Hey there, friend. If you’ve ever stared at a medical article and felt a wave of overwhelm, you’re not alone. The term “early lung cancer detection” can sound like a mouthful, but the idea behind it is simple: catch a problem when it’s still tiny enough to treat easily. In the next few minutes we’ll walk through why it matters, who should think about it, what tools are available, and how you can take confident steps toward your health. Grab a cup of tea, settle in, and let’s talk like we’re sitting at a kitchen table.
Why Early Detection Matters
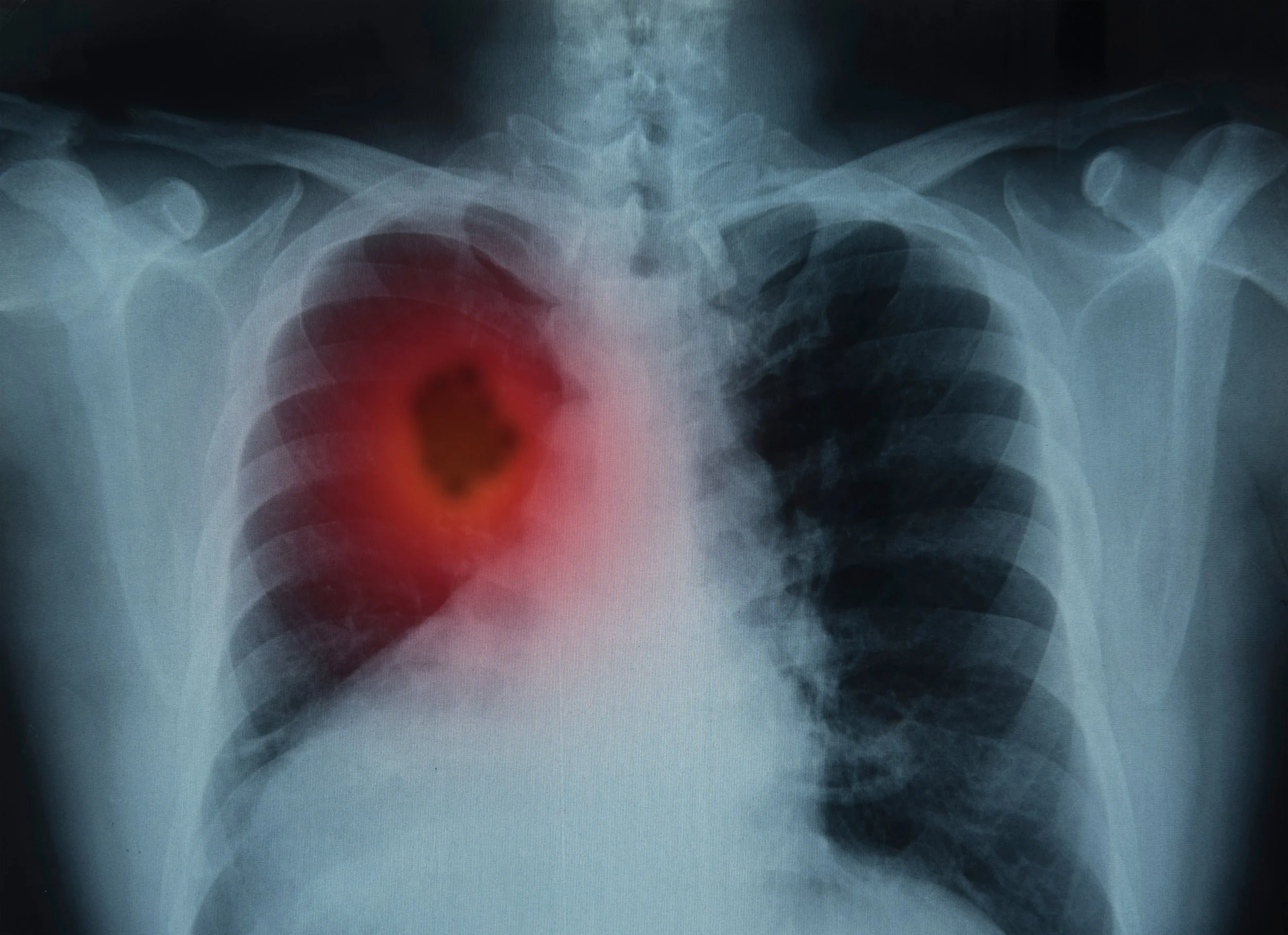
What “early” really means – stage I vs. stage IV survival
Think of cancer stages like the difference between a sapling and a towering oak. When lung cancer is found at stage I, the five‑year survival rate jumps to over 75 %—that’s like a sapling that still has a chance to grow tall and strong. By stage IV, the survival drops below 10 %, meaning the oak has already spread its roots far and wide, making it much harder to pull out.
