Oxford University researchers dropped a bombshell this summer. Their programmable microcapsules could let us ditch the whole “multiple jab” nightmare for malaria. Imagine giving one shot, walking away, and the body handling the rest on auto-pilot. WHAT? That’s not science fiction—this is happening right now. Here’s why this matters: booster shots are a killer, but we’ll get to that later.
But let’s zoom out for a second. You’re not just here to hear about random lab experiments, right? You want the brutal, unfiltered truth about why diseases like malaria keep winning in poor regions. You want to know: “Could this fix the mess?” and “What’s the catch?” Consider your questions answered. Let’s keep it real, not corporate.
Challenges: Why Vaccines Keep Getting Stuck
Lemme clue you in: The vaccine itself isn’t the problem. It’s delivering it to families where it’s needed most. Tiny villages in tropical heat? That’s a logistical hell on Earth. Ever tried hauling a cooler through mud during monsoon season? Yeah, the people doing this work are warriors. But even warriors trip over big rocks—rock like these:
Broken Transport? That’s the Starting Line.
You need roads to get vaccines where they’re supposed to go. Except… the roads don’t exist? One study found health workers in Nigeria spend half their day on transport jams. Vaccines get delayed, spoil in the heat, or just never arrive. Chips fall where they may.
Cold Chain? It’s Hurtin’.
Vaccines are like fresh sushi—you can’t leave them warm for too long. RTS,S expires when storage temps flake out. So far, solar-powered coolers helped, but WHO notes they’re a short-term hack. Protect a dose exposed to +30°C heat? No luck. That’s a $500 wasted shot—just like that.
Vaccine Hesitancy Is Real (And Tricky)
Sometimes, the issue isn’t the syringe—it’s the person it’s meant for. One nurse in Kenya said, “A grandma thought the malaria shot made kids sleepy. Another thought it would cause crocodile dreams.” Yikes. Misinformation gets wild in places where risk perception is low. “Terrible parasite? Nah, just bad spirits,” said an old superstition once… probably.
Say Hello to RTS,S and R21: Current Vaccines In Action
No Free Lunch—These SHots Need Schedules
Right now, you’ve got two big guns:
1. RTS,S/AS01 (Mosquirix): First jab at 5 months, then monthly shots up to 17 months. Still, even after four pins (yes, 4!), protection is partial. WHy? Because malaria is twisted.
2. R21/Matrix-M: Cleaner than RTS,S, lower side effects. First shot at five months, fourth at 17–same as Mosquirix. Two vaccines, both needing tracking spreadsheets. Now imagine how many zeroes in that Excel document. Got a headache yet?
But They Fight for Lives (Proven Stats)
Let’s not trash-talk these vaccines—they’re heroes. CDC notes RTS,S reduces malaria cases by 40% and deaths by 13%. Not a free pass, but it’s been used since 2019 to protect 800,000+ kids in Malawi and it reduced hospital visits. R21 kicked in three years later with even better trial numbers.
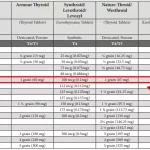
| Vaccine | Vaccination Rounds | Storage Needs | Current Coverage |
|---|---|---|---|
| RTS,S | 4 doses | Cold chain | 1.5M+ children |
| R21 | 3-4 doses | Cold chain | Country-specific |
| Programmable Microcapsules | 1 shot | No strict cold storage?In trials |
Skip the Boosters? Here’s How Microcapsules Could Do It
Science that Feels Like Magic
Okay, time to unpack Oxford’s tech. It’s not sci-fi—it’s smart chemistry. Their lab team engineered capsules that burst weeks after injection. First dose? Goes in. Second? The delayed release. Third? Still tricky—if a one-shot system becomes reliable, they could theoretically add multiple boosters in one needle. Like launching a satellite clump with programmed launch windows. Badass.
Booster Shot Alternative = Better Immunization Coverage
You know what’s better than chasing kids for three more shots? Not… doing that. With missing doses, efficacy drops fast. But one shot? Locks it in. WHO says this could bring immunization coverage to 10% more families in Burkina Faso, Niger, and beyond. That’s fewer missed opportunities to stop a killer.
Real Talk: So Are Microcapsules the Fix or Just Hype?
If It Works… This Changes Everything
Here’s the pitch: Transport problems? Reduced. Cold chain? Maybe optional someday. Nurse visits for dose four? Erased. If Oxford nails single shot malaria vaccine delivery, infant immunization in poor nations leaping forward. Nigeria alone, with 70M kids under five, would get a mega win. Plus, fewer negative stories about doctors poking babies? Builds trust long-term.
The Catch? Yeah, There’s One.
No vaccine wizardry comes flawless. Microcapsules might look sweet on slides, but how about scaling mass production? If every child in Africa and South Asia needs this new pill? Factories cranking 24/7 might still stumble. Plus, mirroring parasite stages inside a slow-release capsule? The malaria parasite has more forms than a Transformers movie. But hey, science is figuring it out—slow, messy progress, but it’s real.
No More “Scheduling Drama” – Matching Solutions to Problems
If we swap traditional vaccines for programmable tech—which parts get easier? Which pieces need more tools? Let’s break it down like a blood sample:
Rural Clinics Deserve This Win
Right now, you’ve got nurses operating off-grid, ice packed in bike coolers. WHO did a pilot where only 30% had consistent vaccine availability. One health officer said, “We try. But miles to drive, cold shelves broken, and sometimes people see needles as bad luck. The new tech makes sense.”
Training Heroes Without Corporate Babble
Want more immunization coverage? Fix this: train natives who speak the language, clearly explain “single shot vaccine” benefits. Gavi cites that a trained health worker increases uptake by 21%. That’s not some quarterly report talking point; it’s boots on the ground doing what they can.
To Avoid Hesitancy—Meet Communities Where They Are
Look, skeptical folks are not stupid. They hear “malaria vaccine,” their cousin got sick, the clinic runs out, so they drop out. To fix it, you don’t tweet facts—you listen. Nurse M’Bala runs a rural station in the Congo. She says, “After a drought ruined food crops, people thought medicines were vanishing. We walked house to house. Shared stories. Then… they lined up for shots easily.” That’s how you grow trust, not check a “vaccine campaign” box.
Next Chapter of Vaccination Tech
Sixty Years to Get Here – Now What?
Malaria vaccines are slow burn projects. WHO started testing in the 80s, 40 years later dropped R21. WHY? Two big hurdles:
- Parasite plays hard to reach—goes through six phases before hitting blood. Catching one isn’t enough.
- Vaccine science has limits—still learning which stages need blocking, how strong a binder link between shot and immune response is required.
What Needs to Happen Before This One-Shot Thing Takes Over?
We’re not handing these to kids tomorrow. Oxford’s tech needs:
- Phase trials across varied species
- WHO and Gavi saying “Yeah, safe and scalable”
- Factories cranking
Still growing pains. But hey, nothing about erasing a disease of this scale is a smooth process. There’s excitement, for sure. But let’s not italicize “every village, every child” just yet. Baby steps.
Can you imagine a world where this tech spreads beyond malaria? Practical dreams like rubella, TB, HIV vaccines becoming “one-time-only pokemon catches” for healthcare. It’s far, but opening this door feels worth it.
So… what’s your take? Would a single shot solution flip the script in low-income nations? Drop your thoughts—or if you need: More details, questions, rants welcome. I read every comment.
Tell me what got your gears turning. Was it the travel dilemma? The trust-building bit? It’s all connected. Malaria vaccine delivery is a tangled web—and the breakthroughs worth celebrating. Keep reading. Stay curious.












Leave a Reply
You must be logged in to post a comment.