Hey there, friend. If you’ve just heard the words “colorectal cancer biomarker testing” and feel a little lost, you’re not alone. Imagine trying to solve a puzzle without the picture on the box – that’s what treatment planning can feel like without this test. In the next few minutes we’ll walk through why the test matters, who should get it, how it works, and what to expect afterward. Think of this as a coffee‑chat with a buddy who’s done a bit of homework on the subject, so you can walk into your next appointment feeling informed and confident.
Why Testing Matters
What’s a biomarker, anyway?
In plain language, a biomarker is a tiny signal that tells doctors what’s happening inside your tumor. It can be a mutation in the DNA, a protein that the cancer cells spit out, or a change in the way cells behave. The NCCN guidelines describe biomarkers as “specific features of cancer cells,” including proteins and DNA changes. Those features become the GPS for your treatment plan.
How biomarkers steer diagnosis, prognosis, and therapy
Biomarkers wear three different hats:
- Diagnostic: They help confirm that a growth is cancer and not a harmless polyp.
- Prognostic: They give clues about how aggressive the tumor might be.
- Predictive: They tell doctors which drugs are most likely to work (or not work) for your particular cancer.
When you hear doctors talk about a “biomarker panel,” they’re usually referring to a set of tests that look for the most clinically relevant signals—all in one report.
Quick comparison of common biomarkers
| Biomarker | Clinical Use | Typical Test | Example Action |
|---|---|---|---|
| KRAS/NRAS | Predictive (anti‑EGFR therapy) | DNA sequencing | Avoid cetuximab if mutated |
| BRAF V600E | Predictive (targeted inhibitors) | DNA sequencing | Consider encorafenib + cetuximab |
| MSI‑H/dMMR | Predictive (immunotherapy) | IHC or PCR | Use pembrolizumab |
| HER2 amplification | Predictive (HER2‑targeted therapy) | FISH/IHC | Add trastuzumab |
Who Should Get Tested
Universal recommendation
All patients diagnosed with colorectal cancer are advised to have biomarker testing—no exceptions. Whether the tumor is in the colon or the rectum, the test can uncover clues that change the whole treatment approach.
Stage‑specific panels
Here’s a handy breakdown:
- Stage 0–I: Test for MSI‑H/dMMR (helps decide if adjuvant chemo is needed).
- Stage II–III: KRAS, NRAS, BRAF, HER2, and a comprehensive panel that may also include ctDNA for minimal residual disease monitoring.
- Stage IV (metastatic): Full‑scale “biomarker panel” plus liquid‑biopsy (circulating tumor DNA) to catch mutations that might emerge after first‑line therapy.
Decision‑tree snapshot
Picture this flowchart in your mind: you get a colonoscopy → a tissue sample is taken → pathologist confirms cancer → the oncologist orders the appropriate biomarker panel → results guide your personalized treatment plan. Simple, right?
Testing Process Step‑by‑Step
Sample collection: tissue or blood?
The classic route is a tissue biopsy taken during surgery or colonoscopic removal of the tumor. If the tumor is hard to reach, or if you’ve already had a lot of procedures, a “liquid biopsy” (just a standard blood draw) can substitute for many of the same tests. Both are safe; a blood draw is even less invasive, which many patients appreciate.
Lab work‑up behind the scenes
Once the sample reaches the molecular lab, several techniques are applied:
- Next‑generation sequencing (NGS): reads thousands of DNA fragments at once to spot mutations like KRAS or BRAF.
- Immunohistochemistry (IHC): stains tissue to reveal protein expression (e.g., HER2, dMMR).
- Fluorescence in situ hybridization (FISH): pinpoints gene amplifications such as HER2.
- Circulating tumor DNA (ctDNA): a blood‑based test that can detect the same mutations without a tissue sample.
Timeline you can expect
Most accredited labs deliver a full report within 7–14 days after the specimen is received. If you’re waiting for a liquid biopsy, the clock can be a little faster because the processing steps are streamlined.
Reading the report—what to look for
A typical colorectal cancer testing report includes:
- Patient ID and specimen type.
- List of biomarkers that were examined.
- Positive findings (e.g., KRAS G12D mutation).
- Therapeutic recommendations tied to each finding (e.g., “Consider anti‑EGFR therapy if KRAS wild‑type”).
