Hey there, you’ve just heard the words “type 2 diabetes” and your mind is probably doing somersaults. “What now?” you’re asking yourself. Good news: the first 30 days are the perfect launchpad for a healthier, more controlled life. In this guide I’ll walk you through the exact steps a doctor would recommend, sprinkle in real‑people stories, and hand you a printable checklist you can start using tonight. Let’s dive in—no fluff, just the stuff that actually helps.
Set the Foundation
What are the three‑step priorities in the first month?
Think of the first month as three pillars that keep everything balanced:
- Lab baseline: Get a fasting glucose and A1C test. These numbers tell you where you’re starting.
- Medication & monitoring schedule: Work with your doctor to set doses, timing, and when to check your blood‑sugar.
- Diet & activity plan: Choose realistic meals and a gentle exercise routine you can stick to.
Why does the “first‑month window” matter?
During the first few weeks your body is still figuring out the new insulin balance. Research from the American Diabetes Association shows that early, consistent control can improve insulin sensitivity and lower the risk of complications down the road. In other words, the effort you put in now can pay off for years to come.
What warning signs mean you need immediate help?
Even though most people feel fine at first, some red flags deserve a call to your provider right away:
- Fasting glucose consistently > 200 mg/dL
- Severe hypoglycemia (shakiness, confusion, fainting)
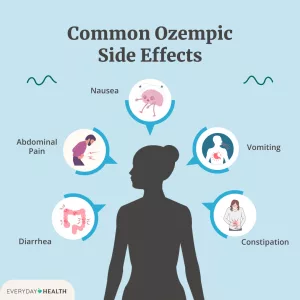
- Persistent nausea, vomiting, abdominal pain – possible ketoacidosis
For a quick reference, the ADA’s taking medication page lists these warning signs in plain language.
Build a Diet
How to design a 30‑day meal plan that actually works?
The secret isn’t “no carbs forever”; it’s the plate method. Fill half your plate with non‑starchy vegetables, a quarter with lean protein, and the remaining quarter with whole‑grain carbs or starchy veg. This simple visual keeps portions in check without counting every calorie.
| Day | Breakfast | Lunch | Dinner |
|---|---|---|---|
| 1‑7 | Greek yogurt + berries + chia | Grilled chicken salad (olive oil vinaigrette) | Salmon, quinoa, steamed broccoli |
| 8‑14 | Scrambled eggs + spinach + whole‑grain toast | Turkey wrap on lettuce, side of carrot sticks | Stir‑fried tofu, brown rice, mixed peppers |
| 15‑21 | Overnight oats (flax, almond milk, cinnamon) | Bean chili, small sweet‑potato | Lean beef kebabs, grilled zucchini |
| 22‑30 | Smoothie (protein powder, kale, frozen berries) | Quinoa bowl with chickpeas, avocado, cucumber | Baked cod, cauliflower mash, green beans |
Feel free to swap proteins or veggies—just keep the plate ratios the same.
Which carbs are “safe” vs. “risky” in the first month?
Safe carbs have a low glycemic index (GI) and release glucose slowly. Think lentils, barley, berries, apples, and sweet potatoes. Risky carbs spike quickly—white bread, sugary drinks, pastries, and most breakfast cereals. Replacing a sugary snack with a handful of nuts or a piece of fruit can make a huge difference in your post‑meal numbers.
Can I still enjoy my favorite foods?
Absolutely. The goal isn’t deprivation; it’s moderation. If you love pizza, have a slice, but pair it with a big salad and a glass of water. That way the fiber in the salad slows sugar absorption, keeping your glucose more stable.
What role does fiber & protein play in blood‑sugar control?
Fiber forms a gel‑like barrier in your gut, slowing the entry of glucose into the bloodstream. Protein does the same by stimulating a slower insulin response. Aim for at least 25 g of fiber a day—examples include a cup of beans, a medium apple with skin, or a serving of oatmeal.
Medication & Monitoring
Which meds are most common in the first month and why?
For most people, metformin is the first‑line drug. It lowers liver glucose production and improves insulin sensitivity. Doctors typically start with a low dose (500 mg) to reduce stomach upset, then gradually increase.
If your A1C is above 9 % or you have symptoms like frequent urination, a second oral agent (like a GLP‑1 receptor agonist) may be added. These newer meds also help with weight loss—a nice double win.
How to set up a blood‑glucose testing routine?
Here’s a simple schedule that works for most beginners:
- Morning (fasting): Right after you wake, before breakfast.
- Pre‑meal: About 15 minutes before lunch and dinner.
- 2‑hour post‑meal: Helps you see how a specific meal affected your sugar.
Log each reading in a notebook or a free app—seeing trends over a week makes adjustments crystal clear.
What questions should I ask my pharmacist/doctor this month?
Good communication cuts confusion. Keep this mini‑script handy for your next appointment:
“Can you walk me through the timing of my medication with meals?”
