Imagine sitting down with a friend over coffee and saying, “I just heard that we can catch cancer without a needle in the arm.” Your friend would probably raise an eyebrow, maybe a hint of excitement, and then ask, “Seriously? How?” That’s the exact moment this article steps in. In the next few minutes we’ll unpack why non‑invasive early diagnosis is more than a buzzword, how saliva and a drop of blood are becoming superhero detectives, and what you can realistically expect when you or a loved one thinks about getting tested. Ready? Let’s dive in.
Why It Matters
The survival gap
Early detection isn’t just a nice‑to‑have; it’s a life‑saver. Data from the U.S. SEER program shows that five‑year survival for stage I cancers can exceed 80 %, while the same metric for stage IV cancers often drops below 10 %. The difference is stark, and it largely comes down to how early we find the disease.
Cost and emotional toll of invasive biopsies
Traditional biopsies can feel like an ordeal: a needle, a waiting period, anxiety about complications, and often a costly hospital visit. For many, the physical discomfort mirrors the emotional weight of waiting for results. Non‑invasive tests aim to cut both the pain and the paperwork, giving you more time for the things that actually matter.
Science backing the shift
According to a 2022 Nature Communications study, a cfDNA‑methylation assay called CancerRadar achieved 81 % sensitivity for stage I/II cancers while maintaining 97.9 % specificity. Those numbers are no longer sci‑fi; they’re the new baseline for what non‑invasive tests can deliver.
Saliva Markers Explained
What are saliva disease markers?
Saliva isn’t just a watery mess; it’s a molecular library. From micro‑RNAs to volatile organic compounds (VOCs), your mouth holds clues about what’s happening deep inside your body. Scientists call these clues saliva disease markers, and they’re becoming a hot topic in research labs worldwide.
Key saliva cancer‑risk biomarkers
Several molecules have shown promise:
- miR‑21 – often elevated in oral and lung cancers.
- DNA methylation patterns – especially in genes like p16 and RASSF1A.
- VOCs – a unique scent signature that can indicate lung cancer, as demonstrated by a 2024 AI‑driven optical sensor study (see the Light‑AI story).
These markers can be measured with a simple spit‑into‑a‑tube, no syringes required.
Real‑world case study
A Korean research team recently used a paper‑based sensor to detect lung‑cancer metabolites in saliva. Their AI model could not only tell “cancer or not” but also assign a stage with over 90 % accuracy. It felt a bit like giving the test a “super‑sniff” – just like a dog, only less cute and more scientific.
Want to dig deeper?
Check out saliva cancer risk for a friendly guide on what those markers mean for you.
Collecting saliva the right way
Here’s a quick checklist to ensure you get a reliable sample:
- Do not eat, drink, or chew gum for at least 30 minutes.
- Rinse your mouth with plain water – no mouthwash.
- Spit into a sterile tube until you reach the indicated line (usually 2 ml).
- Seal the tube, label it, and keep it cool (refrigerator) if you can’t ship it within an hour.
