You’ve probably seen the bread aisles flooded with “low glycemic” options, including oat β-glucan bread, all claiming to help with blood sugar control. But here’s the thing: even though oat β-glucan has health perks, swapping your regular bread daily won’t magically slash your Type 2 Diabetes risk markers. This isn’t about telling you to suffer with dry toast—it’s about understanding what actually works.
Type 2 Diabetes isn’t just a numbers game. You might feel constant fatigue, unexplained weight loss, or that weird “I’m still hungry even after eating a sandwich” hunger. These aren’t random—it’s your body quietly screaming for help. Let’s unpack the truth with a side of real talk (and, yeah, maybe a cold beer metaphor for stress management). Spoiler alert: No single food fixes everything. Let’s dive in.
The Hype Behind Oat Bread
Ever heard the advice that fiber-rich foods are your pancreas’s best friend? Oat β-glucan bread leans into this by promising sustained energy without blood sugar spikes. Makes sense, right? Oats are whole grains, so they must be better than white bread. But here’s the plot twist: a recent study in The American Journal of Clinical Nutrition found that replacing your daily sandwich with oat β-glucan bread didn’t lower long-term A1C levels or improve insulin resistance. Yep, that’s the test that measures average blood sugar over 3 months.
Oat Bread: Fiber, But Not a Miracle
Fiber’s good, don’t get me wrong. Oat β-glucan is a soluble fiber that thickens your intestinal lining, slowing down glucose absorption, but it’s not a band-aid for systemic insulin chaos. Think of your blood sugar like traffic: oat bread might ease one intersection, but if the entire highway is backed up (aka your liver+muscle cell insulin resistance), you’re still stuck in gridlock.
Cases Where Oat Bread Can Fit
| Scenario | How Oat Bread Helps |
|---|---|
| You’re not bothered by bread sugar crashes | May help with short-term energy stability |
| You eat high-carb meals | Reduces glycaemic index of entire meal |
In other words, oat bread isn’t inherently “bad.” It just isn’t the whole solution. More on that later.
Type 2 Diabetes: Not Your Fault, But Nowhere To Hide
Let’s get personal for a sec. Type 2 Diabetes isn’t just about your diet; it’s about your genes, your stress, your sleep, and the way your body sometimes just… stops cooperating. You can eat bamboo shoots and avoid soda but still have it—even your uncle’s cigars and couch-potato habits might’ve played a role. So where does this leave us with oat β-glucan and other “healthy” staples of modern diets?
Here’s the raw deal: about 37 million Americans have diabetes, and 90% of them have Type 2. And if you’re dealing with it already, you’re likely familiar with the frustration of diving into a Whole Foods aisle, picking up every “low glycemic” product, and failing to get that blood sugar control down to target. Don’t beat yourself up. This isn’t easy.
Insulin Resistance Explained (Like I’m Talking to My Sister)
Think of insulin as a key trying to open a rusty lock. In Type 2 Diabetes, your body tries hard to turn that key (your pancreas produces insulin), but the lock (your cells) won’t budge (insulin resistance). Eventually, your pancreas burns out and the key breaks entirely—so blood sugar stays high, and damage starts creeping in.
Fun fact: the more fat your belly holds, the more “inflammation” chemicals you produce, like tumour necrosis factor-alpha. These make your cells tighter and faster to reject insulin’s DJ set. That’s why 40% of people with Type 2 Diabetes have a belly fat component driving this—yet oat bread alone won’t rewire that mess. It’d be like trying to fix a termite problem with a single bedroom cleaner.
The Study That Shook Bread Science
In 2025, a study with 400 T2D overweight participants tried replacing?regular bread with oat β-glucan bread over 8 weeks. The goal? Lower A1C, fasting blood glucose, and insulin resistance—the real “report card” for long-term diabetes management. The result? Nothing significant. But not in a doom-and-gloom way. Here’s what did move the needle:
- Weight loss: A 5% loss of your body weight cut insulin resistance by 20%.
- Exercise time: 30 minutes of moderate movement post-dinner—like dancing to an old playlist—reduced post-meal glucose spikes by 18%.
- Stress balance: Meditation? Therapy? Decreasing road rage (okay, emotional stress)? All statistically dropped C-reactive protein, a silent inflammation marker dragging your blood sugars up.
What Went Wrong With the Oat Bread Assumption
The science was sound: oat β-glucan slows glucose absorption. The flaw? It’s focusing on just ONE meal component when Type 2 is a lifestyle, genetic, environmental scene. Toll of this: You might feel full longer with oat bread, which can help control calories—but if you’re still sitting most of the day and living off cheap wine and fast food? Exactly. It’s not oat bread vs. disaster—it’s habits vs. habits, and the bread has a limited solo role.
Don’t Ignore These Diabetes Risk Markers
Here’s what the CDC and ADA warn you should flag, even if you’re “too young”:
- Dark rashes near your neck: A clinical marker called acanthosis nigricans—your body’s “Dude, we’re insulin-resistant over here.”
- Tingling is not a normal foot massage: One of the earliest signs of nerve damage. If you’ve been chalking it up to sitting at your desk, take note.
