You’re not alone if your lower back pain feels like a constant fight with gravity… and it’s winning. We’re talking about that sharp, unrelenting discomfort in your hip, groin, or lower back that flares when you try to sit, stand, or even just breathe through another sleepless night. Yeah, we’ve been there. And yeah… sacroiliac joint fusion might be the answer.
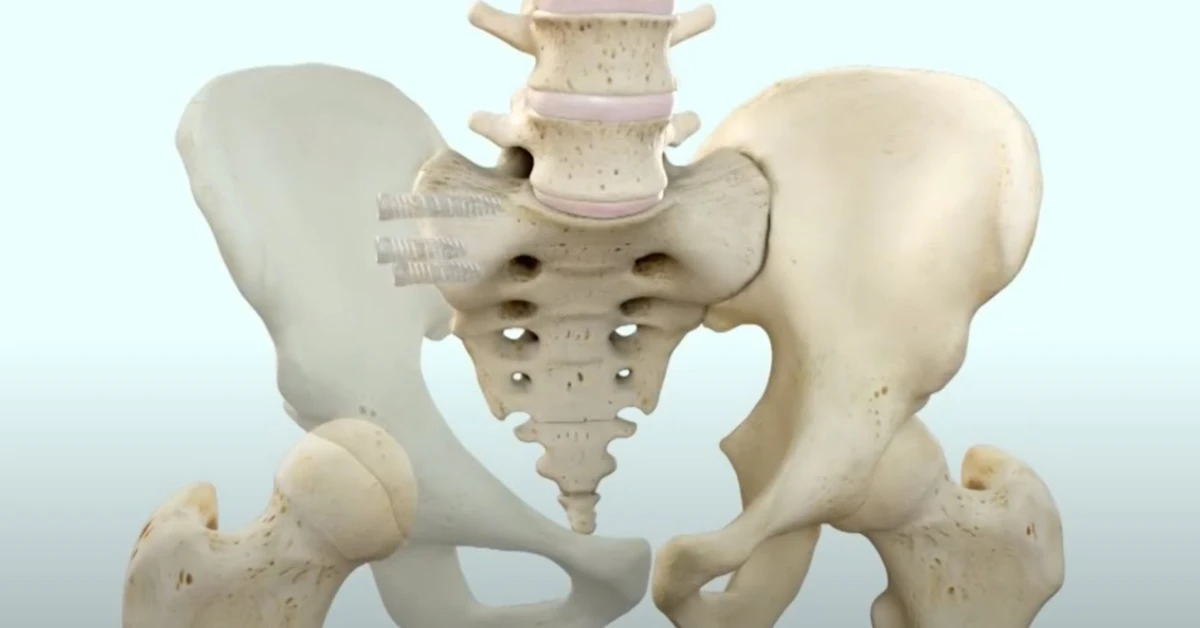
Hold up—what’s the deal with your SI joint anyway? And why on earth would you want to “fuse” it shut? Let’s break this down without the fluff. Sacroiliac joint fusion is a minimally invasive surgery where surgeons permanently lock your sacrum (that cone-shaped spine chunk at your pelvis) to your ilium (hip bones that connect to the sacrum). Why do it? Because movement in an inflamed or misaligned SI joint screams “ows” every time you walk. So, fusing it shuts off the pain signals like unplugging a loud alarm.
What Is SI Joint Fusion?
Sacroiliac (SI) joint dysfunction—aka the pain-in-the-butt name—refers to the inflammation or instability in the SI joint. Where’s that? Right there in your lower back dimples. Most researchers agree this joint can be responsible for 15-25% of chronic low back pain cases as Spine Health Org pointed out in 2024. If your pain-ridden SI joint socks it to you despite physical therapy, PT belts, or even steroid injections, your doc might start chatting fusion.
Wait, Fusing a Joint—What Does That Mean?
Clinically? Fusion means turning two moving bones into one, solid structure. Like gluing Legos together so they stop shifting. Think of it as giving your SI joint a seatbelt for good.
Minimally invasive sacroiliac joint fusion is now the gold standard. Sure, older open surgeries required massive incisions and muscle destruction, but now it’s a one-inch cut and titanium implants holding the pieces together. The first time I saw the iFuse Implant System getting packed into a skeleton, it looked like uninvited tech—but hey, it works.
Can This Surgery Fix My Chronic Pain for Good?
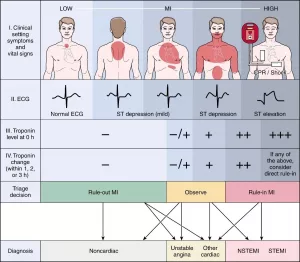
- Yes—if the SI joint is the real pain villain, not a hip or spine issue.
