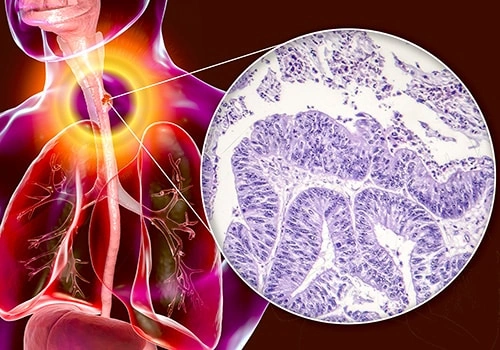
If you’ve just heard the words “esophageal adenocarcinoma” for the first time, your brain is probably buzzing with questions, worries, and maybe even a little hope that there’s a clear road ahead. I get it—being faced with a cancer diagnosis feels like stepping into a foggy forest without a map. That’s why I’m writing this as a friend who’s spent a lot of time listening to patients, reading the latest research, and watching how treatment strategies have evolved. Below you’ll find a relaxed, down‑to‑earth guide that walks you through the most common treatment options, how doctors predict whether chemotherapy will work, and what the future holds with precision‑oncology tools. Grab a cup of tea, settle in, and let’s explore together.
Benefits vs Risks
First things first: every treatment has a bright side and a shadow. Knowing both helps you make decisions that fit your life, not just your lab results.
- Potential upside: Multimodal therapy (surgery + chemo ± radiation) can push five‑year survival for stage II‑III disease up to 45‑50 %.
- Possible downside: Surgery carries a 2‑4 % risk of serious complications; chemotherapy can bring nausea, fatigue, and in rare cases, heart or lung toxicity.
- How to balance: Your age, heart and lung health, and personal priorities (like returning to work quickly) all tip the scale.
When I talk to patients, I say, “Think of treatment as a partnership. You bring your goals and limits; the medical team brings the science. Together you choose the plan that feels doable.” This mindset keeps the conversation honest and the choices realistic.
Standard Treatment Paths
Early‑Stage (0‑I): Endoscopic or Surgical Options
When cancer is confined to the innermost lining of the esophagus and measures less than 2 cm, doctors often start with minimally invasive techniques.
Endoscopic mucosal resection (EMR) & Radio‑frequency ablation
These procedures scrape or vaporize the tumor through an endoscope. Success rates hover around 90 % when the disease hasn’t invaded deeper layers. Recovery is usually a few days, and you can often go home the same day.
Minimally invasive esophagectomy
If the tumor is a bit larger or deeper, a surgeon may recommend a laparoscopic‑assisted or robot‑assisted esophagectomy. Though it sounds intense, the minimally invasive approach reduces pain and shortens hospital stays compared with traditional open surgery. Most patients resume light activity within 4‑6 weeks.
Locally Advanced (II‑III): Multimodal Approach
For cancers that have spread beyond the mucosa but are still potentially curable, the standard recipe includes three key ingredients: neoadjuvant (pre‑surgery) therapy, surgery, and sometimes adjuvant (post‑surgery) chemotherapy.
Neoadjuvant chemoradiation
The CROSS trial, published in 2015, showed that giving chemo‑radiation before surgery improved median overall survival from 24 to 49 months. The regimen typically combines carboplatin, paclitaxel, and 41.4 Gy of radiation over five weeks.
Surgery after down‑staging
Two popular surgical techniques are the Ivor‑Lewis (abdominal + chest incisions) and the trans‑hiatal (abdominal only). Your surgeon will pick the one that gives the best chance of clear margins while matching your anatomy.
Adjuvant chemotherapy
After a successful operation, many oncologists add a few cycles of FOLFOX or capecitabine to mop up any microscopic disease that might be lurking.
Metastatic (IV): Systemic Focus
When cancer has traveled beyond the esophagus, the battle shifts to controlling growth, easing symptoms, and extending quality‑time.
First‑line platinum‑based chemo
Cisplatin plus 5‑fluorouracil (or its oral cousin capecitabine) remains the backbone of first‑line therapy. It works for roughly 30‑40 % of patients, buying several months of disease control.
Targeted agents & immunotherapy
If your tumor tests positive for HER2, adding trastuzumab can boost response rates. For those with high microsatellite instability (MSI‑H) or PD‑L1 expression, checkpoint inhibitors like pembrolizumab have shown durable responses.
Clinical‑trial enrollment
Because new drugs are constantly entering the pipeline, many experts encourage patients to consider a trial. It’s like getting a sneak peek at the next generation of treatment while helping science move forward.
Predicting Chemo Success
Not every tumor loves chemotherapy the same way every person loves chocolate. That’s where chemotherapy effectiveness prediction tools come in.
Current Assessment Methods
Doctors usually start with imaging (PET‑CT) to see how “hot” the tumor is, then repeat the scan after a few weeks of therapy. A drop of more than 35 % in SUV‑max often signals a good response. Some centers also track circulating tumor DNA (ctDNA) — tiny fragments of cancer DNA floating in your blood that can hint at how well treatment is working.
