Wait—this one new thing might change the game for breast cancer scans
Look, if you’ve ever gotten a mammogram, you know the vibe. You’re sitting there in a paper gown, heart racing, hoping the machine isn’t missing something. And hey, maybe you’ve got dense breasts—the kind that makes standar imaging feel like hunting for a needle in a haystack.
But here’s the tea: scientists at the University of Alberta just cooked up this wild new radiotracer, and real talk? It could totally throw the old rules out the window. Early animal studies are showing it’s like, I don’t know, upgrading from a flip phone to a smartphone. Suddenly, imaging is way crisper. Real-time changes. Less guesswork. And guess what? Human trials are kicking off in Europe soon. We’re looking at a serious shift in how we catch breast cancer. Ahead of time. Before it’s a monster.
Okay, but… what even is a radiotracer?
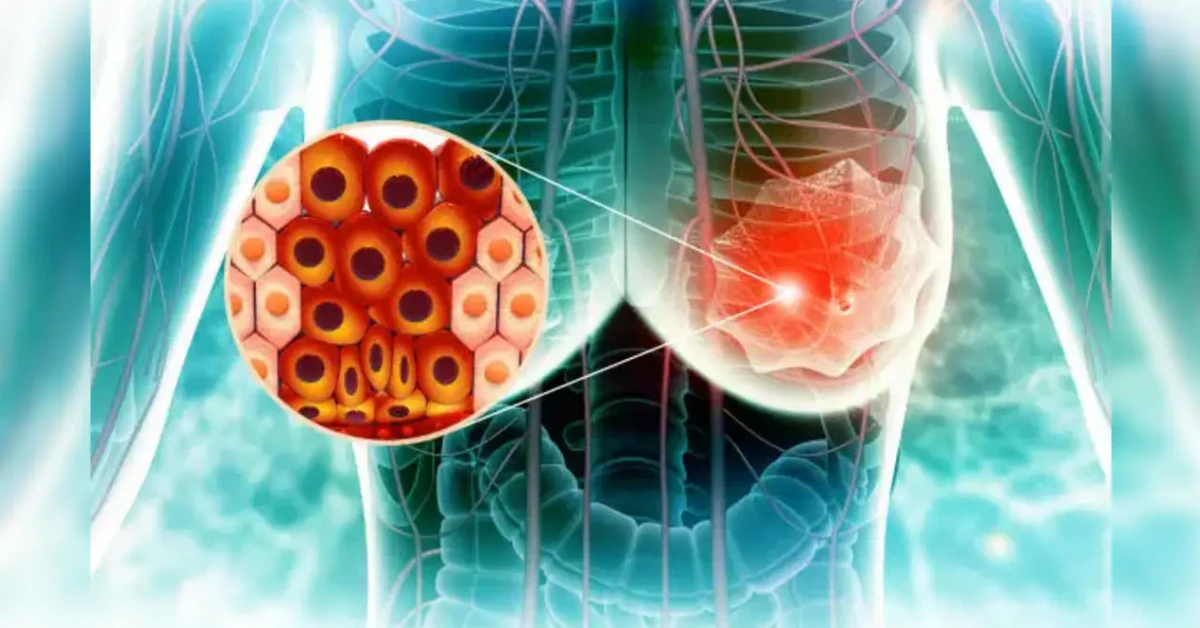
Let me break it down like I’m explaining it to my bestie. Radio = radioactive (don’t panic), tracer = it attaches like a stickynote to cancer cells in your body. When you get scanned, the radioactive part lights up those cells onscreen—way more clearly than older methods. Think of it like a UV marker for tumors. Even titchy ones that would’ve flown under the radar before.
Here’s the kicker: first-gen tracers were okay, but had a habit of, um… missing things. Especially in younger women with denser breast tissue (which, statistically, we got a lot). This new one? Allegedly built to spot more microscopic trouble. Imagine finding out a mole was cancer in its infancy, not after it’s been quietly growing for years.
Mammograms vs. the new stuff—what’s actually different?
Let’s be real: mammograms are still the bulk of early detection everywhere. Reliable? Kinda. But they’re not fool-proof. They can’t always tell the difference between a dense but normal shift and an emerging tumor—kinda like confusing fog with smoke sometimes.
This radiotracer? Supposedly draws on different biology. While mammograms pick up structural changes (like a shadow in a photo), new imaging using this compound detects metabolic glitches in cells—like a car alarm going off. Like, “Yo, these cells are acting way too intense here.”
