You know that feeling when you’re handed a parenting manual that says everything will magically fall into place after your baby arrives? Right? If you’re a new parent, you’re probably snorting coffee through your nose right now. Because here’s the truth: postnatal depression (PPD) feels less like a manual and more like a choose-your-own-adventure book with plot twists nobody warned you about.
But let’s cut through the noise. If you’re here, it’s because you’re curious—or desperate—about treatment options. You might’ve already tried antidepressants for depression, wrestling with side effects that made you crave a nap more than your baby craves milk. Or maybe you’ve heard whispers about neurosteroid drugs and their “magic” effects on the GABA system, like your brain’s finally getting a cup of tea and a foot massage. But what’s the real deal? Are these new postpartum depression remedies as groundbreaking as they seem? Let’s unpack this gently, like peeling an onion, but without the crying… or at least, not the onion kind.
Antidepressants: The OG Remedy with Ups and Downs
Antidepressants for depression have been around the block. For moderate-to-severe postnatal depression, they’re the go-to—selective serotonin reuptake inhibitors (SSRIs) like sertraline or escitalopram. I get it: they’re the reliable, if slightly slow-moving, subway train of mental health treatment. They work… eventually.
But here’s the hitch: they might take weeks to kick in. Weeks when you’re surviving off lukewarm coffee and guilt about neglecting your baby’s laundry. SSRIs also come with side effects that can make you feel like a malfunctioning robot. Fatigue? Check. Low libido? Double check. Oh, and for breastfeeding parents? There’s the lingering question of how these drugs pass through milk. A study in PubMed found that fluoxetine, an SSRI, boosts GABA(A) receptor activity, which might explain some of its effects—but we’ll dive deeper into GABA in a bit.
What Even Are SSRIs, and Why the Wait?
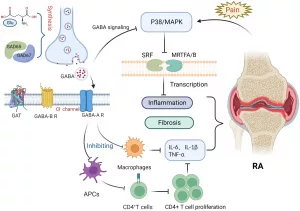
Simple answer: SSRIs tweak your brain’s serotonin system, the stuff that makes you feel calm and happy. But—fun fact!—your gut is also loaded with serotonin. So when people say “serotonin is key,” they’re only telling half the story. The GABA system, that calming neurotransmitter, is calling shotgun here.
Still, the FDA hasn’t officially said, “Antidepressants for depression? Mission Accomplished!” Picture it as a puzzle missing a few pieces. Some folks get relief; others feel stuck in the same cloudy haze.
Neurosteroid Drugs: The New Kid on the Block
Cue the neurosteroid drugs. These little warriors target the GABA system—your body’s natural chill pill. Brexanolone, the IV-infusion poster child, showed a 30-day improvement in depression scores in clinical trials. Flashy, right? And zuranolone, the very first oral treatment approved by the FDA on August 4, 2023, promises faster fixes: take a 50mg pill with a fatty meal, repeat for two weeks, and possibly feel like a real human by Day 15.
But wait! If you’re thinking, “Okay, PAYDAY,” let me add… the science isn’t crystal clear yet. These drugs modulate GABAA receptors, which get tripped up by hormonal roller coasters after childbirth. Mouse model studies (like this one) even link GABA receptor δ-subunit deficiencies to postpartum mood crashes. Neat, huh? But how does that translate to humans? More on that later.
Brexanolone vs. Zuranolone: What’s the Difference?
Let’s play “Which One Is Which.”
- Brexanolone: Administered in a clinic, gets praised in journals like Frontiers in Psychiatry, but requires hours of IV infusion. Not exactly groceries-and-kids-in-tow convenient.
- Zuranolone: Pop a pill by the bed at night, like a bedtime story in capsule form. FDA-trusted, faster-acting, and specifically designed for postpartum depression remedies. Check recent studies here.
Both drugs are GABAA receptor PAMs—positive allosteric modulators. Fancy term: they help GABA do its job better, like giving your brain a co-pilot.
The GABA System: Your Brain’s Sprinkle of Serenity
GABA—short for gamma-aminobutyric acid—is the calming voice in your head when everyone else is panicking. Think of it as the green velvet cushion in life’s espresso machine: without it, you’re just steam and chaos. But when GABA gets knocked off-kilter? Cue anxiety, insomnia, and that “invisible wall” some mothers hit.
Which brings us to…
Why GABA Gets Derailed After Childbirth
Pregnancy and the postpartum period are hormonal maelstroms. Progesterone drops like a lead balloon, and that’s a big deal because GABA loves progesterone byproducts. When those vanish, the cheese stays gripped tight. Science whispers that deficits in GABAAR plasticity (try saying THAT five times fast) may be why some parents crash into postnatal despair. Mouse studies confirm it—mice with wonky GABAA receptors started acting like emotionally reactive toddlers. You can read more about this
Can Low GABA Increase Your Postnatal Depression Risk?
Psychiatrists say yes. GABA levels tracked in moms-to-be? Turns out lower levels marched lock-step with higher depression scores. Like your little inner calm chanting, “I’m not strong enough to hold this.”
So if antidepressants for depression are like tuning a guitar over weeks, neurosteroids are a swift, just-in-time tuning fork. Quick fixes, but… how long does the magic last?
