Hey there, friend. If you’ve ever Googled “gallbladder cancer vs cholangiocarcinoma” you probably felt a wave of confusion – two scary‑looking names, a lot of medical jargon, and the worry that you might mix them up. Let me give you a straight‑up, human‑to‑human rundown of what these cancers really are, why they matter, and what you can do if you or someone you love faces a diagnosis. I promise to keep it clear, compassionate, and, when possible, a little uplifting.
Anatomy Basics
What the biliary system is
The biliary system is simply the network that moves bile – the liver’s grease‑breaking juice – from where it’s made to the tiny intestine where it helps digest fats. Think of it as a set of plumbing pipes: the tiny intra‑hepatic ducts inside the liver join to form the right and left hepatic ducts, which become the common hepatic duct. The cystic duct links that to the gallbladder, and the whole thing then continues as the common bile duct into the duodenum.
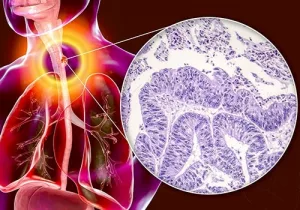
Gallbladder cancer in a nutshell
Gallbladder cancer (often abbreviated GBC) starts in the wall of the gallbladder itself, usually in the fundus or neck. Most of the time it’s an adenocarcinoma – a gland‑forming tumor – and it loves to be sneaky, staying hidden until it has already begun to spread.
Cholangiocarcinoma explained
Cholangiocarcinoma (CCA) is the fancy word for “bile‑duct cancer.” It can pop up anywhere along those ducts:
- Intra‑hepatic – inside the liver.
- Perihilar (Klatskin) – at the crossroads where the right and left hepatic ducts meet.
- Distal – farther down, closer to the pancreas and small intestine.
Because the ducts are long and winding, CCA can look like a lot of other problems, which is why we need to be diligent with imaging.
Symptoms Overview
What they share
Both cancers love to cause jaundice (that yellow glow in skin and eyes), unexplained weight loss, and a vague ache in the upper right abdomen. That overlap is why many patients hear “I have a bile‑duct problem” before the doctors can tell which one it really is.
Clues that point to gallbladder cancer
If pain comes on suddenly, you might feel a palpable lump in the right upper quadrant, or you could have frequent nausea and vomiting. Gallbladder neck tumors often cause a rapid rise in bilirubin and a short‑lived feverish chill – it’s a bit like a “sneaky thief” that quickly blocks the flow.
Clues that point to cholangiocarcinoma
Perihilar CCA often presents as painless, progressive jaundice. You may notice dark urine, pale (clay‑colored) stools, and relentless itching (pruritus) because bile salts are spilling into the skin. The pain, when it appears, tends to be deeper and more constant, as the tumor presses on surrounding tissue.
Real‑world snapshot
Imagine a 62‑year‑old man who showed up with painless jaundice that lingered for weeks. An MRI revealed a stricture right where the right and left hepatic ducts merge. A biopsy confirmed perihilar cholangiocarcinoma – a classic example that matches what Kapoor (2015) describes as “painless progressive surgical obstructive jaundice.”
Diagnostic Pathway
Finding the right diagnosis is a bit like detective work. You start with the easy clues and move to the high‑resolution evidence as the case unfolds.
| Modality | Best for Gallbladder Cancer | Best for Cholangiocarcinoma | Key Insight |
|---|---|---|---|
| Ultrasound | Detects gallbladder wall thickening, stones, and a mass | Shows biliary dilation, especially upstream of a blockage | First‑line, quick, non‑invasive |
| CT / MRI | Maps tumor size, local invasion, and regional nodes | Clarifies intra‑ vs extra‑hepatic location, vascular involvement | Cross‑sectional detail |
| MRCP / ERCP | Helps visualize cystic duct involvement | Excellent for delineating hilar lesions and planning surgery | Non‑invasive (MRCP) or therapeutic (ERCP) |
| PET‑CT | Useful for spotting metastases in gallbladder neck cancer | Not routinely recommended for perihilar CCA | Detects distant spread |
| Biopsy / FNA | Endoscopic‑ultrasound or percutaneous core | Cholangioscopy‑guided tissue sampling | Pathologic confirmation |
Staging at a glance
Both cancers use the AJCC 8th‑edition staging system, which grades tumor depth (T), nodal involvement (N), and distant spread (M). The numbers help doctors decide if surgery is an option or if we’re looking at systemic therapy.
Trusted data point
According to the National Cancer Institute’s PDQ summary (2025), only about 30% of gallbladder cancers are caught at a stage where a simple cholecystectomy can cure the patient.
Biology & Prognosis
How aggressive are they?
Gallbladder neck cancer is notoriously aggressive. Kapoor’s editorial (2015) highlights that “long‑term survivors are rare even after major resection.” In contrast, perihilar cholangiocarcinoma often behaves a bit less ruthlessly, making surgical resection a justified gamble in many cases.
Survival numbers you should know
- U.S. estimates for 2025: ~12,610 new biliary cancers and ~4,400 deaths.
