Hey there, friend. If you’ve just heard the words follicular lymphoma diagnosis and feel a mix of curiosity, worry, and maybe a dash of “what‑now?”, you’re not alone. In the next few minutes we’ll walk through the exact tests doctors use, why each one matters, and what you can expect after the results come back. Think of this as a friendly cheat‑sheet you can pull out before your next appointment – no jargon, just clear, honest talk.
Understanding the benefits and the risks of every test helps you ask the right questions and stay in the driver’s seat of your own care. Let’s get started.
Why Testing Starts
What puts the ball rolling?
Most journeys begin with a simple physical exam. Your doctor will feel for swollen lymph nodes in the neck, underarms, or groin, and check whether your spleen or liver feels enlarged. According to the Mayo Clinic, these findings are the first clues that something might be going on.
But physical signs are just the tip of the iceberg. B‑symptoms – night sweats, unexplained fever, or losing more than 10 % of your weight – can also signal that a deeper investigation is needed. Blood cancer charities like Blood Cancer UK note that these symptoms often appear before anyone even thinks about cancer.
Goals of a follicular lymphoma diagnosis
- Confirm the disease: Is it really follicular lymphoma, or something else?
- Identify the grade and genetics: Different patterns of proteins and DNA changes guide treatment choices.
- Stage the cancer (I‑IV): Knowing how far it’s spread helps doctors pick the right therapy.
Core Diagnostic Tests
Below is a quick‑glance table of the main tests you’ll hear about, why they’re ordered, what they reveal, and their typical pros‑and‑cons.
| Test | Why It’s Ordered | What It Shows | Typical Risks / Benefits |
|---|---|---|---|
| Full blood count & chemistry (LDH, liver/kidney panels) | Baseline health; rule out anemia; assess LDH (marker of aggressive change) | Blood cell counts, organ function, possible disease activity | Simple, low‑risk blood draw – Mayo Clinic |
| Flow cytometry / Immunohistochemistry (IHC) | Detect surface proteins that define follicular lymphoma | Presence of CD10, CD20, BCL2, BCL6, CD23 (and absence of CD5, CD43) | Highly specific; needs tissue sample |
| Genetic / molecular studies (FISH, NGS, PCR) | Identify translocations (t(14;18) IGH‑BCL2) and mutations | Prognostic & therapeutic targets | Requires biopsy tissue; costlier but increasingly routine |
| Imaging (CT, MRI, PET/CT) | Map disease distribution, evaluate organ involvement | Stage (size & location of nodes), monitor response | Radiation exposure; PET/CT gives functional data – HealthTree |
| Lymph node biopsy (excisional or core needle) | Gold‑standard tissue diagnosis | Histology, grade, architecture, protein expression | Invasive but definitive |
| Bone‑marrow aspiration/biopsy | Check marrow involvement for staging | Presence of lymphoma cells in marrow, additional genetics | Minor discomfort; outpatient procedure |
How the tests flow in real life
Most doctors start with the easy stuff: blood work and a quick CT scan. If those raise red flags, they’ll order a PET/CT to pinpoint the exact spots that need a biopsy. The tissue sample then goes through IHC, flow cytometry, and genetic testing all at once, giving a complete picture in one lab visit.
What the day of a biopsy feels like
Picture this: you’re lying on a padded table, a local anesthetic tingles, and a surgeon gently removes a whole lymph node from your neck or armpit. It sounds scarier than it is – most patients report only a brief pinch and a mild soreness afterward. Adding a short personal note here, a friend of mine once said, “I was terrified until the nurse whispered, ‘You’ll barely feel a thing,’ and then I was up and about in an hour.”
Reading Your Results
Pathology report basics
The pathology report is the star of the show. It lists the grade (1‑3), the pattern (follicular vs diffuse), and a Ki‑67 index that tells how fast the cells are dividing. Higher grades often mean a more aggressive approach.
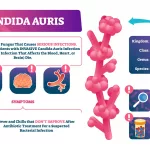
Genetic markers that matter
When the lab spots the classic t(14;18) translocation, it confirms the typical follicular lymphoma pathway. Other mutations, like EZH2 or TP53, can shift treatment toward targeted agents or clinical trials. HealthTree explains that these genetic clues help predict whether the disease might transform into a more aggressive form.
Staging the disease
Doctors use the Ann Arbor system: Stage I (one region), Stage II (two regions on same side of the diaphragm), Stage III (both sides), and Stage IV (spread to bone marrow or other organs). Add an “A” or “B” suffix depending on the presence of B‑symptoms. For example, “Stage III B” tells you the lymphoma is on both sides of the diaphragm and you’ve got night sweats or fever.
