Hey there! If you’re reading this, chances are you—or someone you love—has just started Xpovio (selinexor) and you’re curious (or maybe a little nervous) about the side‑effects that come with the treatment. You deserve clear, honest information right away, not a long‑winded lecture that leaves you scrambling for answers. So let’s get straight to it: what you might feel, why it happens, and the simple steps you can take to stay comfortable and safe while you fight cancer.
Balancing the promise of Xpovio treatment with the reality of side‑effects can feel like walking a tightrope. The good news? Most people experience only mild to moderate symptoms, and there are plenty of proven tricks—plus a supportive medical team—to keep those symptoms in check. Ready? Let’s dive in together.
What Is Xpovio?
Xpovio (generic name selinexor) is an oral cancer medicine that belongs to a class called Selective Inhibitors of Nuclear Export (SINE). In plain language, it blocks a protein called XPO1 that cancer cells use to “export” tumor‑suppressing proteins out of the nucleus. By shutting that door, the drug lets the cell’s own defenses trigger apoptosis (programmed cell death) in the cancer cells while sparing most healthy cells.
The drug is FDA‑approved for two tough‑to‑treat cancers:
- Relapsed or refractory multiple myeloma (MM)
- Relapsed or refractory diffuse large B‑cell lymphoma (DLBCL)
According to the FDA prescribing information, Xpovio is taken as a tablet once or twice a week, usually in combination with bortezomib and dexamethasone (often called the XVd regimen).
Why Side Effects Occur
Every medication has a trade‑off, and Xpovio is no exception. Because it interferes with a fundamental cellular transport pathway, it can also affect healthy cells—especially those that divide quickly, like blood‑forming cells in the bone marrow and cells lining the gut. That’s why you’ll hear talk of “low blood counts,” “nausea,” and other symptoms.
Think of Xpovio as a diligent gardener who pulls out weeds (cancer cells) by cutting off their water supply. Occasionally, the garden hose (your normal cells) gets nudged, too, resulting in a few extra drips that you notice as side‑effects.
Common Side Effects
Below is a quick snapshot of the side‑effects most patients report. The percentages come from the pivotal Xpovio + Vd clinical trial and are rounded for readability.
| Side Effect | How Often? | Simple Management Tips |
|---|---|---|
| Fatigue / Tiredness | ≈ 59 % | Schedule short rest breaks, stay hydrated, light exercise (walks) when you can. |
| Nausea | ≈ 50 % | Take prophylactic anti‑emetics (e.g., ondansetron) before the dose; sip ginger tea. |
| Diarrhea | ≈ 32 % | BRAT diet (bananas, rice, applesauce, toast) and loperamide as needed. |
| Loss of Appetite / Weight Loss | 35 % appetite ↓, 26 % weight ↓ | High‑calorie smoothies, small frequent meals, discuss appetite stimulants with your doctor. |
| Anemia (low red blood cells) | ≈ 20‑30 % | Check CBCs regularly; iron supplements or ESA may be advised. |
| Blood‑Sugar Rise | Variable | Monitor glucose, especially if you have diabetes; talk to your endocrinologist. |
Most of these are manageable with a few lifestyle tweaks and, of course, open communication with your oncology team.
Serious Side Effects
While the majority of patients tolerate Xpovio well, a handful do encounter more serious issues. Knowing the warning signs can make all the difference.
- Low Platelet Count (Thrombocytosis): Can cause easy bruising or bleeding. If you notice pink spots, nosebleeds, or prolonged bleeding from a cut, call your doctor immediately.
- Low White‑Cell Count (Neutropenia): Heightens infection risk. Fever, chills, or a persistent cough? Seek prompt medical care.
- Serious Infections / Sepsis: Symptoms include high fever, rapid breathing, confusion, or a feeling of “being really sick.” This is an emergency—go to the ER.
- Neurologic Effects: Dizziness, fainting, hallucinations, or sudden confusion. Until you know how Xpovio affects you, avoid driving or operating heavy machinery.
- Hyponatremia (Low Sodium): Weakness, headache, or seizures. Lab checks will catch this early.
- Eye Changes (Cataracts, Blurred Vision): Any new visual disturbance warrants an eye exam.
According to the Xpovio safety data, serious adverse reactions appeared in about 52 % of trial participants, and fatal events in roughly 6 %. That sounds high, but remember that many of those patients were heavily pre‑treated and had aggressive disease. Your doctor will weigh the benefits against these risks every step of the way.
