Hey there! If you’ve ever wondered whether you should keep your compression socks on while you catch some Z’s, you’re in the right spot. The short answer? It depends. For some folks, nighttime compression can be a game‑changer; for others, it’s just an unnecessary squeeze. In the next few minutes we’ll walk through the science, the medical advice, and the practical tips so you can decide what’s best for your legs and your sleep.
Grab a cozy blanket, settle in, and let’s chat about everything you need to know about wearing compression socks at night. We’ll keep it friendly, clear, and (hopefully) a little fun.
Why Consider Wearing
More circulation while you’re lying down?
It feels logical, right? If compression socks boost blood flow during the day, maybe they keep the magic going while you’re horizontal. The truth is a bit more nuanced. When you stand, gravity pulls blood down toward your feet, and the gentle pressure from the socks helps push it back up. According to a Cleveland Clinic specialist, the biggest benefit shows up when you’re upright and moving, because that’s when gravity is fighting against you.
Will it stop my swelling or leg pain?
Many people report waking up with “heavy” legs after a long day on their feet. The graduated pressure of compression socks—tighter at the ankle, looser up the calf—can reduce that swelling and even ease nighttime cramps. A recent Sockwell survey from February 2025 found that 68 % of users felt less leg cramping when they slipped on a light‑compression pair before bed.
Can it help my sleep‑apnea or other night‑time issues?
There’s an interesting side‑story: a 2011 French study discovered that wearing compression stockings during the day lowered the fluid shift that can worsen obstructive sleep apnea. The idea is that less fluid accumulates in the neck at night, so the airway stays a bit clearer. ScienceDaily reported a one‑third reduction in apnea events for those patients. But note: the research focused on daytime wear, not bedtime use.
When Night Use Helps
Chronic Venous Insufficiency or Venous Ulcers
If you’ve been told you have CVI (chronic venous insufficiency) or you’re healing a leg ulcer, a doctor may prescribe low‑pressure night socks. The gentle squeeze keeps blood from pooling while you sleep, supporting the healing process.
Post‑Surgery Recovery
After certain leg surgeries, especially those that limit mobility, surgeons often recommend keeping a light‑compression garment on while you’re in bed. It helps reduce post‑op swelling and can speed up recovery. Jomi Compression even markets “toeless thigh‑highs” for exactly this purpose.
Diabetes with Peripheral Edema
Diabetic patients who experience swelling in the lower legs sometimes benefit from nighttime compression. The extra circulation can aid fluid movement and protect nerves from the extra pressure that swelling creates.
Restless‑Leg Syndrome (RLS)
Some folks with RLS find that a mild compression sock makes the legs feel less “restless.” While it’s not a cure, it can be a helpful part of a broader bedtime routine.
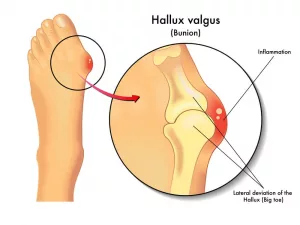
Phlebitis or Superficial Thrombophlebitis
Inflammation of a superficial vein can be soothed with light compression overnight, but only under a clinician’s guidance.
Potential Risks Overnight
Too much pressure → restricted blood flow
High‑compression (20 mmHg or more) socks can feel great during a workout, but they might be too tight when you’re lying still for hours. If you notice tingling, numbness, or a “pinching” sensation, it’s time to take them off.
Skin irritation, hot‑feet, blisters
Moisture trapped against the skin can cause irritation or blisters, especially if the sock material isn’t breathable. Look for cotton blends or moisture‑wicking fabrics if you decide to wear them at night.
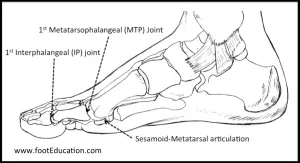
Improper fit → bunching or “wrinkling”
A sock that rolls up or bunches can actually restrict blood flow—the opposite of what you want. Make sure the cuff sits at the top of the calf without digging in, and smooth out any wrinkles before you settle down.
