Sure, you might’ve heard the phrase “colon cancer” and thought, “Yikes, that’s my grandpa’s territory – not mine.” But hold up. The hard-to-ignore truth? Colon cancer isn’t just for folks in their 60s anymore. New data says younger adults – your 20s, 30s, even early 40s – are dying from this. Why? There’s a real problem brewing.
Stick around. We’re diving into why clinicians are seeing this spike, how to spot signs, and (this is the important part) the little things you can do that’ll pull your colon cancer numbers down. No long-boring paragraphs. Just raw truth and real steps to take – in case you’ve been ignoring that weird belly discomfort or disgusting poops for months.
Colon Cancer in Young Adults – What’s Going On?
Is Colon Cancer Real in Your 20s or 30s? Data Don’t Lie
You look at some folks on the internet and you think, “Colon cancer? Me? Nah man, I chase burrito nights and late-night calorie bombs, but cancer? Not here.” But scientists aren’t just speculating about trends. Over the past 15 years, colorectal cancer diagnoses among people 20 to 49 have increased by about 1.5% a year, per Cleveland Clinic and Mayo Clinic.
Here’s the hot take: yes, most colon cancers hit older adults. But more cases among younger groups are showing up – and that’s not coincidence. Doctors are still figuring out the exact “why,” but here’s what they know – it’s not just random cells breaking loose. Things are shifting in our guts. That means your habits, what you eat, where you fall on the sedentary scale – these all matter.
What Lies Behind the Trend? Hidden Risk Factors Too Many Miss
Okay, buckle up. A lot of my younger friends saw this coming – until they didn’t. Scientists are blaming multiple factors, not just a single root cause.
Ultra-processed diet seems to pass as the top suspect. Not “just” fast food. We’re talking boxed pizzas, can-open-food meats, junk-based meals. Western-style eating = colon cancer potential. Cleveland Clinic put it like this – “the newer generation is metabolically transitioning from colon-healthy to colon-unfriendly habits.”
Lack of movement is no joke. We sit – at work, marathons on Netflix, in cars. Mayo Clinic flagged this in their recent article: People with low to zero physical activity are more prone to a mix of unhealthy colon cell growth, especially if nothing in your life suggests otherwise. That posture isn’t doing favors for your colon cells.
Genetics? Some people just have it in the cards. Conditions like Lynch syndrome and familial adenomatous polyposis turn normal colon tissue into a ticking time bomb. If even one close family member had the disease? Yeah, you’re now dodging a potential wave of colon issues without early screening. And guess what? Most young adults neglect their ‘worst-case story’ until it’s too real.
Race, Gender and the Numbers You Should See
Let’s get real: Black people in the U.S. are dying more from colon cancer than other ethnicities. Cleveland Clinic flagged the increased risk. And men – no matter assigned at birth – are getting more colon cancer than women. These are not casual facts. They matter. A lot.
But here’s the thing – colon cancer in young people flies under the radar until symptoms pop. We downplay fatigue, write off stool changes as diet losses, or ignore blood because yep, it could be hemorrhoids. But catching it late? That’s why colorectal cancer will take 53,000 Americans this year.
It’s time to stop pretending this doesn’t touch us until we’re 50. Doctors recommend screening starting at 45 now for average-risk individuals. Go earlier if symptoms hit, or get genetic testing if family history runs toxic with colon cancer. This isn’t bitter science. This is how to define your odds without panic.
Symptoms You Shouldn’t Laugh Off (Even if You’re Young)
Spotting the First Warning Signs: Real People, Real Moments
Meet Jacob. A guy in his early 30s who thought his weird poops were a quinoa overload until he bled. “Blood in your stool and you chalk it up to spicy Thai food? Your next hospital trip in 6 weeks might not be optional.”
Real story: Jacob’s symptoms were passed as IBS for months until a doctor finally insisted on a colonoscopy. By that point, the tumor had grown deeper. His diagnosis? Stage 3.
This is not unique. Cleveland Clinic released case studies of younger patients who shrugged off persistent symptoms for way too long. They thought it was stress, fatigue, you-fill-in-the-blank-explanation, until a real, active cancer diagnosis forced them into pain management.
Can You Confuse These Symptoms for Other Digestive Issues?
You can! We all get it – the digestive system is… well, a mean, messy loop of symbiotic parts. But that casual dismissal? It’s where colon cancer slips in.
Here’s what might be pushing colon cancer under the radar:
- A three-week dry spell? Irritable Bowel Syndrome (IBS) believes and ends the conversation.