Don’t stare at the jargon in silence—ask your doctor to walk you through each line. It’s your health, and you deserve a clear explanation.
Benefits vs Risks
The upside—why it’s worth it
- Tailored therapy: Matching drug to mutation boosts response rates and reduces unnecessary side effects.
- Clinical trial eligibility: Many cutting‑edge studies require a specific biomarker profile—testing can open doors you didn’t know existed.
- Peace of mind: Knowing the molecular makeup of your tumor removes guesswork from the equation.
The flip side—limitations to keep in mind
- False‑negatives/positives: No test is 100 % perfect; some low‑frequency mutations can slip through.
- Turn‑around time: Waiting for results may feel like a long pause before treatment starts.
- Insurance variability: Coverage for the full biomarker panel isn’t guaranteed; it can depend on your plan, state, and cancer stage.
Risk‑mitigation checklist
| What to Ask | Why It Matters |
|---|---|
| Is the test FDA‑cleared for my cancer type? | Ensures clinical validity. |
| What is the sensitivity for low‑frequency mutations? | Helps gauge false‑negative risk. |
| Will my insurance cover the full panel? | Avoid surprise bills. |
| Can I get the results in a patient portal? | Quick, secure access to your data. |
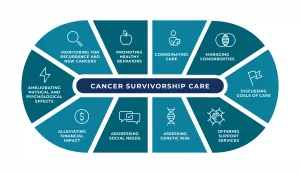
After You Get the Results
Discussing with your oncologist
Bring a notebook (or your phone) and ask clear, focused questions. Here are a few you can start with:
- “What does my KRAS status tell us about anti‑EGFR therapy?”
- “If my tumor is MSI‑H, should we prioritize immunotherapy?”
- “Are there any clinical trials that match my biomarker profile?”
Good doctors love engaged patients. Your curiosity signals that you’re a partner in the decision‑making process.
Personalized treatment pathways
Based on the biomarker panel, your oncology team might suggest one of several routes:
- Targeted therapy: For BRAF‑mutated tumors, drugs like encorafenib (often combined with cetuximab) can be game‑changers.
- Immunotherapy: MSI‑H or dMMR tumors respond remarkably well to pembrolizumab or nivolumab.
- Chemotherapy combos: When no actionable mutations are found, traditional regimens still have a role, guided by stage and overall health.
Real‑world example
Imagine a patient named Alex (pseudonym). After surgery for stage III colon cancer, Alex’s biomarker panel showed a KRAS G12C mutation and high microsatellite instability. The oncologist recommended adjuvant chemotherapy followed by pembrolizumab—an approach that likely wouldn’t have been considered without that test. Six months later, Alex’s scan was clear, and he felt empowered knowing the treatment was chosen based on concrete data rather than a “one‑size‑fits‑all” approach.
Practical Tips & Resources for Patients
Preparing for the biopsy (or blood draw)
- Ask whether you need to fast—most tissue biopsies don’t require it, but certain blood tests might.
- Write down any medications (especially blood thinners) and share them with the team.
- Arrange a ride home; some patients feel a little light‑headed after a sedation or anesthesia.
Post‑test support networks
Knowing you’re not alone can make a huge difference. Two trustworthy sites that consistently update their information on colorectal cancer biomarkers are Fight CRC and Know Your Biomarker. They offer patient stories, printable checklists, and links to clinical trials.
Take‑away checklist (downloadable PDF)
Feel free to copy the table below into a notes app or print it:
| Step | What to Do |
|---|---|
| Before test | Confirm insurance coverage; note any medication adjustments. |
| Day of test | Bring ID, insurance card, and a list of questions. |
| After results | Schedule a dedicated meeting with your oncologist; bring the report copy. |
| Ongoing | Update your health record if new biomarkers appear (e.g., from ctDNA monitoring). |
Conclusion
Colorectal cancer biomarker testing is more than a lab number—it’s the roadmap that tells you which lanes are open and which are closed on the road to recovery. By understanding what biomarkers are, who needs them, and how the results shape treatment, you can walk into every appointment armed with knowledge and confidence. Remember, you don’t have to navigate this alone; lean on your care team, reach out to patient‑advocacy groups, and keep asking questions. If anything feels unclear, drop a comment below or talk to your doctor—you deserve a plan that’s as unique as you are.




















Leave a Reply
You must be logged in to post a comment.