- Healing sores like: Got a knee scrape that’s into its third week? High glucose = power-washing your healing microbes with slowdown juice. It’s a red flag.
So How Do You Know If You’re At Risk?
Let’s talk stats in a real way from the NIDDK: 1 in 3 people have prediabetes, where blood sugar’s creeping up into “pre-battle-stations” territory. Do you need to eat oat bread? No.
The Real Work Behind Managing Type 2 Diabetes
Managing this isn’t about bread—it’s about hitting that trifecta of lifestyle change, blood monitoring, and sometimes medication. Here’s the breakdown:
1. Movement: Step, Stretch, Dance Like You’re Backstage
I know, “movement” sounds guilty until proven whimsical. But laughter—according to Harvard Health—a brisk walk keeps inflammation low and blood vessels flexible. Not into morning runs? Start with dancing while making your coffee. Or walks during podcasts. Just don’t sit all day—it’s like suffocating your cells in a plush cushion of cholesterol buildup.
2. Food Is Data, Not a Scapegoat
The problem isn’t pasta. It’s bio-physics. Regular small meals rich in fats, proteins, and complex carbs (maybe with a lil’ oat β-glucan) help. But to be brutally honest, it’s okay to crave Twinkies—the trick is to slow them down with healthy fats and protein so you don’t have a glucose tsunami. Just don’t fall for the whole “If I eat oat bread, I’ll magically remiss.” Spoiler: it doesn’t.
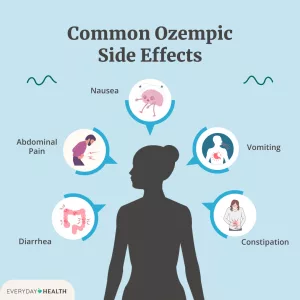
3. Medication & Monitoring: When Science Steals the Show
For many, lifestyle isn’t enough. Your doctor might prescribe Metformin, sulfonylureas, or even insulin—each has a role. And let’s be clear, your glucose monitoring might feel overkill (how many finger pokes are really needed?), but the data police your long-term. Don’t skip your A1C test—listening to “I didn’t feel off” isn’t how you prevent retinopathy.
Case Study: When Bread Change Wasn’t Enough
Meet Sarah. 48, no family history, all-in on low glycemic foods and oat bread. Still had nerve damage and blurry vision in 2 years. What gives? 8 hours of sleep get = none. Remote work, back-to-back stress meetings, and evenings watching TikTok instead of moving. Turns out, inflammation’s the party crasher, which even oat fiber can’t stop when you’re always dying inside (tip for those chasing stability: sleep and curiosity reduce this).
The One Thing You Can Do: The 7-Day Diabetes Risk Hacks
Ever heard of hacking wellness trends, where one change ripples into others? Let’s do that—raw, unoffical, without the wellness creepy-crawl:
Test Run: Your 7-Day Diabetes Defense
- Day 1: Swap one snack (cereal nightcap, salty crackers) for almond butter and apple slices. Fiber + protein to stabilize.
- Day 3: 15 mins of yoga-based stretching post-meal. Helps lower glucose faster than a singsongy salad diet.
- Day 5: Book your A1C and cholesterol tests. Even if you feel “fine.” (Type 2 diabetes often isn’t loud until it’s a full-on party.)
- Day 7: Cook one pasta dish with lentils instead of full gluten. Offer the other half to your boyfriend’s emails.
Bottom Line: Bread Tastes, But Work Serves
Oat β-glucan bread’s a tried-and-true grain with soluble fibers that help with heart health and digestive complaints. But if you’ve been counting on it to lower your diabetes risk markers or feel like you’re “doing something,” the science says: rethink. Ever heard the term: high fiber, but not all the fiber solves, not even if you’re low glycemic all day.
Now What? A Friendly Nudge
If you’re sitting there with your oat-wrapped sandwich thinking “Ugh, now what do I eat?”, slap a high-protein topping on toast and walk around the block after lunch. Before you know it, the habits will sneak in. Don’t overthink the science. Don’t ghost it, either. Just take the next, stress-free bite—and the next step beyond bread.
Got Tips, Woes, or Questions?
Post them below! Let’s keep this chat real. Have a friend who waves off diabetes by munching gluten-free bread? Share this piece and school them gently.
You’ve Got This—Real Talk, Real Change
No one said this was easy, but you’ve made it this far. Oat bread’s not the villain. And you’re not weakness. Knowledge? Yeah…glucose moderation plus anti-inflammatory life wins a little time, every day. The formula’s not rocket science. It’s you, yeast, exercise, and not skipping the glucose monitor Band-Aid when it’s time to peek.
Stay Grounded, Not Ghosted
This isn’t a sprint to diabetes remission or risk. It’s walking the downbeat—day after day, after day. Which is why resistant bread isn’t a foundation. But focused habits? Yep. Ask yourself, today: are you done fighting? Or ready to rethink what your body’s telling you—with signs, stories, and subtle A1C shifts? No oat bread will ever answer that for you. You will.





















Leave a Reply
You must be logged in to post a comment.