heart‑attack risk 15 % earlier than conventional risk calculators. The key is transparent, explainable AI — you’ll always know why a model flagged a risk.
CRISPR‑Based Therapeutics
Gene‑editing is moving from the lab bench to the bedside. Early‑phase trials for sickle‑cell disease already show patients living symptom‑free after a single infusion. While still experimental, CRISPR illustrates the power of targeting the root cause rather than the symptoms.
Timeline Infographic (2025‑2035)
2025: FDA approves first saliva‑based cancer screen.
2027: Nationwide integration of AI risk scores into primary‑care EHRs.
2030: Multi‑omics “digital twin” platforms become standard for complex diseases.
2035: Routine CRISPR therapies for monogenic disorders.
Conclusion
Precision medicine research is turning the vague “one‑size‑fits‑all” model into a finely‑tailored experience that feels almost magical. From saliva‑based early detection to AI‑driven risk scores, the field is delivering real‑world benefits while also confronting genuine challenges around privacy and equity. By staying informed — whether that means reading a non‑invasive early diagnosis article or chatting with your doctor about genetic testing — you become an active partner in your own health journey. So, what’s the next step for you? Explore the links, ask questions, and remember: the future of healthcare is already knocking on your door, and it’s bringing a straw‑filled cup of personalized care.























Leave a Reply
You must be logged in to post a comment.