The hidden cost of late‑stage diagnosis
Late detection isn’t just a line on a statistics chart; it translates into longer hospital stays, more aggressive (and expensive) treatments, and a heavier emotional load for you and your loved ones. In other words, catching it early can spare you a lot of later heartache—and your wallet will thank you, too.
Key Statistic Box
“Every 5 minutes a new lung‑cancer case is diagnosed in the United States.” – National Cancer Institute data.
Who Is at Risk?
Classic risk factors – smoking history, age, occupational exposure
Let’s start with the big three: smoking, age, and the environment. If you’ve ever heard of “pack‑years,” you’ve probably wondered how it works. It’s simple math: the number of packs you smoke per day times the number of years you’ve smoked. Ten pack‑years could be one pack a day for ten years, or two packs a day for five years. Most guidelines say a history of 20 pack‑years (or more) puts you in the high‑risk bucket.
Beyond smoking – radon, air‑pollution, genetics, family history
Even if you never lit a cigarette, other culprits can increase risk. Radon gas seeping from the soil into homes, long‑term exposure to certain chemicals at work, and a family history of lung cancer can all tip the scales. It’s a reminder that “risk” isn’t a single‑track line—it’s a mosaic.
Non‑smoker detection gaps – why many models miss them
Traditional screening programs focus heavily on smokers, leaving many non‑smokers in the shadows. A 2025 study on AI‑driven diagnosis showed that incorporating circulating abnormal cells (CACs) helped spot cancers in never‑smokers that CT alone would have missed. According to the research, adding these biomarkers raised detection sensitivity by 12 % for non‑smokers.
Want to explore more about the underlying causes? Check out our deep dive on smoking and lung cancer and how other factors play a role.
Screening Options Explained
Low‑Dose CT (LDCT) – the gold‑standard
Low‑dose computed tomography (LDCT) is the go‑to test for high‑risk folks. Two massive trials—NLST in the U.S. and NELSON in Europe—showed roughly a 20 % reduction in lung‑cancer deaths when participants received annual LDCT. The scan uses a fraction of the radiation of a regular CT, yet it’s detailed enough to spot tiny nodules that would otherwise hide.
Emerging bronchoscopic navigation tools
Ever heard of a “bronchoscopic navigation tool”? Think of it as a high‑tech GPS for doctors, guiding a tiny camera through the airways to biopsy suspicious spots that a CT can’t reach. This innovative technology can retrieve tissue from early‑stage tumors that might otherwise be missed, giving pathologists a clear look at what’s really going on.
AI‑enhanced imaging & nanosensing (csPWS, breath analysis)
Artificial intelligence is turning ordinary scans into crystal‑clear detectives. One study used AI‑boosted chromatin nanosensing—called csPWS—to differentiate stage‑I lung cancer from healthy tissue with an area‑under‑the‑curve (AUC) of 0.92 % according to Nature. Another breakthrough? A breath‑analysis sensor that spots the molecule isoprene at just 2 parts per billion, distinguishing cancer patients from healthy volunteers in a small pilot.
Comparison Table – Traditional LDCT vs. AI‑optical nanosensing vs. Breath Test
| Feature | LDCT | AI‑optical nanosensing | Breath‑isoprene sensor |
|---|---|---|---|
| Radiation | Low | None | None |
| Sensitivity (stage I) | ~85 % | 92 % (AUC) | ~90 % (pilot) |
| Cost / Access | Moderate | Research‑grade | Potentially low |
| Best for | General high‑risk | Clinical trials / research | Non‑smoker monitoring |
Curious about the broader health perks of screening? Take a look at the lung cancer screening page for a rundown of cancer screening benefits.
Getting Screened Right
Eligibility checklist (USPSTF criteria)
Here’s the quick “yes‑or‑no” list you can run through with your doctor:
- Age 55‑80?
- At least 20 pack‑years of smoking?
- Current smoker or quit within the past 15 years?
If you tick all three boxes, you’re a prime candidate for annual LDCT. Once you pass 80 or haven’t smoked in more than 15 years, routine screening isn’t usually recommended—though your doctor may still keep an eye on you if other risk factors exist.
How to talk to your doctor
It can feel intimidating to bring up “screening” at a check‑up, but a simple script helps: “I read about the low‑dose CT screening for lung cancer. Based on my history, do you think I should be screened?” Doctors love engaged patients, and this opens the door for a clear risk‑assessment conversation.