- No—if your pain tripwire’s somewhere else. That’s why specialists lean on diagnostic injections first.
Still skeptical? Surgeons like David Yingling over at Cape Neurosurgical say performance rates? About 95% of folks see a difference. Short story: Cara Strickland, a fusion patient, described her recovery as going from “light-headed pain to hiking again.” So… outcomes are mixed, but promising.
Candidate Diagnosis

If you’re raising your hand at these signs—like your back’s throwing fire alarms even when you’re at rest—you’re in the candidate zone. Medtronic surgeons put it like this:
Common Symptoms to Watch For
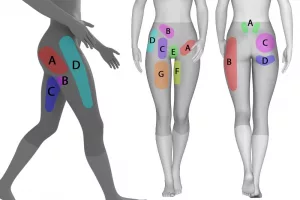
- Severe low back pain (radiates to hip/groin, stays below L5 in placement)
- Sleep destruction because rolling onto that side feels like sitting on a barbed wire fence
- Two or more failed SI injections that shut down pain by at least 75%
- Persistent instability—and patients often describe their leg “buckling” like it’s made of Jell-O
Risky to jump to surgery if your symptoms include numb legs or sciatic zingers—hip issues or disc problems could ride shotgun. The keyword here: wire your surgeon into doing diagnostics before reaching for the fusion button.
The Procedure Explained
SI joint fusion surgery is fast. Surgeons lean toward outpatient procedures these days—no bedhead, no IV vine in your arm for days. So, what happens during the minimally invasive sacroiliac joint fusion beats those traditional open surgeries that were a real mess.
Step 1: You Get Put to Sleep
Yep, general anesthesia sweeps you into dreamtown. You’re face down while the surgical gods prep your skin with antiseptic glue and make a dime-sized cut. No scaling, no muscle cutting here—they chart a path through soft tissue blues.
Step 2: Peek into the SI Joint
The Rialto™ SI Fusion System uses X-rays to position titanium rods those gears right across the joint. Bone surfaces get scraped clean so fresh cells fuse across.
Step 3: Implants or Bone Grafts?
Some systems (like the iFuse Implant System, used in spinal minimal surgeries) don’t need a bone graft. Others, like the Rialto, pack a bone graft into the implant to supercharge the healing process. Why the change-up? Implants vary… your bone quality varies… talk to a surgeon with experience (your spine doc should be grinding those gears, not you).
Benefits vs. Risks
This surgery can be your golden ticket back to doing life again. But it’s not risk-less. If there’s one thing I recommend holding tight, it’s balancing the pros and the “but-what-ifs.”
Here’s Why It’s the ATG Option
- Pain Packed: After the 48-hour mark, 75% say it softens the constant throb. One study tracked pain takes a 75% hit for over six months.
- Movability Spurt: Game of twister again? Fused SI joints don’t mean you’re a statue. Most bounce back to walking, socializing, and—even better—ditching the cane or hip brace.
- Surgical Savvy: No ripping open the pelvis like older methods. The minimally invasive version gets you off the table and into recovery fast. Most people go home within 12–24 hours (some even same-day).
But Let’s Not Whisper This
You’ve got two legs—the surgery might miss its mark entirely and you’re still stuck with that same haunting ache. So what gives? Here’s the run-down:
- Nerve Root Feelings: The surgeon might snag a nerve root near the SI joint. Knife plays near the vibe line to your legs—so any shift could mean tingling or numb patches. Not common, but doctors need to show you the openness.
- Infection Possibility: ’bout 1% of patients get the fever flare-up. But surgical brethren make that rare by using strict protocols like pre-and-post antibiotic shots.
- Implant Risks: Screws shifting or being rejected—although kids like the concept of robot-grade accuracy here. Fluoroscope lasers and guide pins drop error rates significantly.
| Outcome | Risk |
|---|---|
| 75% pain reduction | 5% complication rate |
| Return to yoga, walking, work | 1% infection rate |
Recovery Timing
Suppose June 1st is the day you say “sign-up for the surgery.” Recoverysville looks like this:
| Time | Expect | Restrictions |
|---|---|---|
| Post-op week | Shuffles to bathroom, lays up a lot | Avoid stair climbing, weight lifting |
| Week 2–3 | Gentle sitting, builds up leg strength | Physical therapy gains traction—start chair-sits |
| Week 6–8 | Hiking for half-mile. Driving the car. Laughing more without cringing. | No contact sports, twisting for work, curls at gym (opt. for light weights instead) |
Patients Who Want Details: “Just Describe the Healing Process”
Patients know healing’s not a light switch. After surgery, your SI fusion goes through this progression:
- Soreness (first five days): Bed rest, neck pillow stack, and Tylenol heaven.
