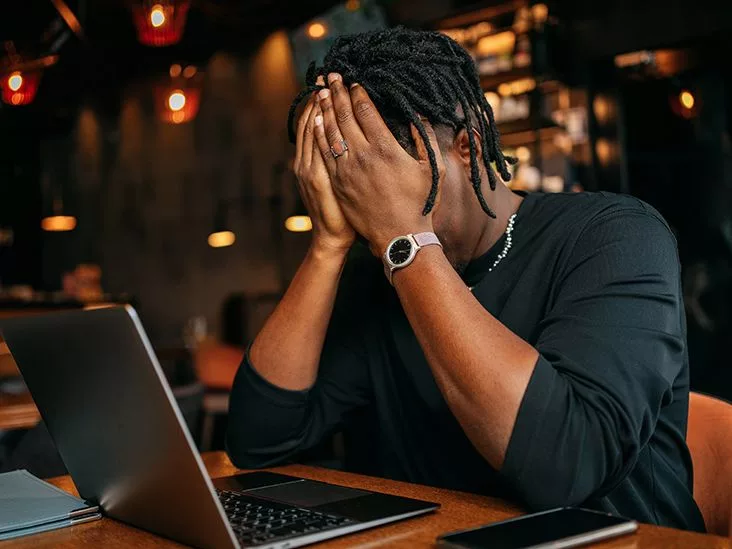
Feeling like your nervous system is stuck on “high alert” even when there’s nothing dangerous around? You’re not crazy, you’re probably dealing with hyperstimulation anxiety. In the next few minutes we’ll break down what that means, why it happens, how to spot it, and—most importantly—what you can actually do today to calm the overload.
What Is Hyperstimulation Anxiety?
In plain language, hyperstimulation anxiety is a state where the body’s stress‑response system stays turned on far longer than it should. Imagine a fire alarm that keeps ringing after the fire is gone—your brain and body keep reacting as if the danger is still present.
It isn’t a formal diagnosis in the DSM‑5, but clinicians and researchers increasingly use the term to describe a pattern of chronic “fight‑flight‑freeze” activation that fuels intense anxiety symptoms. The science behind it is pretty solid: when the hypothalamus, pituitary gland, and adrenal glands keep sending cortisol and adrenaline into the bloodstream, the nervous system never gets the chance to hit the reset button.
According to BetterHelp, this continuous hormonal surge can “push the body beyond its natural equilibrium,” making everyday stress feel like a life‑or‑death situation.
How the Stress Response Gets Stuck
Under normal circumstances, a perceived threat triggers a cascade:
- Hypothalamus shouts “danger!”
- Pituitary gland releases ACTH.
- Adrenal glands dump cortisol and adrenaline.
The surge prepares you to fight, flee, or freeze. Once the threat passes, the system winds down. In hyperstimulation, the “threat” never fully disappears—digital notifications, bright screens, crowded places, even endless to‑do lists can keep the alarm blaring.
Why It’s Not Just “Regular” Anxiety
Regular anxiety usually spikes in response to a specific worry and then eases. Hyperstimulation anxiety is more like a low‑level background static that never fully fades. The difference shows up in intensity, duration, and the ways it infiltrates daily life.
| Aspect | Regular Anxiety | Hyperstimulation Anxiety |
|---|---|---|
| Trigger | Specific event or thought | Continuous low‑level stimuli (phone, lights, noise) |
| Duration | Minutes‑hours | Hours‑days, often all day |
| Physiological load | Occasional spikes | Constant cortisol elevation |
Spotting the Symptoms
If you’re unsure whether you’re dealing with hyperstimulation, run through this quick checklist. Do any of these sound familiar?
- Heart racing or pounding even when you’re sitting still.
- Constant “on‑edge” feeling—like a kettle that never fully cools.
- Frequent headaches, migraines, or neck tension.
- Sleep that feels broken—waking up multiple times or tossing‑turning for hours.
- Upset stomach, nausea, or “butterflies” that won’t go away.
- Difficulty concentrating, feeling mentally foggy.
- Compulsive checking of phones, emails, or news feeds because you can’t tolerate the silence.
These are the same anxiety symptoms many people report, but notice how they linger well beyond the original stressor. That lingering is the hallmark of hyperstimulation.
When to Seek Professional Help
If any of the following are happening, it’s time to talk to a mental‑health professional:
- Symptoms interfere with work, school, or relationships.
- You experience panic attacks or panic‑like sensations.
- Thoughts of self‑harm or hopelessness appear.
- Physical health issues (e.g., high blood pressure) arise from chronic stress.
Remember, asking for help is a sign of strength, not weakness.
Typical Hyperstimulation Triggers
What’s turning your nervous system into a perpetual alarm? Below are the most common culprits, plus a little anecdote to illustrate each.
Digital Overload
Ever notice how a single buzz from your phone can make your heart leap? Constant notifications, endless scrolling, and “doom‑scrolling” news cycles keep the brain in a state of readiness. My friend Maya tried a “no‑phone hour” before bed and literally felt her pulse settle within 15 minutes.
Environmental Stressors
Loud music, flickering lights, bustling crowds—these are sensory inputs that can overwhelm anyone, especially those with heightened sensitivity. Think of a crowded subway during rush hour: the noise, the close quarters, the flashing ads—your nervous system can interpret that as a threat.
Physiological Contributors
Sleep debt, too much caffeine, or hormonal swings (like during menopause) all lower the threshold for overstimulation. A study published in NCBI found that chronic caffeine intake can amplify cortisol responses, feeding the hyperstimulation cycle.