- 5‑year survival for localized gallbladder cancer hovers around 20‑30%.
- Intra‑hepatic CCA: roughly 30% 5‑year survival when resected; perihilar CCA can reach 40% with successful surgery.
These stats sound grim, but remember – they’re averages. Individual outcomes can be better when the disease is caught early and treated at a high‑volume center.
Visual aid (imagine a chart)
If you picture two side‑by‑side Kaplan‑Meier curves, you’ll see the gallbladder curve dropping faster than the cholangiocarcinoma curve, reflecting that aggressive biology.
Treatment Options
Curative intent surgery
When the tumor is still localized, surgery offers the best hope:
- Gallbladder cancer (T1a): Simple laparoscopic cholecystectomy usually suffices.
- Gallbladder cancer (T2‑T3): Extended resections that remove a wedge of liver and regional lymph nodes.
- Perihilar cholangiocarcinoma: A liver‑first (Klatskin) resection, often a hemi‑hepatectomy with bile‑duct reconstruction.
- Distal cholangiocarcinoma: The classic Whipple (pancreatoduodenectomy) procedure.
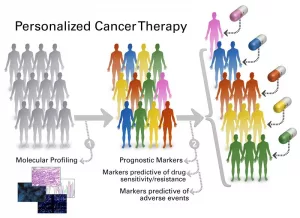
Neoadjuvant and adjuvant therapy
Most of us think chemotherapy is a “last resort,” but modern protocols weave it in both before and after surgery:
- CCA: Gemcitabine plus cisplatin is the standard combo for advanced or borderline‑resectable disease (per NCI PDQ).
- GBC: After an R0 resection, capecitabine for six months has shown a modest survival bump.
Palliative care pathways
If curative surgery isn’t possible, the goal shifts to quality of life:
- Endoscopic biliary stenting to relieve jaundice.
- Radiofrequency ablation or photodynamic therapy for local control.
- Clinical trials – always worth asking your oncologist about.
A patient story for perspective
John, a 58‑year‑old teacher, was diagnosed with perihilar cholangiocarcinoma after months of unexplained itching and yellow skin. He started neoadjuvant gemcitabine‑cisplatin, which shrank the tumor enough for a successful hemi‑hepatectomy. Six months later, his follow‑up scans are clean, and he’s back to grading papers – a reminder that aggressive treatment can pay off when the disease is caught early enough.
Risk & Prevention
Key risk factors
| Factor | Higher risk for Gallbladder Cancer | Higher risk for Cholangiocarcinoma |
|---|---|---|
| Gallstones / chronic cholecystitis | ✔️ | — |
| Primary sclerosing cholangitis (PSC) | — | ✔️ |
| Liver fluke infection (Clonorchis, Opisthorchis) | — | ✔️ |
| Obesity / diabetes | ✔️ | ✔️ |
| Familial adenomatous polyposis, Lynch syndrome | ✔️ | ✔️ |
What you can do today
While there’s no universal screening program for biliary cancers, people with known risk factors benefit from regular imaging:
- Annual abdominal ultrasound for anyone with gallstones over age 60.
- MRCP every 1–2 years for patients with PSC or a known history of liver fluke infection.
- Maintain a healthy weight, manage diabetes, and avoid exposure to industrial chemicals where possible.
Expert source
StatPearls notes that biliary tract cancers make up less than 2% of all malignancies but carry a “high mortality rate” (StatPearls, 2023).
Take‑away Checklist
Symptoms to flag
- Jaundice (yellow skin/eyes)
- Persistent upper‑right abdominal pain
- Dark urine, pale stools, itching
- Unexplained weight loss or fever
Diagnostic steps to expect
- Abdominal ultrasound
- Cross‑sectional imaging (CT or MRI)
- MRCP/ERCP for detailed duct mapping
- Biopsy for definitive pathology
Treatment decision tree
- Early, resectable disease → Surgery ± adjuvant chemo
- Borderline / locally advanced → Neoadjuvant chemo → Re‑assessment → Surgery if possible
- Unresectable → Palliative stenting, systemic therapy, clinical trial enrollment
Follow‑up schedule
Most specialists recommend imaging and blood work every three months for the first year, then every six months for the next two years, and annually thereafter.
Wrapping It Up
Understanding the differences between gallbladder cancer and cholangiocarcinoma isn’t just academic – it changes the conversations you have with your doctors, the tests you undergo, and ultimately the chances of a cure or meaningful control. Both cancers belong to the broader family of biliary system cancers, yet their biology, symptoms, and treatment pathways diverge enough that mixing them up can be dangerous.
Remember, knowledge is power, but empathy is the glue that keeps us moving forward together. If any of this resonated with you, share your thoughts in the comments, ask questions, or tell a friend who might need this info. And if you or a loved one are navigating a diagnosis, reach out to a high‑volume hepatobiliary center – the expertise there can make a world of difference.
We’re all in this together. Stay curious, stay proactive, and never underestimate the strength of a supportive community.





















Leave a Reply
You must be logged in to post a comment.