Hey there! If you’ve been Googling “an ankle replacement eligibility,” you’re probably wrestling with a lot of medical jargon, endless lists of “must‑haves,” and worries about whether you’re even a candidate. Let’s cut through the noise right now: you’re a good candidate if you have severe ankle arthritis that won’t quit, you’ve tried at least six months of non‑surgical care, you’re skeletally mature, and you don’t have any of the red‑flag health issues listed below. If you tick most of those boxes, you’re probably on the right track. And if you don’t, don’t panic—there are other paths, and we’ll walk through those, too.
Understanding the eligibility checklist isn’t just a bureaucratic exercise; it’s a way to avoid unnecessary doctor visits, set realistic expectations, and make the most informed decision about your foot health. So grab a coffee, get comfortable, and let’s demystify ankle replacement together.
What Eligibility Means
Defining Total Ankle Arthroplasty (TAA)
Total ankle arthroplasty—aka ankle replacement—is a surgical procedure that swaps out the diseased surfaces of the tibia and talus for a prosthetic joint. Think of it like a high‑tech shoe insert that actually moves with you, preserving range of motion while taking the pain away.
Why the Eligibility Checklist Matters
Unlike ankle fusion, which locks the joint solid, a replacement relies on a clean surgical field and solid bone stock. The more “clean” the situation, the higher the chance the prosthesis will last and the lower the risk of complications. In other words, the eligibility checklist is the safety net that protects both you and your surgeon.
Core Medical Criteria
Age & Skeletal Maturity
You need to be at least 18 years old, with growth plates fully fused. This requirement isn’t about “age” per se; it’s about making sure the bones are stable enough to hold an implant. As Aetna’s policy notes, skeletally mature patients have a much better platform for long‑term success.
Pain & Functional Limitations
Moderate‑to‑severe pain that interferes with daily activities is a key trigger. If you can’t walk your dog without wincing, or the stairs feel like a mountain, that’s a signal. The pain has to persist despite at least six months of physical therapy, orthotics, and possibly NSAIDs. In short: “You’ve tried everything else, and it still hurts.”
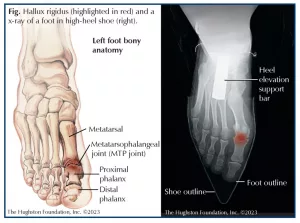
Imaging Confirmation
Radiographs (or sometimes CT/MRI) must show clear signs of advanced arthritis—think narrowed joint space, bone spurs, and subchondral sclerosis. These images prove the ankle is “ready” for a prosthetic and help the surgeon plan the exact size of the implant.
Failed Conservative Management
Doctors want to see that you gave non‑surgical treatments a fair shot. That usually means:
- At least 6 weeks of supervised physical therapy.
- Custom braces or orthotic inserts.
- Injections—corticosteroids are okay, but they must have been administered more than 12 weeks before surgery (to avoid interference with healing).
Overall Health & Bone Quality
Strong, healthy bone is essential. A bone density test (DEXA) should show a T‑score better than ‑1.0. Severe osteoporosis or osteopenia can cause the implant to loosen.
Expert Insight
Dr. Ryan N. Lawrence, DPM, tells us, “These criteria aren’t arbitrary—they’re the result of decades of data. When a patient meets them, we see survivorship rates of 90 % at five years.” That’s the kind of real‑world experience that builds confidence.
Common Contra‑indications
Structural Deal‑Breakers
Even a tiny missing piece of bone can derail the procedure. The most common structural red flags include:
- Absence of the medial or lateral malleolus.
- Severe varus/valgus deformity that can’t be corrected with a simple osteotomy.
- Charcot joint (neuropathic arthropathy).
Infection & Soft‑Tissue Issues
Active infection in the ankle, ulcerated skin, or poor circulation (think “bad blood flow”) is a big no‑no. The prosthetic needs a clean, well‑vascularized pocket to heal.
Bone‑Related Problems
Avascular necrosis of the talus, prior ankle fusion, or any previous surgery that stripped away too much bone can make cementing a new joint impossible.
Systemic Health Concerns
Uncontrolled diabetes, severe peripheral neuropathy, or major cardiovascular disease increase the chance of postoperative complications. Those conditions don’t automatically disqualify you, but they do demand meticulous pre‑op preparation.
Lifestyle Factors
High body‑mass index (BMI > 35), smoking more than a pack a day, or a job that involves high‑impact activities (like construction work) can all raise the odds of implant failure.
Authority Note
According to the Presbyterian health‑plan policy, any of the above conditions listed as “contra‑indications” means the surgery isn’t medically necessary until the issue is resolved.
Special Situations
Mild Deformity or Misalignment
Not all deformities are show‑stoppers. A slight varus/valgus can sometimes be corrected with a concurrent osteotomy (bone cut) before the prosthesis is placed. This “combo” approach lets patients who are otherwise good candidates still move forward.
Prior Ankle Fracture or Hardware
If you’ve had a broken ankle with plates or screws, the surgeon may need to remove that hardware and possibly graft bone before the new joint can be seated. It adds a step, but it’s doable in many cases.
