Imagine you’ve just heard the term “BCG therapy” tossed around at a doctor’s office. Your mind probably races with questions: Is it a vaccine? A chemotherapy? Will it work for me? In the next few minutes I’ll walk you through exactly what BCG therapy is, how it works, who benefits, and what you can expect along the way. No jargon‑filled lecture—just a friendly chat that gets straight to the point.
What Is BCG Therapy?
What does “BCG” stand for?
BCG is short for Bacillus Calmette‑Guerin, a weakened strain of the bacterium that originally protects against tuberculosis. Doctors discovered that, when placed directly into the bladder, this “tuberculosis vaccine cancer”‑style agent can rally your immune system to hunt down cancer cells.
Why is it called an immunotherapy?
It’s a biologic response modifier. Instead of attacking the tumor directly, BCG acts like a fire alarm, waking up immune cells that then seek and destroy cancer cells lining the bladder. This local immune boost is why many urologists refer to it as the gold‑standard bladder cancer immunotherapy.
Is BCG a vaccine or a cancer drug?
Both, in a way. It started life as a TB vaccine, but today it’s repurposed as a cancer treatment. Think of it as a “double‑agent” that borrows the safety profile of a vaccine while delivering a powerful anti‑cancer punch.
How does BCG differ from chemotherapy?
| Aspect | BCG Therapy | Chemotherapy (intravesical) |
|---|---|---|
| Mechanism | Stimulates immune response | Direct cytotoxic kill |
| Typical Use | High‑grade NMIBC | Low‑to‑intermediate grade |
| Side‑Effect Profile | Flu‑like symptoms, bladder irritation | Systemic toxicity, chemical cystitis |
| Duration of Treatment | Induction + maintenance (up to 3 years) | Usually 6‑8 weekly instillations |
Key takeaway
If you’re facing early‑stage bladder cancer, BCG offers a targeted, immune‑driven approach that many specialists trust over traditional chemo for high‑grade disease.
How BCG Works Inside
What is the biological mechanism?
When the BCG solution lands in your bladder, it’s taken up by the bladder’s lining cells. This triggers a cascade of signals—TNF‑α, IFN‑γ, and other cytokines—that summon macrophages, dendritic cells, and T‑cells. Those soldiers then patrol the bladder, seeking out and destroying any rogue cancer cells.
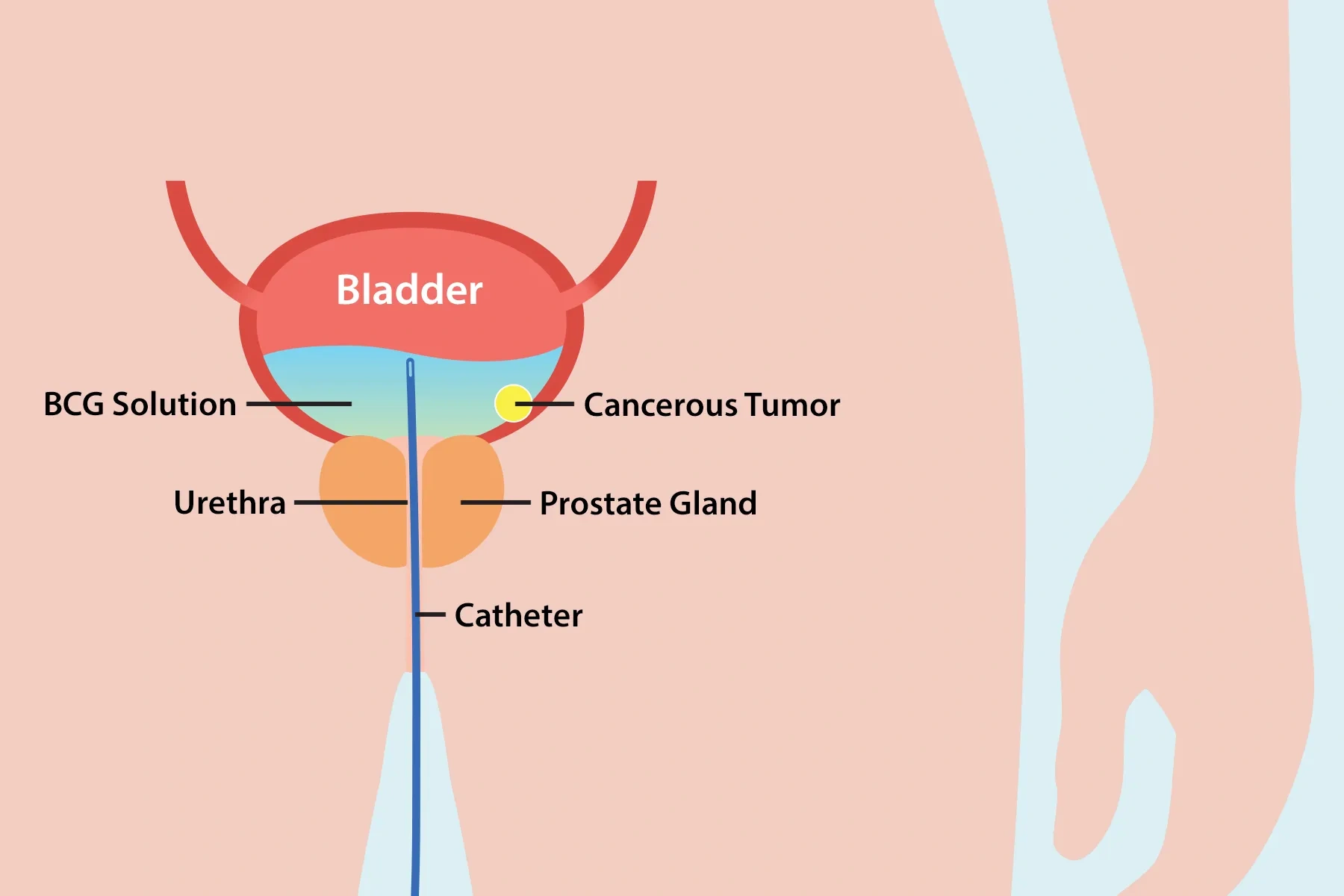
What does “intravesical” mean?