Psychological Factors
Perfectionism, high‑pressure jobs, or chronic worry act like a mental “fuel injector,” constantly feeding the stress engine. When you’re constantly telling yourself, “I have to be perfect,” the body refuses to relax.
Underlying Conditions
People with autism spectrum disorder, sensory processing disorder, or a highly sensitive personality (HSP) often have a lower tolerance for everyday stimuli, making hyperstimulation more likely.
Effect on Existing Anxiety
If you already battle generalized anxiety or panic, hyperstimulation can turn that into a full‑blown storm. Here’s why:
The Feedback Loop
Persistent cortisol keeps the amygdala—the brain’s fear center—hyper‑reactive. That means even minor stressors feel monumental, and the “fight‑flight‑freeze” response is triggered more easily. It’s a vicious cycle: anxiety fuels hyperstimulation, which in turn deepens anxiety.
Why Treatment May Feel Stuck
Therapies like CBT work by teaching you new thought patterns, but if your nervous system never gets a break, the new patterns struggle to take root. Medications can also be less effective when the body is constantly flooded with stress hormones.
Research Snapshot
According to a 2022 study, chronic cortisol elevation is linked to reduced efficacy of standard anxiety medications, underscoring the importance of addressing hyperstimulation directly.
Managing the Overload
Good news: there are concrete steps you can take right now to dial the volume down.
Digital Hygiene
- Set specific “phone‑free” windows (e.g., 7‑9 p.m.).
- Disable non‑essential notifications—your brain will thank you.
- Use grayscale or “night mode” to reduce visual stimulation.
Sleep Optimisation
A consistent bedtime routine signals to your nervous system that it’s safe to shut down. Try a warm shower, a short meditation, and keep the bedroom cool and dark.
Nutrition & Caffeine Management
A balanced diet stabilises blood sugar, which in turn steadies mood. Cutting back on coffee or energy drinks can lower that baseline cortisol surge.
Physical Activity
Even a brisk 20‑minute walk releases endorphins and helps metabolise excess adrenaline. Yoga or gentle stretching is especially useful because it combines movement with breath awareness.
Environment Design
Soft lighting, calming colours, and a tidy workspace reduce sensory overload. If you can’t control a noisy environment, earplugs or a white‑noise app can be lifesavers.
Talk Therapy (CBT, ACT)
Therapists can help you reframe the “alarm” narrative, teaching you skills to recognise when the stress response is falsely activated. Cognitive‑behavioral approaches target the thought patterns that keep the system on high alert.
Medication Options
Selective serotonin reuptake inhibitors (SSRIs) or serotonin‑norepinephrine reuptake inhibitors (SNRIs) can lower overall anxiety levels, making it easier for the body to return to baseline after a stress spike. Always discuss options with a qualified prescriber.
Mind‑Body Techniques
Breathing exercises, progressive muscle relaxation, and grounding practices can quickly bring the nervous system back into the “rest‑and‑digest” mode.
Quick‑Start Reset Routine (Featured‑Snippet Friendly)
- Pause & Breathe: Try the 4‑7‑8 method—inhale 4 seconds, hold 7, exhale 8.
- Screen‑Off: Put your phone on “Do Not Disturb” for at least 10 minutes.
- Ground: Name 5 things you see, 4 you feel, 3 you hear, 2 you smell, 1 you taste.
- Move: Stretch arms overhead, roll shoulders, or walk around the room for two minutes.
- Hydrate: Sip a glass of water—hydration supports cortisol regulation.
Do this whenever you notice that jittery feeling creeping in, and you’ll often feel the “overdrive” light dim.
Everyday Success Stories
Stories make the science feel real. Here are three short snapshots of people who took small steps and saw big changes.
Mike’s Tech‑Detox
Mike, a software developer, found his heart racing during coding sprints. He set a strict “no phone after 8 p.m.” rule. After two weeks, his resting heart rate dropped by 10 bpm and he reported feeling “much calmer” during work.
Lena’s Sleep Overhaul
Lena struggled with insomnia and constant daytime fatigue. She introduced a wind‑down routine: dim lights, a warm bath, and a short meditation. Within a month, she slept an average of 7 hours per night, and the “mind‑racing” anxiety symptoms faded dramatically.
Sam’s CBT Journey
Sam sought therapy after realizing he couldn’t relax even on vacation. Over eight CBT sessions, he learned to identify the “alarm” thoughts and replace them with grounding statements. He now reports a 40 % reduction in hyper‑alert moments, according to his therapist’s notes.
Final Thoughts & Steps Forward
Hyperstimulation anxiety can feel like living inside a perpetual storm, but it’s not a life sentence. By recognizing the triggers, understanding the science, and implementing practical lifestyle tweaks, you give your nervous system permission to hit the “off” switch.
Start with one tiny habit—maybe that 10‑minute phone‑free window or the 4‑7‑8 breathing exercise. Notice how your body responds, and celebrate the small wins. If the overload persists, reach out to a mental‑health professional; they can tailor a treatment plan that combines therapy, medication, and coping strategies just for you.
What’s your biggest hyperstimulation trigger? Have you tried any of the reset techniques? Share your experiences in the comments or reach out to a trusted therapist. You’re not alone in this, and together we can turn down the volume on that internal alarm.






















Leave a Reply
You must be logged in to post a comment.