Calciphylaxis is a kidney-related complication characterized by calcium depositing inside the small blood vessels of fat and skin. It produces intensely painful skin lesions and frequently leads to severe infections. Clinical studies are ongoing to evaluate potential therapies.
Calciphylaxis is also referred to as calcific uremic arteriolopathy.
It is most frequently observed in individuals:
- with kidney failure who are receiving dialysis
- with advanced stages of chronic kidney disease
- who have undergone a kidney transplant
Although rare, if you think you might have calciphylaxis, contact your physician promptly. Early intervention may improve your prognosis.
What are the symptoms of calciphylaxis?
The primary symptom of calciphylaxis is the appearance of skin lesions on the lower extremities or in fatty areas such as the:
- breasts
- buttocks
- abdomen
These lesions can progress to excruciatingly painful ulcers or nodules that are challenging to heal.
People with calciphylaxis may also show elevated blood calcium (hypercalcemia) and phosphate (hyperphosphatemia) levels and may exhibit features of hyperparathyroidism.
Other signs of calciphylaxis can include:
- fatigue
- weakness
- muscle cramps
- depression
- generalized aches
However, symptoms like fatigue and weakness may stem from dialysis itself rather than from calciphylaxis.
How does calciphylaxis affect the skin?
Calciphylaxis damages the skin by obstructing small blood vessels, leading to tissue ischemia and necrosis that manifest as painful lesions and nonhealing ulcers. These skin changes increase the risk of severe infection and systemic complications.
What causes calciphylaxis?
Calciphylaxis arises from a deposition of calcium (vascular calcification) within blood vessels. The specific trigger for this deposition remains unclear, and multiple mechanisms likely contribute.
One potential contributor is disturbed mineral and hormonal balance, involving:
- calcium
- phosphate
- parathyroid hormone (PTH)
The derangement in mineral handling is often attributed to kidney disease, though the precise pathway is not fully defined.
Notably, calciphylaxis can sometimes occur in people with normal kidney function, underscoring the need for further study to clarify its causes.
Who is at risk for calciphylaxis?
Calciphylaxis remains uncommon, yet its incidence appears to be rising.
Individuals with advanced kidney disease face the greatest risk, with an occurrence rate of 0.4 to 4% among people on dialysis.
Although most reports involve dialysis patients, calciphylaxis can also develop in those who:
- are obese
- use systemic corticosteroids
- take warfarin (Coumadin) for clot prevention or treatment
- use calcium-containing supplements or phosphate-binding agents
- have liver disease
- have diabetes
Occasionally, people with normal renal function receive a calciphylaxis diagnosis when they also have:
- malignancy
- inflammatory bowel disease
- hyperparathyroidism (more often secondary or tertiary than primary)
- autoimmune disorders such as systemic lupus erythematosus, Crohn’s disease, or rheumatoid arthritis
- hypercoagulable states, for example protein C or protein S deficiency
- alcohol-related liver disease
A 2024 study of patients from New Zealand and Australia reported a median age of 63 among 333 dialysis patients diagnosed with calciphylaxis, with just over half being female.
How is calciphylaxis diagnosed?
Physicians may suspect calciphylaxis when painful skin lesions are present. To confirm the diagnosis, they will perform a physical exam and often a skin biopsy — both are key in establishing the diagnosis.
Your clinician may also request tests to exclude other complications of chronic kidney disease. Diagnostic evaluations can include:
- skin biopsy
- blood tests measuring calcium, phosphorus, alkaline phosphatase, PTH, and 25-hydroxyvitamin D
- liver function tests
- kidney function tests
- infection workup, such as complete blood count and blood cultures
How is calciphylaxis treated?
At present, there is no definitive cure for calciphylaxis available. Current approaches center on:
- managing skin lesions
- preventing and treating infections
- adjusting abnormal blood levels of calcium and phosphorus
Wound and lesion care may involve:
- enzymatic debridement agents
- hydrocolloid or hydrogel dressings
- systemic antibiotics when infection is suspected
- hyperbaric oxygen therapy
- surgical debridement to remove devitalized tissue
Clinicians may also prescribe medications to treat skin wounds and normalize mineral imbalances. These can include:
- Intravenous sodium thiosulfate: an off-label chelator used to bind calcium and iron
- Cinacalcet (Sensipar): used to lower elevated calcium in people with parathyroid dysfunction or chronic kidney disease
- Noncalcium phosphate binders: to reduce serum phosphorus without increasing calcium levels — for example, consider alternatives like calcium lactate where clinically appropriate
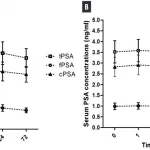
The Massachusetts General Hospital completed a clinical trial in 2019 investigating whether vitamin K supplementation can treat calciphylaxis; results have not yet been posted.
If medications fail to control calcium and phosphorus levels, surgical removal of one or more parathyroid glands (parathyroidectomy) may be necessary. Your clinician might also suggest increasing the frequency of dialysis sessions.
Because calciphylaxis is often severely debilitating, patients may need nutritional counseling, psychological support, and comprehensive pain management.
What is the outlook for calciphylaxis?
Calciphylaxis carries a high mortality risk. One-year survival is reported at under 50%. Death most commonly results from complications such as infection and sepsis.
Nonetheless, symptom control and careful management can improve outcomes, and earlier detection and treatment are linked to better results even in the absence of a cure. As research advances, survival rates are expected to improve.
Talk with your doctor about strategies to reduce modifiable risk factors and about the possibility of participating in clinical trials for new treatments.
The takeaway
Calciphylaxis most often affects people with end-stage kidney disease and those on dialysis, though it can occasionally occur in people with normal renal function. Early recognition can help improve the outlook.
The condition is driven primarily by calcium deposition in blood vessels, with other contributing factors also likely. Typical signs include painful skin lesions or ulcers.
Ongoing research into therapies aims to raise survival and quality of life. Discuss with your healthcare provider whether clinical trial participation is an option for you.























Leave a Reply
You must be logged in to post a comment.