- Belly pain? Overthinking? Maybe. But researchers say ongoing gnawing or cramps are colon cancer flags.
- Blood on your stool? “Just hemorrhoids again.” Yet, one Mayo Clinic study explained that “not all rectal bleeding points to benign conditions,” especially when it pops during bowel cancer growth.
- Weight loss no matter what you eat? Not always diabetes or thyroid stuff. Imagine your body silently going into restriction, even with full appetite.
- Feeling tired for no clear reason? Could be burnout. But it could be chronic internal bleeding and anemia – a common result of colon cancer development.
You sure feel like a “different” person each week. But if a few of those signs keep overlapping? Rate your concern higher. Notice how your body responds when you cut back on fast food or sleep better. Improvement tips from medical groups say lifestyle shifts can sometimes ease early-stage parallels.
Omitted Signs Leading to Later Diagnosis
Keep this in your pocket – screening won’t even pick up most symptoms. You’re the first sensor.
Symptoms you might not realize? Here’s what’s tricky:
- Pooping habits change and won’t fix. Can’t be passed off with a couple smoothies or MiraLax runs.
- Post-bowel feeling that the gut’s not empty? That bloating that clings whether you’ve pooped or not.
- Your stool is narrower. Hashtag “poop change” – even if you don’t see blood, that difference counts.
| Symptom | Colon Cancer Indicator | More Common Explanation |
|---|---|---|
| Blood in stool | Colon polyp / early tumor tears | Hemorrhoids or anal cracks |
| Stool shape changes | Colon pathway narrowing | Diet / dehydration shifts |
| Loss of energy | Anemia due to internal bleeding | Poor sleep / stress |
| Abdominal pain | Gut distress from developing tumors | Gas, IBS, food sensitivity |
All these signs? They’re fine to ride on for a short-term irritation. Mixed and repeating for weeks or months? Mortality outcomes show that those who catch colon cancer in the earliest stage survive – those who wait… don’t always.
Getting Ahead: Screening, Prevention and Real Action
Screening Is the #1 Way Scientists Are Breaking Down Colon Cancer Deaths
Forget waiting until you’re 45 with “normal” risk. Cleveland Clinic’s updates show 20s are where symptoms start – but screenings start a decade earlier if your doctor suspects risk. Mayo Clinic supports colonoscopies in younger adults if there’s 1. family history, and 2. persistent belly discomfort!
You’ve heard about colonoscopies. So has everyone. But here’s the deal: if pre-cancerous polyps show up, early removal saves lives. Cleveland Clinic dropped it like this – “Want cancer prevention? Screening and surveilled colon removal make sense.”
How to Ask Your Doctor About Screening Before 45
The uncomfortable part? Most younger adults don’t start this convo until something hurts. Here’s how to pin the topic before it becomes personal:
- “I’m in my mid-30s and I’ve noticed blood in my poop twice in the last two months. Can we talk?”
- “My best friend was diagnosed at 32. I’m nervous. What should I know?”
- “My family on my dad’s side had colon cancer before 50. I’m 26 – should I have genetic testing?”
- “I’ve been feeling off for a while – not just a stomach thing.”
Brushing off fatigue, weight loss, or poops that “don’t sit right” without checkups isn’t a long-term win. The Mayo Clinic piece says “Colon cancer doesn’t wait for permission” – and neither do experts.
Also: Don’t brush off Cleveland Clinic’s advice. They’ve seen this. Their medical team dropped this line: “Tumor detection increases with early imaging and scope tests. If you’ve been avoiding this for fear of preparation – that bloating is temporary… cancer might not be.”
Simple Daily Moves That Lower Risk
Colon cancer prevention isn’t juicing over emo nights or yoga heels. We’re not selling life-changing pills here. But small shifts can!
- Eat more fiber. That means kale, yes, but beans, whole grains, and apples don’t kill your life either. The American Cancer Society = samples of cancer-friendly diets vs. ultra-processed ones you should never eat.
- Move at least a little. Stand up before your back emergency hits. Take a walk during lunch.”
- Chill out on alcohol. The U.S. medical board isn’t just being “judgy” – they see cutting back as a cancer prevention need. Three drinks a day? MedlinePlus links that to earlier colon cancer spikes.
- Quit smoking now. Not because it’s trendy, but because tobacco and cancer tags stick together like peanut butter and jelly.
- Track your polyp story. Even benign ones can turn to cancer over years, according to Cleveland Clinic.