Managing Side Effects
Let’s get practical. Below are everyday strategies you can start using today.
Before You Begin
- Baseline Labs: Complete blood count (CBC), comprehensive metabolic panel (CMP), electrolytes (especially sodium), and a quick eye check.
- Vaccinations: Flu and pneumococcal vaccines reduce infection risk—talk to your nurse about timing.
- Medication Review: Share every over‑the‑counter drug or supplement with your oncologist; some can worsen nausea or interact with anti‑emetics.
Day‑to‑Day Tips
- GI Comfort: Take Xpovio with a light snack, not on an empty stomach. Keep ginger candies, peppermint tea, or a glass of cold water handy.
- Blood Count Monitoring: Aim for CBCs every 1‑2 weeks at the start, then spacing out as your counts stabilize. If platelets drop below 50,000/µL, your doctor will likely hold the dose.
- Infection Prevention: Wash hands often, avoid crowded places when your neutrophil count is low, and carry a rescue antibiotic prescription if your team recommends it.
- Neurologic Safety: When you feel light‑headed, sit down first. Use grab bars in the bathroom; consider a cane if balance is shaky.
- Hydration: Aim for at least 8 glasses of water a day (more if you have diarrhea). Dehydration worsens nausea and can affect kidney function.
When to Call Your Doctor (Red‑Flag Checklist)
- Uncontrolled bleeding or bruising
- Fever ≥ 38 °C (100.4 °F) or chills
- Severe or persistent vomiting/diarrhea (more than 3 days)
- Sudden vision changes, eye pain, or halos around lights
- New or worsening confusion, dizziness, or fainting
- Rapid weight loss (> 5 % in a week) or loss of appetite that makes you skip meals
Having a short script ready—like “I’m on Xpovio and I’m experiencing ___—what should I do?”—can make phone calls less stressful.
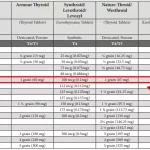
Dosage & Treatment Adjustments
Xpovio comes in 20 mg, 40 mg, 50 mg, and 60 mg tablets. Doctors typically start at a dose that balances efficacy with tolerability, often 40 mg once a week, but regimens vary based on your prior therapies and overall health.
When Dose Changes Happen
- Grade 3‑4 Thrombocytopenia (platelets < 50,000/µL): Hold the dose until counts recover, then restart at a lower strength (usually 20 mg less).
- Persistent Nausea: Add a second anti‑emetic (e.g., metoclopramide) and consider a slower titration schedule.
- Severe Fatigue: Shorten the interval (e.g., from weekly to every 10 days) or reduce the dose by 20 mg.
A real‑world example: Maria*, a 62‑year‑old with multiple myeloma, started on 60 mg weekly. By week three she was exhausted and her platelets dipped to 48,000. Her oncologist paused the drug, gave a platelet transfusion, and resumed at 40 mg every ten days. Within a month her energy improved, and her disease continued to respond. (Names changed for privacy.)
Resources & Support
Knowledge is power, but you don’t have to go it alone.
- Official Patient Kit: The Xpovio website offers a downloadable PDF that outlines dosing, lab schedule, and coping tips—grab it here.
- Support Groups: Many cancer centers host virtual meet‑ups for patients on Xpovio. Hearing others’ stories can normalize the experience.
- Side‑Effect Tracker Apps: Apps like “CancerCare” let you log daily symptoms and share the report with your care team in one click.
- Professional Advice: If you can, set up a brief phone consult with an oncology pharmacist. They specialize in medication‑specific counseling and can fine‑tune your anti‑emetic regimen.
Conclusion
Starting Xpovio is a brave step toward controlling a challenging cancer. Yes, side‑effects are part of the journey, but they are usually predictable and, more importantly, manageable. By staying proactive—monitoring labs, using simple home strategies, and keeping an open line with your medical team—you give yourself the best chance to stay on treatment and benefit from its anticancer power.
Remember, you’re not alone. Your doctors, nurses, pharmacists, and the countless patients who have walked this path before you are all part of your support network. If you have questions, jot them down and bring them to your next appointment. If you’ve found a tip that works for you, share it in the comments—your experience could be the exact reassurance someone else needs.
Stay hopeful, stay informed, and keep fighting. You’ve got this!













Leave a Reply
You must be logged in to post a comment.