- Crutch Cops (week one to two): Surgeons cracked open not to bear full weight. Crutches or a cane are your mobile props here.
- My Life Again (six weeks in): 73% return to light office work; 40% start randos. If you’re like Cara Strickland’s story from St. Francis’ blog, jogging and half-miles make a cameo at 8–12 weeks.
Non-Surgical Exit Roads
Don’t like the idea of body inherently inviting foreign stuff inside via surgery? Totally normal. Try these first:
– SI Joint Belts: Medical-grade compression for three months can mimic fusion temporarily. If pain vanishes with a tightwear wrap, that probably signals mobility issues.
– Injections: Corticosteroids, NSAID site injections—lightning fast but temporary. Wait for these to give out completely before inserting “failure” into Dr.’s notes.
– Radiofrequency: Cauterize those pain nerve ends. Not fusion-permanent, but no scalpels involved here. Great if you’re not ready to undergo lengthy hospital stays (e.g., you, nursing a newborn in your arms).
When’s Surgery Your Only Play?
- Pain doesn’t let you work. Like, at five months, filing paperwork without meds or breaks isn’t even a trial.
- Imaging tracks instability—inflammation, arthritis—confirmed by injections and joints opening like a fault line.
- Conservative treatments failed meaning one word: chronic. PT three months, braces two, cortisone two-shots—and you still dream about running or sleeping like a baby.
CPT Codes & Insurance Buzz
Now onto documentation vibrations—surgeons hate ghostwriting for insurance. What’s the sacroiliac joint fusion CPT code? You need two terms in here: 27279 (meaning you had the minimally invasive version) and sometimes 27280, if they did both hips. Yep, the coding crutches prevent claims from getting tossed into the circular file.
How to Get Coverage
- Confirm the pain lives in the SI joint, not elsewhere. Your provider uses diagnostic blocks and patients who had at least a 75% pain cut after their injection knows it’s SI joint pain.
- Show docs. “Proof” means six months of failed PT, medication logs, and referring specialist letters.
- Surgeon mentions the word necessary in the medical orders. Insurance doesn’t bite on experimental or vague claims.
A real head scratcher: some companies say it’s “investigational.” Classic form. Your doc will send academic papers to med review. The AAOS (American Academy of Orthopedic Surgeons) puts it this way: “SI joint fusion remains the definite solution following failed conservative approaches.” That’ll give your insurance department chills… only this time, good chills.
Bottom line? Don’t cut corners on this. Having accurate paperwork is everything between fusion appointment confirmed—and fusion appointment rejected.
Real Stories Behind Fusion
I remember chatting with Cara. She leans back and says, “I was pregnant with twins, boss. Fell hard in the third trimester, literally.” Her SI joint misalignment took over her entire postpartum chapter. From “I can’t even sit for a feeding” to “fine to run with them at the park,” her SI joint fused with iFuse implants did wonders.
I asked Dr. Yingling why some folks roll the dice on fusion and others don’t. He counters: “It ain’t even gambling if we dial-in the diagnosis first. Patients with true SI dysfunction, proven by nerve blocks and bone-on-bone inflammation?” Difference is night and day. Five years ago, I’d roll the dice on imaging. Now? CPT-guidance’s solid… and fusion rates are as strong as personalized spatial imaging.
His folks jump into healing like there’s a light at the end of the tunnel.
Think Fusion’s Your Way Forward?
Then do this today:
- Check if your pain tracks above the joint or not (below = more likely SI).
- Get a diagnostic shot—if pain drops 70+%, fusion might be your truth.
- Brush up your DDOS report! Just kidding. Ask for charts, pain logs, and letters from your spine god or ortho nerd to prep insurance and referrals.
Here’s the truth. Sacroiliac joint fusion isn’t for everyone but for select people? It fuelizes. Sure, you can flip the “no way back” talk—and surgery ain’t homeopathic—but if you’re crumbling with pain and docs don’t see a spine or hip villain to pin it to, this could be your staircase to well.
What do you think? (drop a comment below or email me). If you’ve hovered around injections or PT for too long without relief, this is your next playground.
Now’s time. Tag your surgeon. Don’t let pain be your rockstar bio longer than necessary. You done deserve that bridge walk, tram ride, or hospital visit without sweats.
Stay sane out there


















Leave a Reply
You must be logged in to post a comment.