As simple as that? Again. Colon cancer doesn’t knock. It pushes in quietly. But the tools for screening and prevention? They’ve improved a lot over the last decade. Back then, prevention strategies were ignored. Today, America is waking up to what colorectal cancer in younger people truly looks like and how many lives it’s taking quietly without alerts.
Getting Serious: The Treatments That Work and Still Make Sense
What Doctors Recommend – Stages They Begin With and Why
Colorectal cancer treatment? No one expects you to enjoy news like radiation, chemotherapy, or surgery. But here’s the deal – far from being outdated, oncology programs for colon cancer have evolved. Docs don’t just rely on these tools anymore; they personalize treatment now.
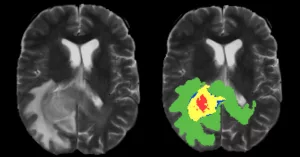
Let’s talk stages real quick but casual. Mayo Clinic categorizes colon cancer in stages from 0 to IV, each designed to determine the complexity of the tumor. Stages I and II often stick to your colon and are removed by surgery. Stage III cancer reaches a point where chemotherapy + radiation join the removal. Stage IV colon cancer? Sometimes spreads to the liver or lungs – treatment gets heavier, but more options + immunotherapies exist now than ever before.
Making decisions like “surgery for early or advanced tumor removal” usually relies on biopsies and imaging tests. Cleveland Clinic used this line the other day: “updates in colon cancer care emphasize disease profile over what hospital you’re in.” Not overly emotional. But makes sense for helping you understand if you’re an early or late-stage patient.
Immunotherapy and Genetic Targeting – Tailored for You
“Cancer drugs and IBS symptoms? Im not going for that.” Cancer care isn’t the ordeal it used to be. Let’s say this: Mayo Clinic and NCI support targeted therapy as a smarter, gas-lighter solution.
Stage IV patients, for example, aren’t relying on just chemotherapy anymore. NEW biologics, proved by current studies and post-5-year cancer web resources, help your immune system single out cancer mutation or tumor cells with way fewer side effects.
If you’re PRJ01CT – a cancer patient in the 21st-century treatment – maintenance plans sound less like (metaphorically) “hospital prison” and more like multi-step clinical approaches taking into account your tolerance, your genetic markers, and your higher life quality post-diagnosis.
Survivor Stories: “I Was Diagnosed in My 20s. I’m Here.”
Some of the best teaching points don’t come from clinical documentation. They come from real people. One cancer survivor summed up her days with a note: “I thought stage 2 meant I wouldn’t make 30. I did. Yes, fighting it sucked – chemo made me see colors differently. But early detection by a doctor? What saved me.
Her story teaches us: Detection + really triggering your checkup can pull the cancer card early. Not just when you feel it. Early.
We should take these lessons seriously. Cancer.org even shares survivor experiences and maybe interviews with young oncology teams, making the learning path easier and more relatable for people who hear the diagnosis and immediately go silent.
Taking Care of the Bigger Picture – Your Health, Your Empowerment
Experiencing Colon Cancer – Finding Strength through Voyage
And if confronting colon cancer hasn’t taught you enough, handling its aftermath can equal a life rehab. The digestive system changes. Nutrients interact differently. Weekly fatigue sticks.
Emotionally, it’s a sucker punch even after disease is gone. It hinges on taking those recovery steps seriously—like dietary tracking, protein rebuild, mental therapy when needed, and lifestyle shifts even future doctors agree with.
One survivor created a journal of “emotional gut check-ins” after her treatments. She wrote things like:
- “I feel food differently now. Some foods I loved before diagnosis crack me open, I’ve learned new.”
- “Gastrointestinal fatigue? Not always weakness. Sometimes it’s your newer colon system adjusting.”
- “Brain fog during chemo? Yeah common – made me question everything I taught myself for work. But after treatment – clarity follows.”
She turned that journal into a lifestyle guide. That’s survival that reaches beyond hospitals. Truthfully personal, valid, and helpful for someone who just asked “now what” after their diagnosis.
Encouraging Cancer Screenings for People Like You
“This isn’t just about me or what happened after my diagnosis. It’s about starting the conversation before someone’s precious Tom travels into worse treatments.”
Talk to your doctor. Ask your local clinic how they screen younger adults. And yeah, make sense of your gut before you start to see the characteristics others overlook. If you think colorectal cancer doesn’t touch people like us? Remember: 1 in 24 developing this. And nearly 50,000 die every year because symptoms and early diagnostics were avoided or even untested.






















Leave a Reply
You must be logged in to post a comment.