What’s the first thing you should do after your last chemo session? It’s not “throw a party” (although you deserve one). The most powerful move is to get a clear, written roadmap of what comes next – a survivorship care plan. That document will tell you which tests you need, which side‑effects to watch for, and how to keep your body and mind thriving.
In the next few minutes we’ll walk through exactly what that plan looks like, how to stay strong physically and emotionally, and what extra challenges might pop up if you live in a rural area. I’ll also share some cool stories about medical‑student projects that are filling gaps in follow‑up care. By the end, you’ll have a toolbox you can start using today.
Why a Plan
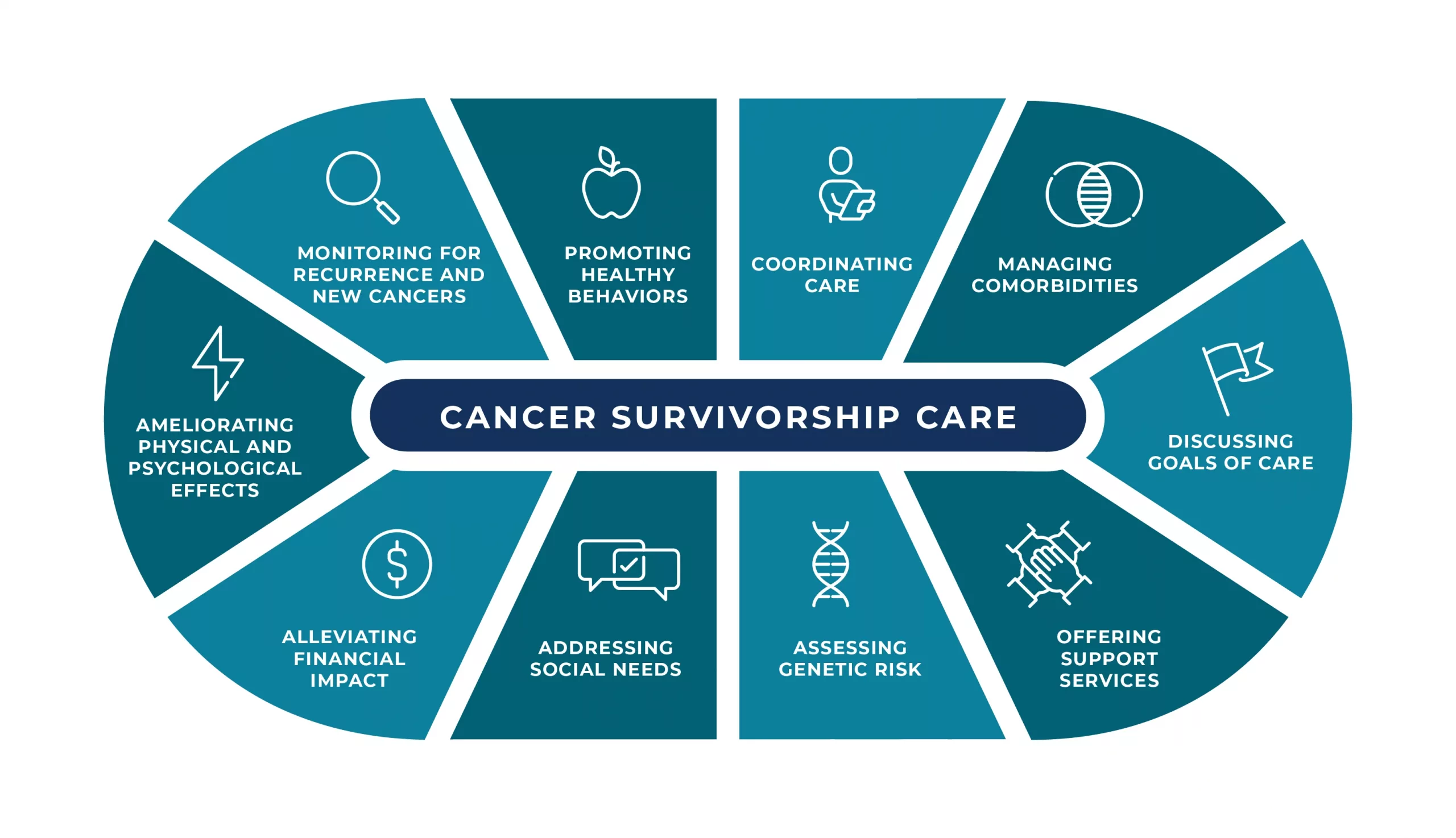
What is a survivorship care plan?
A survivorship care plan is a personalized summary of the treatments you received, the possible late effects, and a schedule for future screenings. Think of it as the “flight itinerary” for your health – you know where you’re going, when you’ll land, and what you need to pack.
Key components you can’t skip
| Component | What it includes |
|---|---|
| Treatment Summary | Dates, types of surgery, chemo, radiation, doses, and any clinical trials. |
| Risk‑Based Screening | When to get mammograms, colonoscopies, blood work, etc., based on your prior therapies. |
| Healthy‑Living Recommendations | Exercise guidelines, nutrition tips, tobacco‑free advice, and stress‑management resources. |
| Psychosocial Check‑Ins | Questions to ask your team about anxiety, depression, or financial concerns. |
How to get one (or make one yourself)
Most cancer centers now have an online tool. The OncoLife Care Plan lets you input your treatment dates and instantly generates a printable summary. If your clinic doesn’t offer a digital version, ask your nurse navigator for a paper copy and use the template above to fill in any missing details.