Emerging Biomarkers & AI Platforms
Molecular profiling (NGS panels)
Next‑generation sequencing can uncover mutations in HER2, FGFR2, or mismatch‑repair genes, each of which may guide you toward a targeted agent instead of “one‑size‑fits‑all” chemo.
Artificial‑intelligence‑driven platforms
Recent studies (see a 2024 ASCO abstract) demonstrate that machine‑learning models that ingest imaging, pathology, and genomic data can predict who will respond to platinum‑based regimens with 78 % accuracy. It’s still early days, but the technology is heading toward bedside decision‑making.
Early signs of neoadjuvant chemotherapy resistance
If after two cycles the PET‑CT still lights up, or if ctDNA levels stay flat, your team may consider switching to a different regimen, adding radiation, or moving straight to surgery.
Practical Tips for Patients
- Keep a daily symptom diary – it helps your oncologist spot trends early.
- Ask about repeat PET‑CT or ctDNA testing before each chemo cycle.
- Don’t be shy about asking for a second opinion on biomarker results.
Future Precision Options
What Is a Precision Oncology Platform?
Think of it as a high‑tech matchmaking service. Your tumor’s DNA is sequenced, the data is fed into a multidisciplinary tumor board, and a personalized treatment plan is generated—often blending classic chemo with a targeted drug that hits a specific molecular “Achilles’ heel.”
Real‑World Impact on Esophageal Adenocarcinoma
Case study
John, 52, was diagnosed with HER2‑positive stage II disease. After standard neoadjuvant chemoradiation, his surgeons added trastuzumab to the adjuvant phase. Ten months later, his scans showed no evidence of disease, and John returned to his marathon training. A recent analysis of a national registry found that HER2‑targeted therapy added roughly a 10‑percentage‑point boost to two‑year overall survival for this subgroup.
Data snapshot
A 2024 NCCN report highlighted that patients whose treatment was guided by a precision oncology platform enjoyed a 12 % higher median progression‑free survival compared with those who received standard chemo alone.
How to Access These Tools
Ask your oncologist if the hospital participates in a molecular tumor board or if they can refer you to a nearby academic center. Many community hospitals now partner with commercial labs that provide quick turnaround on NGS panels.
Managing Side Effects
Chemo‑Related Toxicities
Even the best‑tolerated regimens can cause nausea, low blood counts, or peripheral neuropathy. Proactive measures include:
- Anti‑emetics: 5‑HT3 antagonists (ondansetron) are standard; adding dexamethasone can curb delayed nausea.
- Growth‑factor support: Filgrastim (G‑CSF) helps keep white blood cells up, especially if you’re at high risk for infections.
- Neuropathy guard: Dose‑adjustment of paclitaxel and regular foot‑checks can limit permanent nerve damage.
Post‑Surgical Nutrition & Quality of Life
After esophagectomy, the stomach is often pulled up to become a new “tube” for food. Here’s what helps:
- Early oral intake: Small, frequent meals start within a day if the surgeon allows.
- Feeding tubes: Some patients get a jejunostomy tube for the first 2‑3 weeks to ensure calories while the throat heals.
- Swallowing therapy: Speech‑language pathologists teach safe techniques and exercises that restore confidence.
Psychosocial Support
Facing cancer can feel isolating. Counseling, support groups, or even a trusted friend who simply listens can make a world of difference. Many centers also offer financial navigation to help with insurance paperwork and medication co‑pays.
Questions to Ask
| Question | Why It Matters |
|---|---|
| What is my exact stage and tumor location? | Determines which modalities are recommended. |
| Will I need neoadjuvant therapy? | Impacts surgery timing and overall prognosis. |
| Are there targeted drugs for my tumor’s genetics? | Opens the door to precision‑oncology options. |
| How will we monitor chemotherapy response? | Helps catch resistance early and adjust treatment. |
| What nutrition plan will support my recovery? | Prevents weight loss and improves healing. |
Feel free to bring a notebook to appointments—writing down answers helps you remember details later, and it shows your care team that you’re actively involved.
Key Takeaways
In a nutshell, here’s what we’ve covered:
- Multimodal therapy (chemo + radiation + surgery) remains the gold standard for curable esophageal adenocarcinoma.
- Modern tools—chemotherapy effectiveness prediction, ctDNA monitoring, and AI‑driven models—are sharpening the accuracy of response assessment.
- Precision oncology platforms are turning genetic data into personalized drug combos that can boost survival and lessen unnecessary toxicity.
- Side‑effect management, nutrition, and psychosocial support are equally important for a successful journey.
- Ask the right questions, keep an open dialogue with your multidisciplinary team, and consider clinical trials for cutting‑edge options.
Remember, you’re not walking this path alone. Your doctors, nurses, dietitians, and even the online community are all part of a supportive network. If anything feels overwhelming, pause, breathe, and reach out—whether it’s a phone call to your nurse navigator or a quick chat with a trusted friend. You deserve clear answers, compassionate care, and a treatment plan that respects the life you want to live.
What part of the treatment journey excites or worries you the most? If you have questions, feel free to ask—knowledge is a powerful ally in the fight against cancer.






















Leave a Reply
You must be logged in to post a comment.