Liquid Biopsy Basics
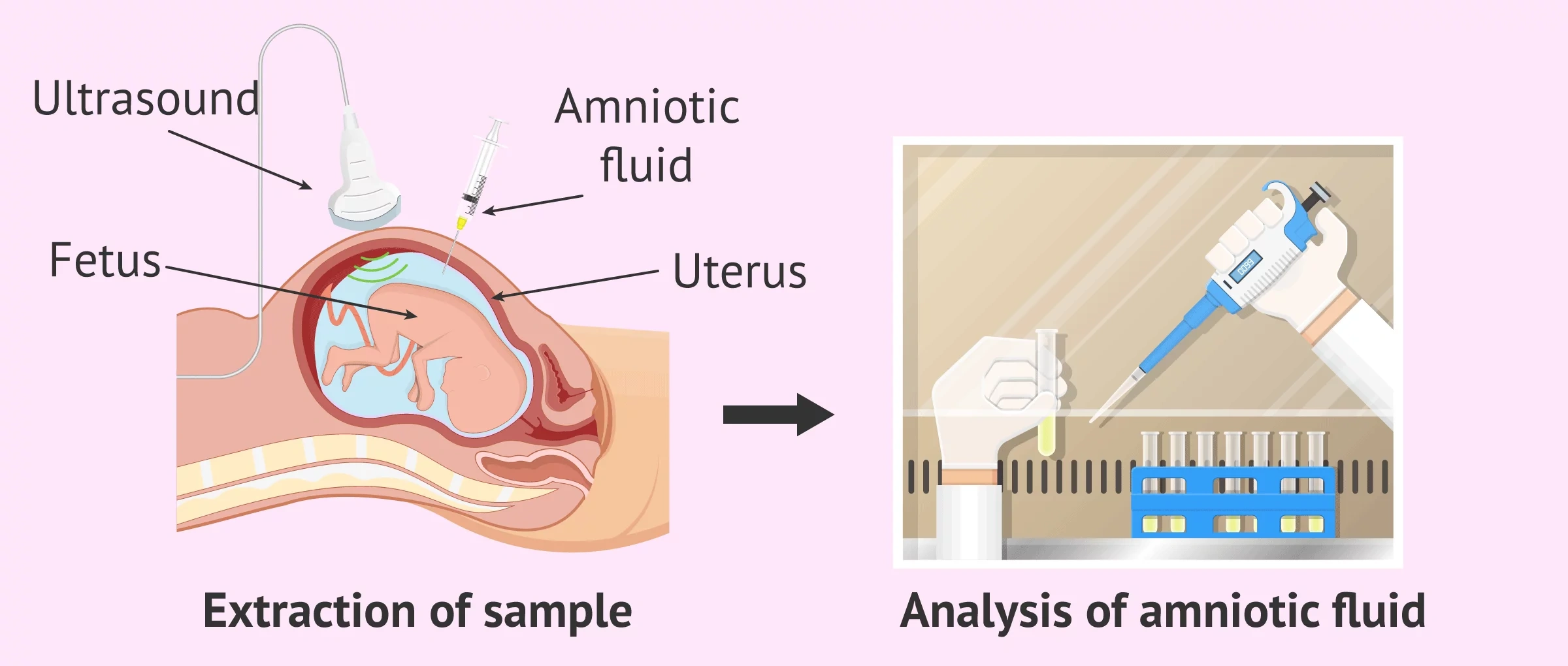
cfDNA methylation profiling
Circulating cell‑free DNA (cfDNA) is shed by cells everywhere, including tumors. By looking at methylation patterns – tiny chemical tags on DNA – researchers can spot cancer signals hidden among millions of normal DNA fragments. Platforms like CancerRadar and Insighta’s FRAGMA use this approach to locate not just the presence of cancer but also its tissue of origin.
Performance numbers you can trust
When researchers applied cfDNA methylation to 408 patients with colon, liver, lung, and stomach cancers, they reported 85.9 % overall sensitivity and an 84.4 % accuracy for locating the tissue of origin in early‑stage disease. CancerRadar’s data backs those figures.
FRAGMA’s AUC scores
Insighta’s FRAGMA liquid‑biopsy platform posted AUC (area under the curve) values of 0.98 for liver cancer, 1.00 for colorectal cancer, and 0.90 for lung cancer. In plain English: the test is extremely good at distinguishing cancer patients from healthy controls.
Comparison: Saliva vs. Blood
| Aspect | Saliva Test | Blood cfDNA Test |
|---|---|---|
| Sample type | Spit (non‑invasive) | Finger‑prick or venipuncture |
| Key biomarkers | miRNAs, DNA methylation, VOCs | cfDNA methylation, fragmentomics |
| Turn‑around time | Hours to 1 day | 1–2 days (lab processing) |
| Cost (US) | $100–$200 | $300–$600 |
| Clinical readiness | Early‑stage trials, FDA‑review pending | Commercially available (e.g., Galleri, CancerRadar) |
Exosome AI Breakthrough
How Exosome‑SERS‑AI works
Exosomes are tiny vesicles released by cells, carrying proteins, DNA, and RNA. By shining a laser on them and measuring the resulting Raman scattered light (SERS), scientists generate a spectral fingerprint. Feed those fingerprints to an AI model, and you get a diagnostic output that tells not only “cancer?” but also “which organ?”
