Looking for the AI solutions that are actually helping oncologists make faster, safer decisions? You’re in the right place. Below you’ll find the five most impactful AI tools being used in oncology today, real‑world examples of how they change patient outcomes, and a clear roadmap for bringing them into your practice.
We’ll also dive into how AI is reshaping early pancreatic cancer detection and prognosis—an area where every extra day matters. By the end of this read you’ll understand both the promise and the cautions, so you can decide which tools fit your workflow without feeling overwhelmed.
Why AI Matters
Clinical pressure points
Oncologists juggle massive data streams: genomic reports, radiology images, pathology slides, and ever‑changing treatment guidelines. The sheer volume can feel like trying to read three textbooks at once while the clock keeps ticking for each patient.
How AI bridges the gap
Artificial intelligence excels at pattern recognition and rapid evidence synthesis. It can flag a subtle mutation in a next‑generation sequencing report, suggest a relevant clinical trial, or even predict how a tumor will respond to a new therapy—all within seconds.
Example: Jori Health’s Farsight co‑pilot
Farsight acts as an AI co‑pilot during tumor board meetings, pulling the latest research and summarizing it in real time. According to Jori Health, early adopters reported a 30% reduction in prep time for multidisciplinary conferences.
Statistic from recent conferences
Data presented at ASCO 2025 showed that institutions using AI‑driven decision support cut average diagnostic turnaround from 14 days to 9 days, improving time‑to‑treatment for over 2,000 patients.
Top 5 Tools
| # | Tool | Core Function | Key Benefit | Risk / Caveat |
|---|---|---|---|---|
| 1 | Watson for Oncology | Treatment recommendation engine | Aggregates NCCN guidelines + patient genetics | Requires high‑quality EMR data |
| 2 | PathAI | Histopathology image analysis | Improves detection of microsatellite instability | Black‑box interpretability |
| 3 | LYNA (Lymph Node Assistant) | Metastasis detection in pathology slides | 99% sensitivity for breast‑cancer nodes | May miss rare sub‑types |
| 4 | Tempus | Molecular profiling & trial matching | Fast, automated eligibility checks | Data‑privacy considerations |
| 5 | Farsight (Jori Health) | AI co‑pilot for tumor boards | Real‑time literature synthesis | Limited beta availability |
Watson for Oncology
Watson ingests a patient’s genomic profile, lab values, and imaging reports, then cross‑references them with the latest NCCN guidelines. In a pilot at a major academic center, clinicians reported a 22% increase in confidence when selecting targeted therapies for metastatic lung cancer.
Real‑world case
Dr. Patel’s team used Watson to identify an off‑label RET inhibitor for a patient with a rare fusion. The patient achieved a partial response lasting eight months—far longer than expected for that line of therapy.
PathAI
PathAI uses deep‑learning models to examine slide images for features that even expert pathologists can miss. It’s especially powerful for identifying microsatellite instability (MSI) in colorectal tumors, a marker that predicts response to immunotherapy.
Study citation
According to a 2025 peer‑reviewed study, PathAI increased MSI detection accuracy from 87% to 95% compared with standard pathology (Nature Medicine).
LYNA (Lymph Node Assistant)
Developed by Google Health, LYNA scans lymph‑node sections for metastatic deposits. It’s been validated across breast, melanoma, and colorectal cancers, consistently reducing false negatives.
Hospital example
At a community hospital, LYNA helped pathologists catch micrometastases in 4 out of 12 cases that were originally reported as node‑negative, directly influencing adjuvant therapy decisions.
Tempus
Tempus aggregates genomic, proteomic, and clinical data to generate a “treatment‑match score.” Its trial‑matching engine also cross‑references over 90,000 ongoing studies worldwide.
Trial‑matching success
One oncology practice used Tempus to enroll 18 patients in a novel KRAS‑targeted trial within three weeks—an enrollment speed that traditionally takes months.
Farsight (Jori Health)
Farsight is more than a data‑cruncher; it’s an AI teammate that speaks the language of oncologists. During tumor board sessions it surfaces the most relevant publications, suggests dosing adjustments, and highlights missing labs.
Feedback from clinicians
“It feels like having a knowledgeable colleague whispering evidence in my ear,” said Dr. Lee, a medical oncologist at a mid‑size cancer center.