“Intravesical” simply means “inside the bladder.” A thin catheter (think of a tiny garden hose) delivers the liquid directly into the bladder, ensuring the medicine coats every nook and cranny.
Why use a live‑attenuated bacterium?
Live‑attenuated bacteria are great at keeping the immune system’s attention. They’re not strong enough to cause disease, but they’re alive enough to provoke a robust, lasting immune response—exactly what we need to keep bladder tumors at bay.
Evidence of efficacy
According to a 2023 systematic review, BCG reduced recurrence rates by more than 30 % compared with TURBT alone, and patients who completed a full maintenance schedule enjoyed up to a 70 % five‑year disease‑free survival rate. a 2023 study confirms these numbers across multiple international centers.
Bottom line
BCG turns your bladder into an immunologically “hot” environment—exactly the kind of setting that helps the body keep cancer under control.
Who Should Get BCG?
Which bladder‑cancer stages qualify?
BCG is primarily used for carcinoma in situ (CIS) and non‑muscle‑invasive bladder cancer (NMIBC) stages Ta and T1, especially when the tumors are high‑grade (aggressive). In plain language: if the cancer is still on the surface of the bladder and hasn’t invaded the muscle wall, BCG is often the first line of defense.
Can BCG be used after TURBT?
Yes! The standard pathway is transurethral resection of bladder tumor (TURBT) followed by BCG induction. The surgery removes visible tumors, and BCG cleans up any microscopic cells that might be left behind.
Contra‑indications & red flags
- Severe immunosuppression (high‑dose steroids, HIV, organ transplant)
- Active urinary tract infection or hematuria
- History of severe BCG reaction (sepsis)
- Recent bladder or prostate surgery (< 2 weeks)
- Pregnancy or breastfeeding
Special populations
Older adults often tolerate BCG well, but they may need closer monitoring for systemic flu‑like symptoms. Pediatric cases are rare but have been reported in specialist centers.
For a broader view of options, see our guide to NMIBC treatment.
BCG Treatment Schedule
What is the standard induction regimen?
Induction usually means six weekly installations. Each session involves a catheter placement, a brief dwell time (1–2 hours), and then you go home. Think of it as a “boot‑camp” for your immune system.
How does maintenance therapy work?
If the cancer responds, doctors often recommend maintenance: three weekly installations every six months (at 3, 6, and 12‑month marks), potentially extending up to three years. This “maintenance” phase is key to keeping the cancer from creeping back.
What’s the role of cystoscopy between phases?
After induction, a cystoscopy (a tiny camera exam) checks whether the bladder looks clear. If it does, you move into maintenance; if not, your doctor may adjust the plan.
Visual timeline
Imagine a calendar: weeks 1‑6 = induction, then a 2‑week break for cystoscopy, weeks 8‑10 = “post‑induction boost,” followed by maintenance cycles at 3‑month intervals. Keeping this schedule on a wall or phone reminder can make the process feel manageable.
Key point
Sticking to the full schedule dramatically improves long‑term outcomes—think of it as planting a garden and watering regularly, rather than a one‑time sprinkle.
Preparing for BCG
Pre‑procedure checklist
- Stop diuretics and certain antibiotics 4 hours before (your nurse will confirm).
- Empty your bladder just before the appointment.
- Avoid caffeine and limit fluid intake for the 4 hours prior.
- Bring a list of all medications—some may need a temporary pause.
What to bring to the clinic?
A small bag with your ID, medication list, a water bottle (for after you’re done), and perhaps a favorite book or playlist to pass the time while the BCG sits in your bladder.
Do I need a driver?
