Hey there, friend. If you’ve landed on this page, chances are you (or someone you care about) are navigating the maze of non‑muscle invasive bladder cancer, aka NMIBC. The name sounds technical, but the core question is simple: what can we do to keep the cancer from coming back and stay as healthy as possible? I’m not a robot—I’m just a fellow human who’s spent a lot of time learning from doctors, patients, and the latest research. So let’s sit down, have a virtual coffee, and walk through the most up‑to‑date NMIBC treatment landscape together.
Why Benefits & Risks
First things first—any treatment comes with a trade‑off. Understanding both sides helps you feel empowered, not scared. Think of it like choosing a new phone: you love the camera, but you might have to give up the bulky charger.
The “go‑to” therapy – BCG
For decades the gold standard has been BCG therapy. BCG (Bacillus Calmette‑Guérin) is a live, weakened strain of the same bacteria used in the tuberculosis vaccine. When we put it into the bladder, it wakes up the immune system to hunt down any stray cancer cells.
When BCG falls short
Unfortunately, about 30‑40 % of patients don’t get a lasting response. Think of it like planting seeds: most sprout, but a few just won’t grow despite the best soil.
Balancing act
All therapies have side‑effects. Some are mild—like a bit of burning when you pee—while others are rarer but more serious, such as infection that spreads beyond the bladder. The goal is to choose a plan where the benefits clearly outweigh the risks.
| Therapy | Key Benefits | Typical Risks |
|---|---|---|
| BCG (intravesical) | High recurrence‑free rates for high‑risk NMIBC; long‑term immune memory | Flu‑like symptoms, cystitis, rare systemic infection |
| Gemcitabine (intravesical) | Effective for BCG‑intolerant patients; milder bladder irritation | Local irritation, mild nausea |
| Hyperthermic Mitomycin C | 44 % higher efficacy when bladder warmed > 42 °C; synergistic drug uptake | Transient urinary urgency, heat‑related discomfort |
| ANKTIVA® + BCG | Provides response in BCG‑unresponsive CIS; bladder‑preserving option | Injection‑site reactions, flu‑like symptoms |
First‑Line Therapies
Intravesical BCG – the classic
BCG is still first‑line for most high‑risk NMIBC. The usual schedule is six weekly “induction” installations followed by a maintenance phase that can stretch up to three years. During each session, a thin catheter delivers the solution, you hold it for 1–2 hours, then you’re free to go about your day.
Why does it work? The bacteria act like a friendly fire alarm, recruiting white blood cells that also target the cancerous cells lurking on the bladder lining. As a result, many patients enjoy a durable remission.
Intravesical Gemcitabine – a solid backup
If you’ve had a reaction to BCG or if BCG supplies are scarce (it’s happened before), gemcitabine steps in. It’s a chemotherapy drug that directly interferes with DNA synthesis in cancer cells. Studies from 2020 show it’s especially useful for low‑risk tumors, delivering about a 70 % response rate with fewer side‑effects than BCG.
Hyperthermic Mitomycin C – heat meets chemo
Ever heard the saying “heat makes things easier”? In bladder cancer, warming the bladder to around 44 °C makes the lining more permeable, letting Mitomycin C soak in deeper. Devices such as EMDA® or the Synergo® radio‑frequency system circulate the heated drug, achieving uniform temperatures across the bladder wall.
Evidence from the UCLH centre and a UK radio‑frequency study showed a 44 % jump in recurrence‑free survival when the bladder stayed above 42 °C (according to a 2024 NEJM study). The side‑effect profile is generally mild—mostly temporary urgency or slight burning.
Emerging Options
ANKTIVA® + BCG – new hope for stubborn cases
For patients whose cancer refuses to budge after BCG, the FDA approved a combo: ANKTIVA® (a recombinant immunotherapy) plus a reduced BCG schedule. The therapy re‑sensitizes the bladder’s immune environment, and trial data show about 60 % complete response at 12 months for carcinoma in situ (CIS) cases.
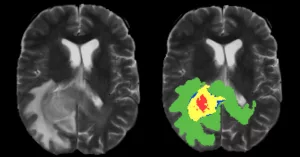
Cysview® Blue‑Light Cystoscopy – see what you missed
This isn’t a drug, but it’s a game‑changer for detection. Cysview makes tumors glow pink under blue light, allowing doctors to spot lesions that white‑light cystoscopy might miss. Detecting and removing every tumor at the first TURBT (trans‑urethral resection) dramatically improves the odds of a successful enhanced immunotherapy plan.
Systemic Checkpoint Inhibitors – for the very resistant
When everything else fails, drugs like pembrolizumab or atezolizumab—originally designed for metastatic disease—can be given intravenously. They “release the brakes” on your immune system, letting T‑cells attack lingering cancer cells. These are NOT first‑line, but they’re valuable lifelines for BCG‑unresponsive NMIBC.