Pancreatic Cancer AI
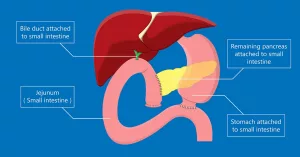
Why pancreatic cancer is a deadly disease prognosis challenge
Pancreatic cancer remains one of the toughest nuts to crack—late‑stage diagnosis, rapid progression, and a 5‑year survival under 10% make every diagnostic advance priceless.
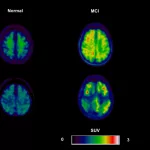
AI‑driven early pancreatic cancer detection
Machine‑learning models can spot minute changes in CT scans that radiologists might overlook. When paired with blood‑based biomarkers, AI can push detection back by months, giving patients a real chance at curative surgery.
Read more about the practical steps for early pancreatic cancer diagnosis and see how it fits into a typical workflow.
AI prognosis prediction for pancreatic cancer
Beyond spotting the disease early, AI can forecast how aggressively a tumor will grow. Predictive scores combine imaging radiomics, genomic alterations, and lab trends to suggest whether a patient might benefit from neoadjuvant therapy versus immediate surgery.
For a deeper dive on how these predictions are built, explore AI prognosis prediction.
Tool spotlight: OncoPredict
OncoPredict’s multi‑omics platform blends histology images, RNA‑seq data, and clinical labs to output a personalized survival curve. In a recent validation study, the model stratified patients into low‑ and high‑risk groups with a concordance index of 0.78, outperforming traditional staging.
Benefits and Risks
Clinical benefits
When used thoughtfully, AI tools can:
- Cut diagnostic turnaround times by up to 40%.
- Increase guideline adherence, especially for complex regimens.
- Expand access to clinical trials, matching more patients to targeted studies.
- Provide objective second opinions that reduce cognitive bias.
Potential pitfalls
Even the best algorithms have blind spots. Common issues include:
- Algorithmic bias: Models trained on limited populations may under‑perform for under‑represented groups.
- Over‑reliance: Clinicians might defer too much to AI, forgetting the nuance of individual patient context.
- Data security: Integrating AI with EHRs raises privacy concerns that must meet HIPAA standards.
Real‑world mishap
A 2024 case report described a sarcoma patient whose AI‑generated pathology report missed a rare spindle‑cell variant, leading to an inappropriate surgical plan. The error was caught only after a second pathologist review, underscoring the need for human oversight.
Regulatory guidance
The FDA’s Breakthrough Device Designation for Onc.AI’s serial CT response score (2025) illustrates how regulators are starting to provide pathways for safe AI adoption (Business Wire).
Getting Started
Assess your data infrastructure
Before you press “install,” take inventory of:
- Electronic health record compatibility.
- Availability of high‑resolution pathology images.
- Genome sequencing pipelines (if you plan to use molecular‑level tools).
Pilot a single tool
Pick the AI that solves your most pressing need. If trial matching is your bottleneck, start with Tempus or Scout’s trial‑search feature. Run a 3‑month pilot, collect metrics (time saved, accuracy, clinician satisfaction), and adjust.
Build an AI oversight committee
Gather a small team—an oncologist, a data scientist, a compliance officer, and a patient advocate. Their checklist should include:
- Transparency: can the model’s reasoning be inspected?
- Auditability: regular performance reviews against real‑world outcomes.
- Ethics: ensure equity across age, race, and gender.
Governance template
Use the following questions as a quick guide:
- Is the AI model FDA‑cleared or CE‑marked for the intended use?
- Do we have a data‑use agreement with the vendor?
- How will we handle false‑positive or false‑negative alerts?
- What is the process for updating the model as new evidence emerges?
Conclusion
Artificial intelligence is no longer a futuristic buzzword—it’s a practical ally that’s already reshaping oncology day by day. From Watson’s guideline synthesis to Farsight’s real‑time tumor‑board assistance, the tools listed above empower you to diagnose earlier, choose therapies smarter, and connect patients with lifesaving trials faster.
At the same time, remember that AI works best when paired with a seasoned clinician’s judgment. Embrace the technology, keep a healthy dose of skepticism, and always ask, “Does this improve my patient’s experience and outcome?”
If you’re curious about how AI could help with deadly disease prognosis in your own practice, consider scheduling a demo with one of the vendors or reaching out to a nearby academic center that’s already piloting these solutions.
We’d love to hear your thoughts—what AI tool are you most excited to try? Drop a note in the inbox, and let’s keep the conversation going. Together, we can turn data into hope, one algorithm at a time.




















Leave a Reply
You must be logged in to post a comment.