Why stage matters
Early‑stage (I‑II) disease can sometimes be observed without immediate treatment—a “watch‑and‑wait” approach that spares you from chemo side‑effects. Advanced stages (III‑IV) usually need systemic therapy, often a combination of immunotherapy and chemotherapy.
Next Steps After Diagnosis
Treatment options at a glance
- Watch‑and‑wait: For low‑grade, asymptomatic disease.
- Immunotherapy (rituximab, obinutuzumab): Targets CD20 on B‑cells.
- Chemo‑immunotherapy (e.g., bendamustine + rituximab): Common first‑line for symptomatic patients.
- Targeted agents (lenalidomide, EZH2 inhibitors): Chosen based on genetic findings.
- Clinical trials: Always worth a conversation if you’re comfortable with experimental therapies.
When to ask for a second opinion
It’s perfectly okay to visit another hematologist‑oncologist to confirm the staging or discuss alternative regimens. A fresh set of eyes can sometimes spot a trial you didn’t know existed.
Living with uncertainty
Dealing with a new cancer diagnosis is an emotional roller coaster. Support lines such as the Blood Cancer UK helpline (0808 2080 888) are staffed by caring professionals who can answer practical questions and simply listen. Connecting with a patient community—online forums, local support groups, or the Follicular Lymphoma Foundation—helps you realize you’re not navigating this alone.
Checklist for your first oncology visit
- Bring a copy of all test results (blood work, imaging reports, pathology).
- Write down any symptoms, even if they seem minor.
- Prepare questions: “What does my stage mean for everyday life?” “What are the side‑effects of the recommended regimen?”
- Ask about fertility preservation, if relevant.
- Note down the doctor’s answers—don’t rely on memory alone.
Common Questions Answered
What test actually proves follicular lymphoma?
The definitive answer comes from an excisional lymph‑node biopsy evaluated with immunohistochemistry and genetic studies. Imaging and blood work are essential, but they can’t replace tissue confirmation.
How long does a PET/CT take and why is it useful?
A PET/CT usually lasts about 30 minutes. The radioactive tracer lights up metabolically active cells, showing exactly where the lymphoma is lurking. This functional picture helps decide the stage and later monitors treatment response.
Can blood work alone diagnose the disease?
No. Blood panels can hint at abnormal cell counts or a high LDH level, but without a tissue sample you can’t be certain.
What does a “B” symptom mean for my stage?
B‑symptoms (fever, night sweats, weight loss) upgrade any stage to an “‑B” suffix, indicating a higher‑risk disease that may need earlier intervention.
Is “watch‑and‑wait” ever safe?
Yes—if your lymphoma is low‑grade, limited to one or two regions, and you have no B‑symptoms, many experts recommend observation with regular check‑ups. It avoids unnecessary toxicity while keeping a close eye on any change.
Your Journey Map
Step‑by‑step timeline
- Symptom or incidental finding: You notice a lump or your doctor finds swollen nodes.
- Initial labs & basic imaging: Blood work and a CT scan rule out immediate emergencies.
- PET/CT for precise mapping: Highlights all suspicious areas.
- Biopsy of the key node: Tissue sent for pathology, flow, and genetics.
- Staging discussion: Results are placed into the Ann Arbor system.
- Treatment planning: Multidisciplinary team decides on watch‑and‑wait, chemo‑immunotherapy, or a trial.
- Follow‑up: Regular scans and blood work to watch for progression or relapse.
Visual tip
If you’re a visual learner, draw a simple flow chart on a sticky note. Color‑code each step (green = tests, blue = results, red = decisions). Seeing the path laid out can calm the “what‑if” anxiety.
Conclusion
Getting a follicular lymphoma diagnosis is less about a single test and more about a coordinated series of examinations that together paint a clear picture of what’s happening inside your body. From the first blood draw to the final staging scan, each step offers valuable clues that guide your treatment plan and help you stay informed.
Remember, knowledge is power—and the more you understand the why behind each test, the more confidently you can speak with your care team. If anything feels overwhelming, reach out for a second opinion or a supportive community; you don’t have to walk this road alone.
Take a deep breath, keep this guide handy, and feel free to share your own experiences or questions in the comments below. We’re all in this together.





















Leave a Reply
You must be logged in to post a comment.