Picture this: you’re at a family barbecue, the sun is blazing, the grill is sizzling, and you feel a little bit warm—nothing out of the ordinary, right? Now imagine that the same warmth turns into a pounding headache, dizzy spells, and an overwhelming need to sit down. The culprit might not be the sun alone; it could be a pill you’re taking. Certain medications turn your body’s natural thermostat upside‑down, making you far more vulnerable to heat‑related illness. Below we’ll unpack which drugs do this, why they matter, how to spot the danger early, and what you can actually do—including safe deprescribing—so you can enjoy the season without sweating your health away.
Why Heat Risk Matters
Heat‑related illnesses—heat exhaustion, heat stroke, and hyperthermia—are not just “bad days”; they’re life‑threatening emergencies. In the United States, the CDC reports a 30 % jump in emergency‑room visits for heat stroke during the hottest weeks of the year. The World Health Organization flags medication‑induced thermoregulation failures as a hidden driver of these spikes, especially among older adults and people on multiple prescriptions.
When a drug interferes with how we sweat, circulate blood, or generate metabolic heat, even a mild summer day can become a hazardous “heat trap.” The more pills you’re juggling, the higher the “prescription drugs heat risk.” Knowing which medications are the usual suspects is the first line of defense.
How Meds Disrupt Thermoregulation
What Physiological Pathways Are Affected?
Our bodies keep a steady core temperature (around 37 °C) by balancing heat production and heat loss. Several drug classes throw a wrench into this delicate dance:
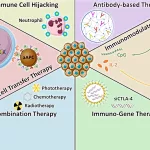
- Anticholinergics (e.g., atropine, amitriptyline, diphenhydramine) block the nerve signals that stimulate sweating, so you can’t off‑load excess heat.
- Non‑selective beta‑blockers (propranolol, nadolol) blunt heart‑rate acceleration and peripheral vasodilation, limiting the body’s ability to pump warm blood to the skin.
- Sympathomimetic stimulants (MDMA, methamphetamine, cocaine) crank up metabolism and muscle activity, flooding the system with extra heat.
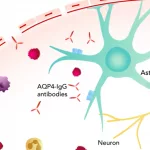
- Antipsychotics and dopamine antagonists can trigger neuroleptic malignant syndrome, a rare but catastrophic hyperthermic state.
- Serotonergic agents (SSRIs, MAOIs, tramadol) may lead to serotonin toxicity, which also raises core temperature.
- Anti‑Parkinson’s drugs (levodopa, selegiline) increase dopamine‑driven thermogenesis.
Scientific Back‑up
According to a 2012 study in the Journal of Medical Toxicology, drug use was linked to higher morbidity and mortality in heat‑stroke patients, especially when anticholinergic or sympathomimetic agents were involved (a study).
A 2024 systematic review and meta‑analysis of core‑temperature responses during heat stress found moderate‑quality evidence that high‑anticholinergic drugs, non‑selective beta‑blockers, adrenaline, and anti‑Parkinson’s agents each raised core temperature by 0.1 °C–0.4 °C under hot conditions (a study).
High‑Risk Drug Classes
| Drug Class | Typical Examples | How It Raises Heat Risk | Common Uses |
|---|---|---|---|
| Strong Anticholinergics | Atropine, Amitriptyline, Diphenhydramine | Blocks sweat glands → less heat loss | Depression, allergies, motion sickness |
| Non‑selective Beta‑Blockers | Propranolol, Nadolol | Reduces cardiac output & peripheral vasodilation | Hypertension, migraine prophylaxis |
| Sympathomimetics / Stimulants | MDMA, Methamphetamine, Cocaine | Boosts metabolic heat production | Recreational use, ADHD meds (methylphenidate) |
| Antipsychotics / Dopamine Antagonists | Haloperidol, Olanzapine | Possible neuroleptic malignant syndrome | Schizophrenia, bipolar disorder |
| Serotonin‑Modulating Agents | SSRIs, MAOIs, Tramadol | Serotonin toxicity → hyperthermia | Depression, chronic pain |
| Anti‑Parkinson’s Drugs | Levodopa, Selegiline | Increases dopamine‑driven heat production | Parkinson’s disease |
Case vignette: Mrs. Patel, 68, had been on amitriptyline for chronic neuropathic pain for years. One sweltering July weekend, she spent an afternoon gardening without enough water. By late afternoon, she felt dizzy, her skin was dry, and her temperature spiked to 39 °C. EMS diagnosed heat stroke, attributing it partly to the anticholinergic effect of her medication. After a brief hospital stay, her physician switched her to a low‑risk antidepressant and added a proactive heat‑safety plan.