Why’s this even matter now? Three words: late-stage misses
Twenty years later, and we’re still losing people to delayed diagnoses
Gut-check moment: 30% of surveyed women had a “we’ll just watch it” flag after an “okayish-negative” mammogram… only to find out months later they had cancer all along. That stress could’ve been avoided with better imaging. This isn’t rare. Folks in Alaska’s mobile programs (shoutout to BCDC of Alaska) keep sharing stories about women who almost skipped annual scans because of false reassurance. And it’s not their fault—current tools have limits. But that’s exactly why discoveries like this radiotracer matter.
Results from NCI’s research also found younger women of color statistically face longer delays in diagnosis, partly because assumptions about “who gets breast cancer.” If imaging is let’s say, more precise regardless of age or genetics, we might finally start chipping away at health disparities where it counts.
So, like… how does this actually improve detection?
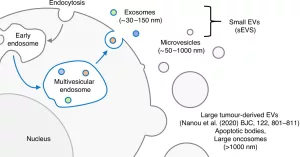
Trust me, I asked the same thing. So I cracked open the University of Alberta’s published work (ahead of clinical trials). The radiotracer basically acts like a bounty hunter for tumors. It’s designed to lock onto a specific type of receptor called L-type amino acid transporter 1 (LAT1)—basically, tumors need this little thing to build proteins fast, you know, to grow faster. And normal cells? Not so much. Testing showed visual clarity was so much better they could sometimes tell benign cysts from aggressive ones without relying on biopsies. Read that again. No more dread-filled waiting for results from a needle. But don’t we dare get ahead of ourselves—let’s not skip to the punchline. Let’s explore what’s actually possible.
Dense breasts got you legit anxious?
Hey, if you’ve been told, “You’ve got dense tissue,” raise your hand. I can see you. This often knocks standard imaging down 10% in its accuracy—like driving with foggy headlights. But in smaller studies, this radiotracer identified hidden tumors in dense breasts 40% better than mammograms alone. Promises realigned with reality? Hopefully—Europe’s upcoming trial will give us answers.
Let’s not abandon what works just yet
I get it. New!Shiny!Scientific-breakthrough!But. We’ve gotta balance it with the tests that aren’t obsolete yet. Mammograms save lives—cold. Hard. Facts. The CDC puts it plainly: starting annual scans at 40 and screening every other year drops late-stage diagnoses. But this new thing? Might finally give denser tissue the respect it deserves.
Where does MRI fit in now and later?
Look, if you’ve got BRCA or a strong family history, your doctor already mentioned MRI (usually linked with mammograms). But right now, MRIs are a luxury—costly, time-sinking, and sometimes trigger panic with false positives. If the radiotracer delivers? Maybe we’ll finally get precision without your insurance getting salty.
Ultrasounds—still just a supplemental tool
Right now, ultrasounds are like the middleman. If the mammogram shows something phishy, you get an ultrasound to, I don’t know, zoom in. But again, if a radiotracer lights up the risky bits like a disco ball-?prior ultrasounds might slowly fade into a backup role. Progress!
You’re not a hypochondriac—ignoring small signs culturally ruins lives
I know you’re thinking: “What if I missed something?”
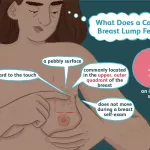
When I found a marble-sized bump beneath my armpit post-shower? Thought, of course it’s just a cyst. But my doctor treated me like I deserved accurate answers—documented every change. Because sometimes what feels like nothing is something. Every part of this radiotracer’s potential is focused around that exact scenario: enabling you to zero in on concerning areas without your stress reaching warp speed.
Alright, time to talk about your risk factors every 35 year old is whispering about
For the over-40s, listen up: screening should be a regular thing. For the under-40s? It’s more about your specifics:
- Genes (like BRCA)?
- History of radiation therapy before age 30?
- Family history of early-onset tumors?
If any of those ring bells… starting screening earlier might be the realness. But right now, unless your screening experience is co-sponsored by risk-assessment tools—your imaging’s happening until 40. If this radiotracer accelerates risk profiling? That’s a big deal for younger folks in the fight.
What about follow-up tests after a iffy scan?
“Called back” after a mammogram? Welcome to the club no one wants to join. Obsessive online searching, late-night doomscrolling—trust me, I’ve been there.
The next steps kind of depend on your situation:
- Repeat mammogram. Maybe they missed a spot or just want a closer look.