Future horizons – personalized vaccines & CAR‑T
Researchers are experimenting with personalized cancer vaccines that use snippets of your tumor’s DNA, and even CAR‑T cell therapy that engineers your own immune cells to hunt bladder cancer. While still in trial phases, the excitement is real—imagine a future where your treatment is as unique as your fingerprint.
Choosing the Right
Risk‑Stratification Checklist
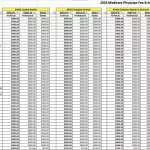
Before any decision, doctors use tools like the EORTC risk tables to grade your tumor’s size, number, grade, and presence of CIS. Here’s a quick cheat‑sheet you can ask your urologist to walk through:
- Is the tumor high‑grade or low‑grade?
- How many tumors are there, and how big are they?
- Is there carcinoma in situ (CIS)?
- What’s your overall health—kidney function, heart health, age?
Patient‑Centric Factors
Maybe you’re a marathon runner who can’t miss many weeks of work, or perhaps you have a busy family schedule. Your lifestyle, tolerance for side‑effects, and personal preferences matter as much as the science.
Shared Decision‑Making Tools
There are decision‑aid apps and printable charts that compare outcomes side‑by‑side. I found one that showed a 75 % 5‑year disease‑free survival with BCG versus 55 % with gemcitabine for high‑risk disease. Visuals like that make the abstract numbers feel concrete.
Sample Dialogue (you & your doctor)
You: “I understand BCG is the standard, but I’m worried about the flu‑like side‑effects. Are there alternatives that fit my schedule?”
Doctor: “Absolutely. We could consider a hyperthermic Mitomycin C schedule that only requires a 90‑minute visit once a week, and the side‑effects are usually milder. If you’re comfortable with a slightly higher cost, ANKTIVA + BCG is another option for BCG‑unresponsive disease.”
Practical Guide
Below is a simple timeline of what you’ll experience before, during, and after each treatment session. Knowing the steps can calm nerves and let you plan your day.
| Phase | What Happens | Patient Tips | Red‑Flag Symptoms |
|---|---|---|---|
| Pre‑procedure | Urine culture, medication review, bladder emptying | Hydrate 2 hours before; avoid NSAIDs | Fever, blood in urine, painful urination |
| During | Catheter insertion, drug/heat instillation, hold 1–2 h | Relax, deep breathing; bring a book | Severe abdominal pain, intense burning |
| Post‑procedure | Flush bladder, monitor symptoms, schedule next visit | Drink plenty of water; keep a side‑effect log | Persistent fever > 38 °C, chills, flank pain |
Key Lifestyle Hacks
- Stay well‑hydrated (but limit caffeine on treatment days).
- Maintain a balanced diet rich in antioxidants—think berries and leafy greens.
- Keep a short diary of any urinary changes; share it with your care team.
- If you’re on blood thinners, discuss timing with your doctor to reduce bleeding risk.
Follow‑Up Strategies
Even after you finish the induction phase, surveillance is the cornerstone of staying cancer‑free.
Cystoscopy Schedule
Typical follow‑up involves cystoscopy at 3 months, 6 months, then yearly if everything looks good. Some specialists add urine cytology or fluorescence cystoscopy (like Cysview) to improve detection.
When to Consider Radical Cystectomy
If the cancer progresses to muscle‑invasive disease (i.e., it starts invading the bladder wall), many urologists recommend removing the bladder—called radical cystectomy. It’s a major surgery, but outcomes are excellent when performed early.
Living Beyond Treatment
Many patients report returning to normal activities within weeks of finishing therapy. A supportive community, whether it’s an online forum or a local support group, can make the journey less isolating. Sharing stories—like yours—helps others feel less alone.
Conclusion
Choosing the right NMIBC treatment is like charting a course on a map: you need a clear destination, a reliable compass, and the courage to keep moving forward. Whether you start with the tried‑and‑true BCG, shift to hyperthermic Mitomycin C, explore the promising ANKTIVA + BCG combo, or keep an eye on future personalized vaccines, the most important thing is to stay informed and partner closely with your medical team.
Remember, you’re not alone in this. Ask questions, weigh the benefits against the risks, and trust that advances in bladder cancer immunotherapy—like tuberculosis vaccine cancer approaches—are continually improving your odds for a healthy future.
What’s been your experience with NMIBC treatment? Have you found a particular therapy that works best for you? Feel free to share your thoughts, and if you have any lingering questions, don’t hesitate to reach out. Together, we’re stronger.





















Leave a Reply
You must be logged in to post a comment.