What Is It?
Ever wonder why some babies are born with extra fingers, a tiny heart defect, or why certain families seem to run in circles with miscarriages? Most of the time, the culprit is a tiny mistake in the way our chromosomes are set up. A chromosome abnormalities study is simply a deep‑dive into those mistakes—how they happen, what they look like, and why they matter for health, fertility, and even cancer.
Types of Changes
When researchers talk about “chromosome abnormalities,” they’re usually referring to two big families: numeric (the number of chromosomes is off) and structural (the pieces are broken, swapped, or flipped).
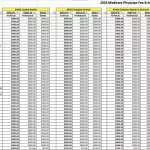
| Type | Numeric vs. Structural | Typical Signs | How Common |
|---|---|---|---|
| Trisomy 21 (Down syndrome) | Numeric – extra copy of chromosome 21 | Intellectual disability, characteristic facial features | ≈ 1/700 live births |
| Monosomy X (Turner) | Numeric – missing one X chromosome | Short stature, infertility, heart anomalies | ≈ 1/2,500 female births |
| Translocation | Structural – pieces swap between chromosomes | Varies; can cause infertility or miscarriage | ≈ 0.2 % of newborns |
| Inversion | Structural – a segment flips inside the same chromosome | Often silent; may disrupt meiosis | Very rare |
These patterns aren’t just academic; they guide everything from prenatal counseling to cancer risk assessment.
Why It Matters
Imagine you’re building a house. If you accidentally place the wrong number of bricks—or misplace a load-bearing wall—the whole structure can become shaky. Chromosome imbalances do the same to our bodies. They’re a leading cause of:
- Congenital anomalies—birth defects that can affect organs, growth, or development.
- Recurrent pregnancy loss—often the silent reason behind multiple miscarriages.
- Infertility—especially when sperm or eggs carry extra or missing chromosomes.
- Cancer risk—cells with the wrong chromosome count tend to become chaotic, a hallmark of many tumors.
For instance, researchers have linked certain chromosome imbalances to chromosome imbalances cancer pathways, and they’re also exploring how a faulty mitochondrial function cancer connection fuels these instabilities.
How We Detect Them
No magic crystal ball needed—just modern genetics labs. Here’s the usual toolbox:
Karyotyping
The classic method. It takes cells, spreads them on a slide, stains the chromosomes, and looks at the big picture under a microscope. Great for spotting whole‑chromosome extra copies or large deletions, but it can miss tiny changes.
Chromosomal Microarray (CMA)
Think of CMA as a high‑resolution map that can detect gains or losses as small as 100 kb. A 2024 study in the International Journal of General Medicine showed CMA caught abnormalities in 15 % of fetuses with abnormal ultrasounds—far more than karyotype alone.
Fluorescence In‑Situ Hybridisation (FISH)
FISH zooms in on a specific chromosome region using fluorescent probes. It’s fast and perfect when you already suspect a particular disorder, like the 21‑probe for Down syndrome.
Next‑Generation Sequencing (NGS)
Whole‑genome sequencing can reveal even the smallest copy‑number variations and point mutations. It’s becoming more affordable, but interpreting the flood of data still needs expert eyes.
Below is a quick comparison to help you see which test might fit your situation:
| Test | Resolution | Turn‑around | Detects |
|---|---|---|---|
| Karyotype | ≈ 5 Mb | 1‑2 weeks | Whole‑chromosome gains/losses, large translocations |
| CMA | ≈ 100 kb | 2‑3 weeks | Microdeletions/duplications, unbalanced translocations |
| FISH | Targeted | Days | Specific loci (e.g., 22q11.2) |
| NGS | Single‑base | 4‑6 weeks | All variants, including single‑gene disorders |
Global Patterns
Chromosome abnormalities don’t respect borders, but their frequency does shift with healthcare access, prenatal screening programs, and even cultural practices. Here’s a snapshot from a few studies:
- Saudi Arabia – A retrospective review of newborns with major congenital anomalies found that ~12 % carried a detectable chromosomal abnormality.
- North‑East Iran – The 2013 Cell J paper reported a pattern where trisomy 21 was the most common, followed by a variety of structural rearrangements.
- Central China – In a massive cohort of 14,965 infertile couples, 0.5 % of women were carriers of balanced translocations that could affect pregnancy outcomes.
- WHO EMRO (2025) – Among 137 children with suspected genetic issues, 38.7 % showed abnormal karyotypes, underscoring the value of cytogenetic testing.
These numbers illustrate a simple truth: the more we look, the more we find. Improved screening (like non‑invasive prenatal testing, NIPT) has already lowered the surprise factor for many families.
Managing a Diagnosis
Finding an abnormality can feel like opening a Pandora’s box, but there’s a roadmap:
- Confirm the result. Most labs will repeat the test or run a complementary assay (e.g., CMA after an abnormal karyotype).
- Get a genetics consultation. A certified genetic counselor can translate the numbers into real‑world risk percentages.
- Discuss reproductive options. Pre‑implantation genetic testing (PGT‑A), donor gametes, or adoption are all valid pathways.
- Plan for health surveillance. Some chromosomal imbalances heighten cancer risk; regular check‑ups and targeted screening become part of the plan.
One practical tip: if you’re a parent facing a new diagnosis, write down three questions before your appointment. It helps keep the conversation focused and ensures you leave with the answers you truly need.
Future Frontiers
Scientists aren’t just cataloguing faults; they’re hunting for fixes.
Single‑Cell Sequencing
By analyzing each embryo cell individually, researchers can spot mosaicism (where some cells are normal, others aren’t) and decide which embryos have the best chance of healthy development.
CRISPR‑Based Corrections
Early lab work shows it might be possible to “edit out” a small deletion or duplication before implantation. We’re a few years away from clinical use, but the momentum is real.
Link to Mitochondria
Oddly enough, mitochondria—our cell’s power plants—play a role in chromosome segregation. Faulty mitochondrial function cancer pathways can lead to mis‑segregated chromosomes, feeding the cycle of instability.
Protein Imbalance
When chromosome numbers go awry, the balance of proteins in a cell is thrown off. This protein imbalance cells scenario is a hot research area for new cancer drug treatments—see the cancer drug treatment page for a deeper dive.
Take‑Away Checklist
- Ask your doctor about a family history of chromosomal conditions.
- Consider NIPT after 10 weeks if you’re pregnant.
- If an abnormal result pops up, schedule a genetics consult right away.
- Explore reproductive options that feel right for you.
- Stay on top of any recommended health surveillance (especially cancer screening).
Closing Thoughts
Chromosome abnormalities may sound intimidating, but remember—they’re tiny variations in a massive, beautiful system. Understanding them empowers you to make informed choices, eases anxiety, and opens doors to supportive care. Whether you’re a soon‑to‑be parent, someone grappling with infertility, or simply a curious reader, I hope this walk‑through gave you clarity and a sense of control.
What part of a chromosome abnormalities study resonated most with you? Have you or a loved one navigated a genetic diagnosis? I’d love to hear your story—feel free to reach out. Together, we can turn complex science into personal confidence.





















Leave a Reply
You must be logged in to post a comment.