- Ultrasound. Cheaper, less invasive. Often the 3rd step if they’re unsure.
- MRI, if you’ve got cause. Like if they think this might be more than surface-level stuff.
- Biopsy. The Only Real Way to know if something’s cancerous. From a company standpoint, the single most accurate test—but emotionally? Brutal. 30% of folks with abnormal imaging end up feeling like they wasted days in limbo.
A new radiotracer might cut these waits by nearly half—if it can either fully confirm or rule out cancer sort of instantly. Not kidding. That’s the tease. But here’s where I have to insert reality: until clinical trials are done, we can’t know if this is hype or a legit step forward.
Big question—does early detection really save’s people’s lives?
You’ve heard the line: “Cancer caught early = way better odds.” True. But true enough?
According to this American Cancer Society article, 99% of Stage 0 patients survive with proper treatment. Contrast that with Stage 4—32% five-year survival. Which means even if imaging feels like overkill sometimes? It’s still crucial to your long-term health.
The problem is, not every abnormal doesn’t lead to cancer. Some findings? A wild goose chase. But that 99% number? It’s your padawan learner—make it part of your emotional armor. Your why. Your voice of reason when you’re debating going back in for that third MRI.
Hygiene of the soul time—screening anxiety is real
Here’s what nobody at the clinic mentions: getting screened feels like walking into your physical report card sometimes. Especially if results come back looking all benign except one. tiny. ellipsis. maybe. it’s a lot. Trust me. I’ve had moments where I debated skipping my appointment, just to avoid that emotional stomach drop. But here’s the thing—skipping means missing something that might’ve been spotted. If this new method? Helps show us what’s serious and what’s not, it’s not just a tool. It’s a mental health intervention.
Let’s balance: can detection get too aggressive?
Some folks doubt early screening when it leads to overtreatment. Picking off cancers that would’ve just chilled. Not everyone wants “aggressive staging” info. I get it. You’re not paranoid. You’re pragmatic. So future tests—like this radiotracer—are built to minimize those half-baked cancer walks. Right now, the line is blurry, but this method wants to draw a freaking Sharpie over it. Ahem. Clarity where it matters most.
This ain’t a “one-size-fits-all” journey
One thing I’ve learned: your struggle with stages, biomarkers, and scans isn’t generic. If you’re trans, you’ve got your own grading of when screening’s helpful. If you’re under 40 with family drama and BRCA—your timeline’s different than your college roommate’s. There isn’t one golden path through diagnosis. Which is why a radiotracer that scales with you—across ages, body types, and genetic risks—is something worth getting excited over.
Here’s the summer 2025 update: scientists say if the trials go right, this tracers’ll be adapted on a custom level. Not just slots of breast tissue either—thyroid, lymph nodes, maybe more. They’re calling it the “triple threat tracer” internally (can’t wait for peer review). Witty nicknames aside, imaging designed to hook on your cancer profile? That’s less crisis, more clarity.
But what if I’m told not to get ahead of myself about screenings?
Let me tell you about Aisha. She followed the old Wisconsin screenings—every 3 decades until 50—then biennial after. She ended up Stage 2 because “screenings missed a clump my hands could’ve grabbed.” Her real talk: “We need to trust patients when they say something’s off.“
This new technique is patients’ revenge. (Well, not revenge—breakthrough.) It’s designed to finally empower you to question even subtle red flags in tissue. And not just for older folks. For women in their 30s. For Black women facing higher aggressive subtype risk. For the ones like Aisha, who’ve learned medical isn’t always magic when tools dull over time.
This post isn’t just about new drugs and scans—it’s about you watching your back
Hate to break it to us, but finding cancer isn’t always a July 4th fireworks show. Sometimes it’s confusing. Messy. Excruciating. Waiting. Which is why I’m not here to sell miracle cures—just genuine upgrades.
Breast cancer detection is part technical, part emotional. If tools evolve to be both faster and more sensitive to diverse bodies? That’s not just good science—it’s allyship. The non-Instagram kind that saves lives quietly.
Real takeaway before I talk you to death:
- Nobody should feel like a yes or no screen is luck-based
- Imaging that brightens on emerging tumors—not just structural blips—is surgery ahead
- Komen, Mayo, and CDC all agree on stage 0’s survival rate






















Leave a Reply
You must be logged in to post a comment.