Mad Libs: Risks vs. Rewards of Postnatal Depression Treatments
Let’s make one thing clear—we’re not here to hype up treatments like they’re hot-sale items on QVC. PPD is too damn serious for that. Instead, we’re slicing through the fluff (you’re welcome) to talk about what matters: balancing postnatal depression treatment with your safety and sanity.
Zuranolone: Fast, But Is It Forever?
The buzz around zuranolone is legit. It’s the first oral treatment specifically for postpartum depression. That convenience factor? Skyrocketing through the roof. However, rapid onset doesn’t mean quick expiration. Trials followed patients for weeks to months, showing sustained improvement. But—plot twist—the studies often lacked racial, socioeconomic, and trauma-diversity in subjects. Oh well. Progress! (Sort of.)
An OB care guide during an August 2023 advisory mentioned moms needing rest and organized sleep—a loophole your sleep-deprived soul applauds. So while the tablets can help the emotional loops spin smoother, self-care is still a co-pilot. Like chocolate and peanut butter, drugs + habits may make a fuller plan.
Is Allopregnanolone the Future?
Brexanolone is a synthetic version of allopregnanolone, which your body already makes. Basically, science is copying natural homework. But—heads up—not every study drops the mic on long-term effects. Nature’s 2023 review raised a valid question: are we just patching symptoms, not the root cause?
“But Did It Work?” A (Not-So-Fictional) Friend’s Story
Meet patient_001, a mom who gave permission to share her brain fog and gradual comeback. Tried-and-true SSRIs? Made her feel like a cartoon ghost—detached, floaty. Switched to neurosteroid therapy in 2023? Dropped her Hamilton Depression Rating from a stormy 24 to a refreshing 9 in 4 weeks. Feeling her baby’s smile finally mattered again was… enough to cry in a good way. But there were lingering side effects. Brain fog didn’t vanish. Still, things stabilized.
Takeaway? Even “breakthrough” drugs like zuranolone won’t rescue you from all pain, but they might offer a seatbelt.
Postpartum Depression Remedies Beyond the Pharmacy
What if drugs aren’t your jam? (No shame there.) Postpartum depression remedies might start in the kitchen or the best yoga mat in your living room. Mom groups, counseling, omega-3 supplements—these cuddle your GABA system without a written script. A Healthline checklist includes movement, diet swaps (swap instant noodles for salmon with gusto?), and squeezing in sleep. “Sleep? When?” you might groan—but the system works when it can. Try scheduling a nap like you schedule your Netflix queue.
Is It Cool to Mix Ephedra-Free
Technically? Yes. Antidepressants for depression modify serotonin; neurosteroids hug GABA. Think of them as twins with totally different interests. One’s into coding and silence; the other loves DJ spins and spontaneous road trips.
Of course, GABA supplements are all-in on this collaborative vibe. They’re the herbal tea of the mental health world—gentle, low-risk, and workable for parents who balk at chemical cocktails. (Though, if you’re on brexanolone, it’s IV-only social time—no snacks.)
So… Are We Trusting Science Yet?
Balance. Balance. Balance.
Brexanolone, zuranolone, and even fish oil: they’re worth your gaze, but no final votes just yet. Still, trends are leaning toward the GABA system being the stealth MVP of postnatal depression treatment. Like finding your baby’s pacifier… right when they need it most. But here’s the rub:
- Antidepressants stay the bedrock for the moderate-to-severe crew.
- Neurosteroid drugs offer hope with fewer emotional wobbles.
- Kitchen-and-mind campaigns? Still underused and underrated.
If you’re in the thick of PPD? Talk to your doctor. Dive into feelings without shame. Says this StatPearls guide, there’s no universal postnatal depression remedy—just what works forYOU™.
Big Brain Fact
Antidepressants and zumasterolone are being compared in clinical trials more intensively than ever. PMCs and a JAMA team shrug and say, “Does this drug work better in the long haul?” They’re hopeful. Neurosteroid therapy’s still in ropes, though—it’s way newer. First IV brexanolone, then 2023’s pill zuranolone. What’s next? Gene edits? Android mothers?
Wrap-Up: Own Your Recovery, But Stay Honest
Let’s end with truth, not a sales pitch. You might’ve landed here because you’re adrift—possibly in the same sticky sweater for days
So if you take one thing from this postnatal depression treatment round-up?
- Antidepressants for depression work for many—just side effects and wait time kind of suck.
- Neurosteroid drugs calm your GABA system screaming “help!”—but data’s-freezing eyebrows still unsure if it’s the final hero.
- Postpartum depression remedies like exercise and quality sleep deserve gold stars—HOLD ON wins, even if small.
Your path is YOUR path. No guilt. No pressure. Just honest, human words and support. Take what resonates. Leave what doesn’t.
So what’s your game plan next week? Slap on a therapist’s schedule, cry-laugh while taking zumasterolone? Or become the boss of small self-care wins? All roads lead to healing.
Curious or overwhelmed? Drop a line. Share your ^stolen sweater battle^. We’re out here—together.





















Leave a Reply
You must be logged in to post a comment.