Why it matters (CDC says…)
According to the CDC, survivorship care plans “help survivors and providers stay informed about ongoing health risks.” In practice, patients with a clear plan are 40 % more likely to attend recommended follow‑up appointments.
Physical & Emotional Health
Common late effects you should know
Even after the cancer is gone, the body can hold on to a few “souvenirs” from treatment – fatigue, lymphedema, heart rhythm changes, or hormonal swings. Knowing which of these are realistic for you cuts down on anxiety and lets you act fast if something feels off.
Exercise: your secret super‑power
Regular movement is a game‑changer. A Mayo Clinic study found that cancer survivors who exercised at least 150 minutes a week reported lower fatigue, better mood, and a 20 % drop in recurrence risk. Start small: a 10‑minute walk after breakfast, a gentle yoga video before bed, or parking two rows farther from the store. The key is consistency, not intensity.
Nutrition: fuel for recovery
Think of food as the fuel that powers healing. A balanced plate (half veggies, a quarter protein, a quarter whole grains) supplies antioxidants, fiber, and protein needed for tissue repair. If you’re unsure about portion sizes, the Mayo Clinic offers simple meal‑planning worksheets you can print and stick on the fridge.
Mental health: don’t go it alone
It’s completely normal to feel a roller‑coaster of emotions after treatment – relief, fear, guilt, even loneliness. Peer‑support groups, either in‑person or via video, give you a safe space to vent. If you prefer one‑on‑one counseling, many survivorship clinics (like Roswell Park’s Young Adult Program) have therapists who specialize in cancer‑related anxiety.
Rural Survivors
Why distance can be a barrier
If you live outside a major city, the nearest oncology center might be a two‑hour drive away. That adds stress, travel costs, and can lead to missed appointments. According to a 2024 study, rural survivors are 30 % less likely to receive a survivorship care plan compared with urban patients.
Tele‑health and mobile clinics
Tele‑medicine has exploded since the pandemic. A recent pilot in the Midwest showed that video visits cut travel time by 45 % and kept 92 % of participants on schedule for follow‑up labs. When a physical exam is needed, some health systems deploy mobile “clinic vans” that bring imaging and lab services directly to the community.
Practical tips you can start today
- Keep a digital “care journal” on your phone – note meds, side‑effects, and upcoming appointments. The OncoLife portal even lets you export this data.
- Identify a local primary‑care doctor you trust; they can order routine blood work and refer you back to the oncology center when a scan is required.
- Ask your oncologist if there’s a regional survivorship coordinator who can serve as a liaison.
For more on navigating health services far from the city, check out our guide on rural cancer care and the broader look at rural healthcare access.
Student Innovations
How medical‑student projects are closing gaps
Across the country, enthusiastic med‑students are creating low‑cost navigation apps, community‑based follow‑up clinics, and survivor‑mentor programs. One initiative at a Midwest university paired seniors with student volunteers who called monthly to check on medication adherence – the program lifted appointment‑keeping rates by 30 %.
Examples you can emulate
- Survivorship Navigation App: A simple phone app that stores your treatment summary, sends reminders for scans, and lists local support groups.
- Community Health‑Fair Booths: Students set up kiosks at rural fairs to distribute survivorship checklists and educate on lifestyle changes.
- Peer‑Mentor Networks: Recent graduates who are themselves survivors mentor newly finished patients, offering practical advice and emotional support.
Read more about the inspiring work happening in our medical student initiatives section.
Follow‑Up Timeline
First‑year checklist
In the first 12 months after treatment, most oncologists recommend:
- Physical exam and blood work every 3–6 months.
- Imaging (CT, MRI, or mammogram) based on your original cancer type.
- Vaccinations – flu yearly, COVID boosters as advised, and shingles if you’re 50+.
- Heart‑function tests if you received anthracyclines or chest radiation.
Long‑term schedule (years 2‑5 and beyond)
| Year | Key Actions |
|---|---|
| Year 2‑3 | Annual physical + blood work; imaging per risk; psychosocial screening. |
| Year 4‑5 | Continue annual labs; reduce imaging frequency if clear; consider bone‑density scan. |
| Every 5 years | Comprehensive wellness visit – cardiology, endocrinology, and survivorship clinic. |
Who should you see?
Early on, stay with your oncology team for disease‑specific monitoring. After the first year, a primary‑care physician (PCP) can take over routine labs and preventive care, while you still schedule an annual “survivorship check‑in” with your oncologist or a dedicated survivorship clinic.
If you’re hunting for concrete, ready‑to‑download templates, our follow‑up care solutions page has printable calendars and symptom‑tracking sheets.
Key Takeaways
1️⃣ Get a survivorship care plan – it’s your health GPS.
2️⃣ Move your body – even gentle activity pays big dividends for mood and recurrence risk.
3️⃣ Eat smart, sleep well, stay smoke‑free – the basics still win the day.
4️⃣ Seek mental‑health support – feelings are real, and help is out there.
5️⃣ If you’re rural, leverage tele‑health and local PCPs – you don’t have to travel alone.
6️⃣ Watch out for student‑run programs – they often bring fresh, free resources right to your doorstep.
7️⃣ Stick to a follow‑up timeline – regular labs and scans catch problems early.
Remember, survivorship isn’t a passive “wait‑and‑see” phase; it’s an active partnership with your health team and yourself. Grab that care plan, set a small weekly goal (maybe a 15‑minute walk), and watch how confidence builds. If you have questions, or just want to share what’s working for you, feel free to reach out. Your journey inspires the next survivor – let’s walk it together.





















Leave a Reply
You must be logged in to post a comment.