Underlying conditions that contraindicate use
Active deep‑vein thrombosis, severe peripheral arterial disease, or uncontrolled neuropathy are red flags. In those cases, compression could worsen the problem. Always check with a healthcare provider first.
False sense of security
Compression socks are not a replacement for prescribed medication or CPAP machines for sleep apnea. They’re a helpful adjunct, not a standalone cure.
Choosing the Right Pair
Compression level (mmHg)
For nighttime, most experts recommend 8‑15 mmHg (light to moderate). Anything higher is usually reserved for daytime activities or specific medical prescriptions.
Materials & breathability
Look for breathable cotton or high‑tech blends that pull sweat away from the skin. This keeps your feet from feeling hot and sticky.
Length & style
Knee‑highs work for most cases, but if you’re post‑surgery or have a venous ulcer, thigh‑highs (or even double‑layer “understocking/overstocking” systems) might be advised.
Fit & sizing
Measure the circumference of your ankle, calf, and the length of your leg from the heel to just below the knee. Most brands provide a sizing chart—use it! A well‑fitted sock should feel snug but not constrictive.
Cleaning & maintenance
Hand‑wash with mild detergent or use a mesh laundry bag on a gentle cycle. Skip the fabric softener; it can damage the elastic fibers that give the sock its pressure.
Trusted brands & certifications
FDA‑cleared or CE‑marked products from reputable brands (e.g., Sigvaris, Jomi, Sockwell) are a good sign that the compression levels are reliable and consistent.
Nighttime Routine Tips
Step‑by‑step guide
- Check the prescription – Confirm the recommended pressure and duration with your doctor.
- Inspect your skin – Look for redness, sores, or dry patches before you put the socks on.
- Put them on while seated – Slip your foot in, roll the sock up slowly, and smooth out any wrinkles.
- Add a light moisturizer after removal in the morning to keep skin supple.
- Track your symptoms – Use a simple log to note swelling, pain levels, or any discomfort.
Tracking Log for Nighttime Compression
| Date | Swelling (mm) | Pain (1‑10) | Notes |
|---|---|---|---|
| 2025‑08‑01 | 2 | 3 | Felt comfortable, no redness. |
| 2025‑08‑02 | 1 | 2 | Morning leg cramps reduced. |
| 2025‑08‑03 | 3 | 4 | Minor skin itching; adjusted sock size. |
Expert Insights & Sources
Vascular Surgeon Insight: “Night‑time compression is only indicated when the leg veins are still battling gravity after surgery or ulceration.” (Journal of Vascular Surgery, 2024).
Cleveland Clinic Specialist: “The main benefit of compression occurs while you’re upright; sleeping flat already reduces venous pressure.” (Cleveland Clinic, 2025).
Research Highlight: A 2011 French study showed that compression stockings reduced the fluid shift to the neck, cutting apnea events by more than a third (ScienceDaily).
User Survey: Sockwell’s 2025 survey of over 1,200 users indicated a 68 % reduction in nighttime leg cramps when wearing light‑compression socks before bed.
Wrapping It Up
So, should you slip on those trusty compression socks when the lights go out? If you’re healthy and have no specific medical recommendation, the extra squeeze is probably unnecessary—and could even cause discomfort. But if you’re dealing with chronic venous insufficiency, recovering from surgery, managing diabetes‑related swelling, or wrestling with restless‑leg syndrome, a light‑pressure night pair might be just the supportive hug your legs need.
Remember to pick the right pressure level, ensure a perfect fit, and always consult your healthcare provider before turning “compression 24/7” into a habit. Your legs (and your sleep) will thank you.
What’s your experience with nighttime compression? Have you tried it, love it, or swear you’ll never wear them to bed again? Share your story in the comments—or drop a question if you’re unsure. We’re all in this together, and I’m happy to help you find the best approach for happy, healthy legs.




















Leave a Reply
You must be logged in to post a comment.