Stunning accuracy
A 2023 study showed an AUC of 0.970 for detecting any of six early‑stage cancers, and an average AUC of 0.945 for pinpointing the organ of origin. That’s like having a single test that can say, “Yes, there’s a tumor, and it’s most likely in the colon.”
Practical outlook
Right now, the technology lives in research labs, but commercial kits are on the horizon. The biggest hurdle isn’t the physics—it’s regulatory approval and scaling the AI model across diverse populations.
Explore the science
Read the full Nature paper for a deep dive into the method.
Precision Medicine Link
From test to treatment
When a non‑invasive test flags a potential cancer, the next step isn’t panic; it’s targeted follow‑up. Imagine your doctor receives a detailed risk score that highlights specific pathways—say, an over‑active KRAS mutation in a colorectal signal. That score can guide the choice of a targeted therapy, sparing you from generic chemo that may not work.
Research hubs leading the way
Key players include:
- Grail’s multi‑cancer early detection (MCED) platform.
- Insighta’s FRAGMA liquid biopsy.
- University‑industry consortia developing AI‑driven exosome analysis.
All of them aim to plug early‑diagnosis data straight into precision‑medicine pipelines.
Read more about the field
Our precision medicine research page breaks down how these data streams become actionable treatment plans.
Balancing Benefits Risks
False positives and anxiety
No test is perfect. A false‑positive result can send you down a cascade of imaging, biopsies, and sleepless nights. That’s why specificity—how well a test avoids false alarms—is as crucial as sensitivity. Most FDA‑cleared liquid‑biopsy tests report > 95 % specificity, meaning less than 5 % of healthy people will be flagged.
Regulatory and ethical angles
Regulators like the FDA demand rigorous validation, especially when AI decides medical outcomes. Data privacy is another hot topic; you’re essentially handing over a genetic snapshot of yourself. Trustworthy companies will encrypt data, store it securely, and give you control over who can see it.
Patient‑centred checklist
Before you book a non‑invasive test, ask yourself:
- Is the test FDA‑cleared or CE‑marked?
- What is the reported sensitivity for the cancer type I’m most at risk for?
- How will a positive result be confirmed?
- Does my insurance cover the test, or will I pay out‑of‑pocket?
Choosing the Right Test
Factors to weigh
Age, family history, personal risk factors (smoking, diet), and the specific cancers you’re most concerned about will shape the best choice. For example, if lung cancer looms large in your family, a saliva‑based VOC test might be a perfect first step. If you have a broader cancer‑screening desire, a blood‑based cfDNA panel could cover more ground.
Decision‑tree snapshot
Picture a simple flowchart:
- Do you prefer a painless at‑home test? –> Look at saliva disease markers options.
- Do you need multi‑cancer coverage? –> Consider FDA‑cleared blood panels.
- Are you comfortable with AI‑driven results? –> Explore Exosome‑SERS‑AI studies.
Final thoughts before you decide
Ask your doctor to walk you through the pros and cons of each method, and remember that early detection is a partnership—you, your clinician, and the lab technology all play a part.
Conclusion
Non‑invasive early diagnosis is no longer a futuristic promise; it’s a practical reality that blends saliva science, liquid‑biopsy magic, and AI brilliance. By understanding the strengths and limits of each test, you can make informed choices that keep you one step ahead of disease. So, next time you hear “painless cancer testing,” don’t dismiss it as hype—dig in, ask questions, and consider whether a simple spit or a quick blood draw could be the key to a healthier future.
If you’re curious about specific markers or want to explore how these tests fit into a personalized treatment plan, feel free to explore our saliva molecular biomarkers page or reach out to a trusted healthcare professional. Early detection is a conversation—let’s keep it going.




















Leave a Reply
You must be logged in to post a comment.