Revision Ankle Replacement
Sometimes a first‑time prosthetic fails—maybe it loosens or gets infected. Revision surgery is a separate set of criteria, but if you met the original eligibility and the failure wasn’t due to a contraindication, you might be a candidate again.
Elderly Patients
Age over 80 isn’t an automatic exclusion. If you’re otherwise healthy, have good bone density, and understand the rehab timeline, many surgeons will still recommend a TAA because it preserves joint motion—something an ankle fusion can’t provide.
Risks vs. Benefits
Top 5 Risks of Ankle Replacement
| Risk | Typical Frequency | Mitigation |
|---|---|---|
| Infection | 1‑3 % | Pre‑op antibiotics, meticulous wound care |
| Implant loosening | 5‑10 % | Proper bone stock, activity modification |
| Nerve or vascular injury | <1 % | Experienced surgical team, careful dissection |
| Wound‑healing problems | 2‑4 % | Control diabetes, stop smoking |
| Need for revision surgery | ~7 % | Follow rehab protocol, avoid high‑impact sports |
Why the Benefits Often Outweigh Those Risks
When you qualify, you typically enjoy:
- Pain relief—most patients report a 70‑80 % drop in pain scores.
- Preserved range of motion—unlike fusion, you can still point your toes.
- Faster return to daily activities—many walk without crutches within 6‑8 weeks.
Those advantages are why surgeons spend so much time perfecting the eligibility checklist—it protects you from unnecessary risk while delivering a life‑changing benefit.
Preparing for Your Eligibility Evaluation
Gather Your Records
Before the appointment, pull together:
- Recent X‑rays, CT or MRI scans.
- Physical‑therapy notes outlining the exercises you’ve tried.
- Lab results (especially blood sugar and bone density).
- A list of all medications, including over‑the‑counter pain relievers.
Questions to Ask Your Surgeon
Turn the appointment into a two‑way conversation. Here are a few prompts you might use:
- “What is my bone stock like on the imaging?”
- “If I lose 20 lb, does that improve my chances?”
- “What does the rehab timeline look like for someone my age?”
- “Are there any hidden costs I should plan for?”
Pre‑Op Lifestyle Tweaks
Even small changes can make a big difference:
- Lose 10‑15 % of body weight if your BMI is above 30.
- Quit smoking at least 4 weeks before surgery (your blood vessels will thank you).
- Keep blood glucose under 150 mg/dL if you’re diabetic.
- Start a low‑impact cardio routine (like swimming) to keep the muscles around the ankle engaged.
Real‑World Success Story
Maria, a 58‑year‑old teacher, was told she was “borderline” because of a 35 % excess weight. She worked with a dietitian, lost 25 lb, and after a repeat DEXA scan showed improved bone density, she was cleared for surgery. Six months later she’s back on her classroom legs, teaching without a cane, and says the whole process was “worth every ounce of effort.” Stories like Maria’s illustrate how proactive preparation can shift you from “maybe” to “definitely.”
Alternative Options
When Fusion Beats Replacement
If any of the contraindications are present—especially active infection, severe bone loss, or a BMI > 40—ankle fusion (arthrodesis) may be the safer route. Fusion eliminates motion but provides excellent pain relief and stability for the right patient.
Non‑Surgical Paths Still Worth Trying
Don’t dismiss the power of conservative care entirely. Consider:
- Custom orthotics that off‑load the painful joint.
- Intra‑articular hyaluronic acid injections (still experimental but promising for some).
- Targeted strength training for the surrounding musculature.
Sometimes a combination of these measures postpones surgery for years, buying you time to optimize health before a big operation.
Expert Resources & Further Reading
Trusted Guidelines
For those who love the nitty‑gritty, the following sources lay out the official medical‑policy criteria:
- Aetna Clinical Policy Bulletin #0645 (covers age, pain, imaging, and contraindications).
- Presbyterian Health‑Plan Policy 20.10 (details bone quality and infection rules).
- Cigna Coverage Position 0285 (FDA‑cleared implants and patient‑selection standards).
Professional Societies
The American Orthopaedic Foot & Ankle Society (AOFAS) and the Orthopaedic Trauma Association publish up‑to‑date consensus statements on ankle arthritis surgery. Checking their websites can give you confidence that the information you’re reading reflects the latest research.
Verify Implant Approval
All prosthetic systems used in the U.S. must be FDA‑cleared. You can confirm a brand’s status on the FDA’s database—just search the device name and look for the “510(k)” clearance number.
Takeaway
In a nutshell, ankle replacement eligibility hinges on three pillars: medical necessity, absence of contraindications, and overall health readiness. If you meet the core criteria, have no major red flags, and are willing to fine‑tune your lifestyle, you’re likely a solid candidate. Armed with this checklist, you can walk into your surgeon’s office feeling empowered, ask the right questions, and make a decision that aligns with your goals.
Want to dive deeper? Download our free Ankle Replacement Eligibility Checklist (PDF) and schedule a consultation with a board‑certified foot‑and‑ankle specialist. Your journey to pain‑free steps starts with the right information—and you’ve just taken a big step forward.























Leave a Reply
You must be logged in to post a comment.