Ever noticed that a summer that feels “just right” for most people suddenly feels like a furnace when you’re taking certain pills? You’re not imagining it. A surprising number of prescription and over‑the‑counter medications can throw a wrench into your body’s natural cooling system, turning a sunny day into a health hazard. Below is the low‑down on why this happens, which drugs are the usual suspects, and everything you can do to stay cool, comfortable, and safe.
Quick Answer
Short version: Some drugs mess with sweating, blood flow, and hydration, making you more prone to heat intolerance and heat‑related illness. The biggest culprits are certain antidepressants, antihistamines, blood‑pressure medicines, diuretics, antipsychotics, and a handful of OTC products. To protect yourself, stay well‑hydrated, avoid prolonged exposure to extreme heat, and talk to your prescriber about possible alternatives or timing adjustments.
Need a deeper dive? Check out our guide on prescription drugs heat risk for a quick checklist.
How It Works
The Body’s Cooling System
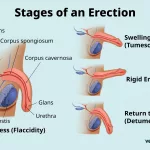
When the thermostat in your brain—the hypothalamus—detects a rise in core temperature, it flips a switch that tells sweat glands to fire up, blood vessels near the skin to widen (vasodilation), and respiration to speed up. The sweat evaporates, pulling heat away from your body, while the extra blood flow carries warmth to the surface where it can be released.
According to a Harvard Chan study, several medication classes interfere with one or more of these cooling mechanisms, leaving you “stuck in a sauna” even when the temperature isn’t extreme.
What Breaks the System?
Medications can disrupt cooling in three main ways:
- Anticholinergic effects: many drugs block acetylcholine, a neurotransmitter that triggers sweat production. Fewer sweat droplets mean less evaporative cooling.
- Fluid loss or reduced thirst: diuretics and some blood‑pressure agents increase urine output or blunt the thirst reflex, so you may become dehydrated without even noticing.
- Central nervous system (CNS) interference: certain psychiatric drugs alter the hypothalamic set‑point or blunt the body’s signals that tell you to seek shade or drink water.
Quick Reference Table
| Mechanism | Medication Class | Typical Symptom | Why It Matters |
|---|---|---|---|
| Reduced sweating | First‑gen antihistamines, antipsychotics | Dry skin, overheating | Body can’t lose heat efficiently |
| Increased urine output | Thiazide & loop diuretics | Dehydration, dizziness | Less fluid means less sweat |
| Altered hypothalamic signaling | SSRIs, SNRIs, stimulants | Unexplained fever, fatigue | Temperature set‑point rises |
Medication Classes
Psychiatric & CNS Drugs
Antidepressants—especially SSRIs (e.g., fluoxetine, sertraline) and SNRIs (e.g., duloxetine, venlafaxine)—raise serotonin levels, which can increase core temperature and, in many cases, produce anticholinergic side effects that curb sweating. Antipsychotics, both typical (e.g., haloperidol) and atypical (e.g., olanzapine), can also mess with the hypothalamus, making you feel hotter than the mercury actually is.
Stimulants prescribed for ADHD (like methylphenidate) constrict blood vessels in the skin, reducing the heat‑dumping effect of vasodilation. If you’re on any of these, keep a water bottle handy and schedule outdoor errands for the coolest part of the day.
Cardiovascular & Diuretic Drugs
ACE inhibitors, ARBs, calcium‑channel blockers, and especially thiazide or loop diuretics are notorious for promoting fluid loss. They may also diminish thirst sensation, so you might sip less water even as your body’s water stores dwindle.
When you’re on a diuretic, aim for at least 2 liters of fluid daily (more if you’re active). Adding an electrolyte‑rich drink can offset the sodium loss that diuretics cause. Heat illness prescription medications often include these cardiac drugs, so it’s worth reviewing your regimen during a heat wave.
Antihistamines & Decongestants
First‑generation antihistamines (diphenhydramine, chlorpheniramine) are classic anticholinergics. They dry up your mouth, eyes, and—crucially—your sweat glands. Decongestants like pseudoephedrine raise blood pressure and can also reduce sweating. If you need allergy relief in the summer, consider a second‑generation, non‑sedating antihistamine that isn’t as heat‑sensitive.
OTC & Other Common Culprits
Non‑steroidal anti‑inflammatory drugs (NSAIDs) can impair kidney function, aggravating dehydration. Some antibiotics, especially those that cause fever as a side effect, can combine poorly with hot weather. Even cholesterol‑lowering statins have been reported—albeit rarely—to increase heat intolerance in older adults.
Quick‑Check Box
- Do you take an SSRI or SNRI?
- Are you on a diuretic or blood‑pressure pill?
- Do you reach for Benadryl during allergy season?
- Are you on a stimulant for ADHD?
If you answered “yes” to any of these, you’re in the high‑risk group and should read on.