If you live far from the treatment center (say a 2‑hour drive), arrange for a friend or family member to take you home. Some patients even keep a “BCG travel kit” with a blanket, snacks, and a phone charger.
Home‑care after the session
- Hold the BCG for 1‑2 hours—don’t force yourself to urinate.
- Drink plenty of fluids afterward to flush the bladder.
- Follow the bleach‑toilet protocol for the next 6 hours (2 cups of undiluted bleach, lid closed, wait 15 minutes, then flush).
- Avoid public restrooms if possible during that window.
Looking for ways to boost the immune response? Check out our article on enhanced immunotherapy for complementary strategies.
What Happens During Procedure
Step‑by‑step walk‑through
- Urine sample: Checks for infection or blood.
- Catheter placement: A thin tube slides through the urethra into the bladder.
- Drainage: Any residual urine is removed.
- Instillation: About half a cup of BCG solution is pumped into the bladder.
- Catheter removal: Usually taken out right away.
- Dwell time: You lie comfortably while the solution sits for 1‑2 hours.
How long is the appointment?
Typically about two hours total—15 minutes for prep, 30‑45 minutes for the actual instillation, and the remaining time for the dwell period.
Pain control & anesthesia
Most centers use a local anesthetic lidocaine gel to numb the urethra. If you’re anxious, ask about a mild oral sedative; it won’t affect the BCG itself.
What if I can’t hold it?
Some patients use an incontinence pad or a “Depends” brief‑wear product for the drive home. It’s a practical solution and completely normal—just remember to wash clothing separately afterward.
Safety tip
Avoid driving or operating heavy machinery for at least four hours after each treatment, as the flu‑like feelings can linger.
Side Effects & Management
Common local reactions
Most people feel a mild burning sensation, urgency, and more frequent trips to the bathroom. Blood in the urine (hematuria) can appear but usually clears within a few days.
Systemic symptoms
Low‑grade fever, chills, fatigue, and muscle aches are typical “flu‑like” side effects. They’re signs your immune system is doing its job. If fever climbs above 38.5 °C or lasts longer than 48 hours, call your care team.
Rare but serious complications
In less than 1 % of patients, BCG can cause sepsis, bladder contracture, or allergic‑type reactions. Look out for severe abdominal pain, persistent high fever, or sudden swelling—these warrant immediate medical attention.
Self‑care measures
- Increase water intake (2‑3 liters/day) to flush the bladder.
- Take acetaminophen for fever or discomfort (avoid NSAIDs unless prescribed).
- Use a sitz bath or warm compress for bladder pain.
- Over‑the‑counter urinary pain relievers (e.g., Azo®) can help with burning.
When to seek urgent care
If you notice large clots, severe abdominal pain, or a fever that won’t break, get to a hospital straight away. Early intervention prevents complications.
Balanced view
The benefits of BCG—lower recurrence, potential cure—usually outweigh these manageable side effects. Knowing what to expect turns uncertainty into confidence.
Expert Insights & Real‑World Stories
Dr. Maria Alvarez, a urologist at a leading cancer center, says, “I recommend BCG for any high‑grade NMIBC because the long‑term data consistently show better disease‑free survival compared with intravesical chemo.” She adds, “The key is patient adherence to the maintenance schedule—skipping weeks can reduce the protective effect.”
Jonathan’s story (the quote you saw in the snippet) illustrates this perfectly: after a series of TURBT surgeries, he embarked on a 12‑month BCG regimen. “The first few weeks were rough—fever and a lot of bathroom trips—but I kept a journal, noted the side‑effects, and stayed in close contact with my nurse. By month 6, my cystoscopy was clear, and the maintenance cycles felt more like a routine than a battle.”
These anecdotes remind us that while BCG isn’t a magic bullet, it’s a powerful ally when paired with diligent follow‑up and a supportive care team.
Resources & Further Reading
For deeper dives, explore these trusted pages:
- Comprehensive guide to bladder cancer immunotherapy
- Details on the tuberculosis vaccine cancer connection
- Updates on enhanced immunotherapy options
- All you need to know about NMIBC treatment
Remember, choosing a treatment is a personal journey. Talk openly with your urologist, ask the questions that matter to you, and keep a notebook of symptoms and feelings. You deserve a clear roadmap, and BCG therapy can be a cornerstone of that plan.
Conclusion
BCG therapy transforms a simple bacteria into a targeted immune weapon for early‑stage bladder cancer. By understanding how it works, who it helps, and what the treatment journey looks like, you can approach the process with confidence rather than fear. Stick to the induction and maintenance schedule, manage side effects with practical self‑care, and lean on your healthcare team for guidance. If you or a loved one are navigating NMIBC, consider asking your doctor whether BCG therapy fits your story—you might just find the ally you need to keep cancer at bay.






















Leave a Reply
You must be logged in to post a comment.