What to expect during the scan
The LDCT appointment is quick—usually under 15 minutes. You’ll lie on a table, and the machine will glide around you while you hold your breath for a few seconds. The radiation dose is about 0.1 Sv, roughly the same as 10 days of natural background radiation. After the scan, a radiologist reviews the images and your doctor discusses any follow‑up steps.
Need a deeper dive on the test itself? Our lung cancer test guide walks you through what the results look like and what the next steps might be.
Balancing Benefits & Harms
False positives & downstream procedures
Screening isn’t a flawless crystal ball. About 25 % of LDCT screens flag something that looks suspicious but isn’t cancer. That can lead to extra scans, biopsies, and a few anxious weeks. The good news? Most false positives are caught early, and the overall mortality benefit still outweighs the inconvenience.
Radiation exposure concerns
Radiation scares are real, but the dose from an annual LDCT is tiny. Over ten years, you’d accumulate roughly the same exposure as a few cross‑country flights. For most, the life‑saving potential far eclipses the tiny risk.
Over‑diagnosis & “watchful waiting” strategies
Sometimes a tiny nodule is benign and would never cause problems. In those cases, doctors may recommend active surveillance—periodic scans every 3‑6 months—to monitor growth before deciding on an invasive procedure.
Expert tip
Dr. Maya Patel, board‑certified thoracic surgeon at a leading academic center, says, “A patient‑centered discussion about the pros and cons of screening is essential. We weigh the statistical benefit against personal values and health status.”
Real‑World Success Stories
Case 1 – High‑risk smoker caught at stage I
John, 62, smoked a pack a day for 30 years. He started LDCT screening after his doctor suggested it during a routine visit. A tiny nodule was spotted, and a quick biopsy confirmed stage I adenocarcinoma. He underwent a minimally invasive surgery and is now cancer‑free two years later. “I never imagined a scan could save my life,” he says, smiling.
Case 2 – Non‑smoker detected with AI‑nanotech model
Maria, 58, never smoked but worked in a shipyard with heavy metal exposure. She enrolled in a research trial using AI‑enhanced csPWS. The test flagged abnormal chromatin patterns, prompting a CT that revealed a 7 mm nodule. Early resection led to a full recovery. “I felt like I was part of the future of medicine,” she recalls.
Case 3 – Breath‑sensor trial participant
David, 49, has a family history of lung cancer but no smoking history. He joined a pilot study using the new breath‑analysis device. The sensor recorded isoprene levels consistently below the cancer threshold, prompting a baseline CT that was clear. Ongoing monitoring now offers him peace of mind without repeated radiation.
Future Directions Ahead
Integration of AI into routine CT reads
Radiology departments are piloting AI algorithms that instantly highlight suspicious spots on LDCT scans, cutting reading time and improving consistency. FDA clearance for several AI‑CAD tools is already in place, and we can expect broader adoption in the next few years.
Portable breath‑analysis devices for home screening
Imagine blowing into a handheld gadget at home, and within minutes you know whether you need a follow‑up scan. Ongoing clinical trials are fine‑tuning sensitivity and specificity, aiming for a low‑cost, radiation‑free first‑line screen.
Personalized risk calculators (genomics + exposure)
Beyond pack‑years, next‑gen calculators will combine DNA‑based risk markers, environmental data, and lifestyle factors into a single score. This could expand eligibility to people who traditionally fell through the cracks—like never‑smokers with a genetic predisposition.
According to a 2023 review, integrating AI with risk calculators “has the potential to increase early detection rates by up to 30 %” according to the study.
Quick Reference Checklist
- Who should screen? Age 55‑80, ≥20 pack‑years, current smoker or quit ≤15 years.
- What test? Low‑dose CT (annual) – the most validated lung cancer screening method.
- When? Once a year, or as directed by your physician.
- Where? Accredited imaging centers, hospitals, or specialized radiology clinics.
- Why? Reduces lung‑cancer mortality by ≈ 20 % and catches disease when 5‑year survival exceeds 75 %.
For a concise guide on navigating a quit smoking screening program, check out our dedicated page.
Conclusion
Early lung cancer detection isn’t a buzzword—it’s a lifeline. Whether you’re a long‑time smoker, a former smoker, or someone with hidden risk factors, the tools are evolving faster than ever. From proven low‑dose CT scans to cutting‑edge AI and breath sensors, you have more options than you might think. Take the first step: talk to your doctor, assess your personal risk, and consider a screening schedule that fits your life. Knowledge is power, and in this case, it can literally add years to your story.
What questions do you have about screening? Have you or a loved one experienced early detection? Share your thoughts, and let’s keep the conversation going.





















Leave a Reply
You must be logged in to post a comment.