For a broader list, see our article on drugs that increase heat risk.
Who Is At Risk?
Age & Health Status
Older adults (65+) naturally lose some sweating capacity and often take multiple medications, a perfect storm for heat sensitivity. Children’s thermoregulation isn’t fully mature either, making them vulnerable during outdoor play.
Chronic conditions—diabetes, cardiovascular disease, multiple sclerosis, thyroid disorders—already tax the body’s ability to regulate temperature. Adding a heat‑risk medication can tip the balance from “a bit warm” to “dangerously hot.”
Lifestyle & Environment
Outdoor workers, athletes, and anyone who spends long hours in direct sun are on the front lines. Low fluid intake, alcohol consumption, and high‑humidity environments all amplify the heat‑risk effect of medication.
Polypharmacy & Interactions
Taking two or more heat‑sensitive drugs multiplies the risk. For example, an antihistamine plus a diuretic can simultaneously block sweating and dehydrate you. If you’re juggling several scripts, ask your pharmacist for a “heat‑risk review.”
Learning about all the ways meds can affect heat tolerance is part of the heat-related illness medications conversation you should have with your health team.
Spotting Symptoms
Mild Heat Intolerance
The early warning signs are often subtle—and easy to dismiss as “just being hot.” Keep an eye out for:
- Excessive thirst that feels abnormal
- Light‑headedness or a “spinning” sensation
- Headache or “brain fog”
- Nausea, vomiting, or an upset stomach
- Flushed, reddened skin without a rash
- Muscle cramps or weakness
Escalation: Heat Exhaustion → Heat Stroke
If those mild signs linger, you may be sliding toward heat exhaustion: rapid heartbeat, heavy sweating (or paradoxically, lack of sweat), dizziness, and a temperature climbing above 100.4 °F (38 °C). Without prompt cooling, heat stroke can follow, marked by confusion, seizures, or loss of consciousness, and a core temperature over 104 °F (40 °C). Heat stroke is a medical emergency—call 911 immediately.
Action Flowchart
| Step | What to Do |
|---|---|
| 1 | Move to a shaded or air‑conditioned area |
| 2 | Drink cool (not ice‑cold) water—aim for 8‑oz every 15‑20 minutes |
| 3 | Loosen clothing; apply cool compresses to neck, armpits, and groin |
| 4 | If symptoms worsen (confusion, fainting, no sweat), seek emergency care |
Stay Safe Strategies
Medication Management
Never stop a prescribed medication without your doctor’s guidance. However, you can discuss:
- Adjusting the time of day you take a diuretic (e.g., morning instead of evening).
- Switching to a lower‑risk alternative (e.g., second‑generation antihistamine).
- Evaluating the necessity of each “as‑needed” drug during peak heat months.
Hydration & Electrolytes
Water is your best friend, but plain water alone might not replace lost salts if you’re on a diuretic. A sports drink with a balanced sodium‑potassium mix can help. Aim for at least 2 L (about 8 cups) of fluid each day, more if you’re sweating heavily.
Environmental Controls
Simple tweaks make a big difference:
- Keep blinds or curtains closed during the hottest part of the day.
- Use fans in conjunction with air‑conditioning to circulate cool air.
- Schedule outdoor activities before 10 a.m. or after 6 p.m.
- Wear lightweight, breathable fabrics—think cotton or moisture‑wicking sports wear.
- Carry a cooling towel or misting spray bottle for quick relief.
Emergency Planning
Consider creating a “heat‑alert card” that lists all your medications, dosage, and any known heat‑sensitivity. Slip it into your wallet so EMS personnel have instant access.
Lastly, keep a personal “heat‑check” reminder on your phone—something like “Drink water & check meds” that pops up twice daily during summer months.
Resources & Further Reading
For deeper scientific background, check out these trusted sources:
- CDC’s heat‑related illness guidance (search “heat and medications” on the CDC site).
- Harvard T.H. Chan School of Public Health’s commentary on medication‑induced heat sensitivity.
- MedlinePlus’s overview of drugs that can cause heat intolerance.
- American Society of Health‑System Pharmacists (ASHP) heat‑risk medication list.
Conclusion
Heat waves are becoming a regular part of life, and the medications we rely on for chronic conditions can unintentionally make those sweltering days dangerous. By understanding which drug classes interfere with your body’s cooling system, recognizing early warning signs, and taking practical steps—hydration, smart timing, and open conversations with your health team—you can stay cool without sacrificing the benefits of your treatment.
Remember, you’re not alone in this. If you ever feel uncertain about a medication’s heat risk, reach out to a pharmacist or physician; they’re there to help you navigate these tricky waters. Stay safe, stay hydrated, and enjoy the sunshine—just a little more wisely.






















Leave a Reply
You must be logged in to post a comment.