“What side‑effects should I watch for?”
“If I miss a dose, what’s the best way to handle it?”
“Do any of my other meds interact with this one?”
When is insulin ever needed in the first month?
Most people manage without insulin initially, but there are exceptions:
- A1C > 9 % with symptoms of high blood sugar.
- Pregnancy or severe hyperglycemia that doesn’t respond to oral meds.
- Rapid weight loss or hospitalization.
If insulin is prescribed, doctors usually start with a short‑acting (prandial) dose before meals, then add a basal (long‑acting) dose if needed.
Lifestyle Hacks Guide
What type of exercise is safest for a brand‑new diagnosis?
Start gentle. Aim for at least 150 minutes of moderate activity per week—think brisk walking, cycling, or water aerobics. Add two days of resistance training (bodyweight squats, wall push‑ups) to boost muscle mass, which in turn improves insulin sensitivity. Always check your glucose before and after workouts; a reading between 80‑180 mg/dL is generally safe.
How does sleep affect blood‑sugar in the first month?
Sleep is the unsung hero of glucose control. Poor sleep spikes cortisol, a stress hormone that raises blood sugar. Aim for 7‑9 hours of consistent, uninterrupted rest. Keep screens out of the bedroom, dim the lights an hour before bed, and consider a short breathing exercise if you find yourself tossing.
Stress‑reduction techniques that actually lower glucose?
Stress hormones (epinephrine, cortisol) act like a hidden sugar‑spike button. Simple practices can flip that switch off:
- 5‑minute mindful breathing (inhale 4, hold 4, exhale 4).
- Journaling one grateful thing each night.
- Short walks in nature—studies show green space reduces stress hormones according to medical research.
Quick daily habit checklist
- Morning: water, meds, glucose check, balanced breakfast.
- Mid‑day: short walk, water, pre‑lunch glucose, protein‑rich lunch.
- Evening: review day’s log, prepare tomorrow’s meals, relax with a book.
- Before bed: final glucose check, set alarm for medication if needed.
Real Stories Shared
First‑month success story: “From confused to confident in 28 days”
Sarah, 52, was terrified when her doctor said “type 2 diabetes.” She started with a metformin prescription, logged every glucose reading, and swapped sugary snacks for a handful of almonds and an apple. By day 28 her A1C dropped from 8.2 % to 7.0 %, and she felt more energetic than she had in years. “It wasn’t magic,” she says, “it was simply doing one small, doable thing each day.”
Common pitfalls: “What I wish I’d known sooner”
Mark, 44, skipped meals trying to “cut carbs” and ended up with low blood sugars and headaches. He also ignored his doctor’s advice to start a light walk, thinking it was “too much effort.” The lesson? Consistency beats intensity. Small, regular meals and a 10‑minute walk are far more sustainable than drastic restrictions.
How to find a supportive community
Loneliness can magnify stress. The American Diabetes Association hosts online forums where people share triumphs and setbacks. The Diabetes.co.uk community is another friendly space where you can ask about medication timing, recipe tweaks, or just vent.
30‑Day Action Plan
Week‑by‑Week checklist
| Week | Goal | Key Actions |
|---|---|---|
| 1 | Baseline & Basics | Get fasting glucose & A1C, start metformin, log every reading, set up meal‑plan template. |
| 2 | Nutrition Upgrade | Follow plate method, replace one sugary snack with fruit, begin 15‑minute daily walk. |
| 3 | Review & Adjust | Check trends, discuss any side‑effects with doctor, consider adding a second oral agent if A1C > 7.5 %. |
| 4 | Fine‑Tune & Celebrate | Finalize daily routine, schedule 1‑month follow‑up appointment, download printable planner. |
Tools & resources
- Free glucose‑log apps: MySugr, Glucose Buddy.
- Printable “First‑Month Planner” (PDF) – a quick‑reference sheet you can tape to your fridge.
- Credible reading: the ADA’s understanding diabetes page and the Low Carb Program for lifestyle evidence.
When to schedule your 1‑month follow‑up
Ask your provider to review:
- Current A1C and fasting glucose.
- Medication tolerance and any side‑effects.
- Blood‑sugar log trends – are you staying within target range?
- Any adjustments needed to diet or exercise.
Conclusion
Congratulations—by reading this you’ve already taken the first step toward mastering your first month type 2 diabetes journey. Remember, the three pillars—baseline labs, a sensible medication & monitoring plan, and a balanced diet plus gentle movement—are your allies. Stay curious, keep logging, and lean on community support when things feel overwhelming. Download the printable checklist, try one new low‑glycemic recipe this week, and let us know how it goes. You’ve got the tools; now go show your new diabetes treatment plan who’s boss.






















Leave a Reply
You must be logged in to post a comment.