Early Warning Signs
Heat‑related trouble doesn’t always announce itself with a dramatic flare‑up. Keep an eye out for these subtle—but critical—signals, especially if you’re on any of the drugs listed above:
- Unexplained feeling “too hot” even in shade.
- Rapid heart rate (> 110 bpm) without exertion.
- Dry mouth, absent or reduced sweating.
- Nausea, vomiting, or sudden confusion.
- Muscle cramps, rigidity, or seizures.
If you notice any of these, act fast: move to a cool environment, hydrate with electrolytes, apply cool compresses, and call emergency services—mention every medication you’re taking. Early intervention can mean the difference between a night in the ICU and a quick recovery.
Reduce Your Heat Risk
Medication‑Review & Deprescribing Toolkit
Not every medication needs to be abandoned, but a thoughtful review can uncover safer alternatives. Here’s a quick checklist you can run through with your prescriber:
- List every pill, supplement, and over‑the‑counter product. Include “as needed” meds.
- Identify the heat‑risk rating. (Low / Medium / High). Use our prescription drugs heat risk guide for a quick reference.
- Ask about alternatives. For example, replace a non‑selective β‑blocker with a cardio‑selective β‑1 blocker, or swap a strong anticholinergic antidepressant for a newer, less thermally active SSRI.
- Set a monitoring plan. Schedule a follow‑up after any change to track blood pressure, mood, or Parkinson’s symptoms.
Many clinicians welcome a proactive approach—especially when you frame it as “I want to stay safe this summer.” It shows you’re engaged and reduces the chance of abrupt, unsafe discontinuations.
Lifestyle Adjustments While Staying on Needed Meds
- Hydration is non‑negotiable. Aim for at least 2 L of water daily, plus electrolytes if you’re sweating heavily.
- Timing matters. Schedule outdoor activities before 10 am or after 6 pm when ambient temperatures dip.
- Dress smart. Light‑colored, breathable fabrics, and a wide‑brimmed hat can shave a few degrees off your skin temperature.
- Cool‑down tools. Portable fans, cooling towels, or a misting bottle can be lifesavers on a hot porch.
- Know your environment. Humidity hampers sweat evaporation. If the heat index tops 95 °F (35 °C), pause outdoor plans.
Even simple tweaks like sipping water every 30 minutes, rather than waiting for thirst to hit, can keep your core temperature steady.
Talk to Your Doctor About Deprescribing
Deprescribing isn’t “stopping medication”; it’s a collaborative, evidence‑based process to trim unnecessary drugs while safeguarding health. Here’s a friendly script you could try:
“I’ve read that certain meds can make heat stroke more likely, and I’m planning to be outdoors a lot this summer. Could we review my current list and see if any can be lowered in dose or swapped for something cooler?”
Bring a printed list (including OTCs) and note any heat‑related symptoms you’ve experienced. Your doctor may suggest a gradual taper, especially for drugs that affect the nervous system, to avoid withdrawal or rebound effects.
For extra reassurance, you can also explore our heat illness prescription medications resource, which breaks down each drug’s risk profile and offers safer alternatives.
Bottom‑Line Takeaways
– Certain drugs—especially strong anticholinergics, non‑selective β‑blockers, stimulants, and some antipsychotics—mess with the body’s thermostat, raising the chances of heat‑stroke or severe dehydration.
– Recognize early warning signs (unexplained heat, rapid heart rate, dry skin, nausea, confusion) and act immediately.
– Conduct a medication review, discuss deprescribing or substitution with your prescriber, and stay hydrated, cool, and smart about timing.
– Use trusted resources like medications and heat sensitivity and heat‑related illness medications to stay up‑to‑date.
Summer’s a season of sunshine, barbecues, and good vibes—but it shouldn’t be a season of hidden medical danger. By understanding which drugs that increase heat risk you’re already ahead of the curve. Stay curious, stay safe, and remember: a little proactive conversation with your doctor can keep the heat where it belongs—outside, not in your core temperature.






















Leave a Reply
You must be logged in to post a comment.