Ever tried powering through the day on four hours of sleep? Yeah, me neither… and honestly, I wouldn’t want to. But for active-duty military personnel, sleep deprivation isn’t just a bad night—it’s a way of life. And when sleep-related breathing disorders like obstructive sleep apnea are thrown into the mix? It turns into a real messy cycle. Let’s unpack this.
Here’s the deal: Over 1 in 10 active-duty Soldiers in the U.S. military have a diagnosed sleep disorder, with OSA leading the charge. This isn’t just about snoring loudly enough to wake your barracks. We’re talking increased risks of heart problems in military life, mood meltdowns, and even reduced mission readiness. Basically, sleep apnea is like having a saboteur in your own body during critical moments. (That’s not a metaphor—studies back it up.)
Why Sleep Apnea Plagues Soldiers
Combat, chaos, and caffeine. Oh my. Military life isn’t exactly a spa retreat. Shift work, jet lag from deployments, and stress are baked into the culture. But guess what? All these things are like fuel for the sleep disorder fire. Let’s break it down:
Obstructive vs. Central Sleep Apnea: Which Is More Common?
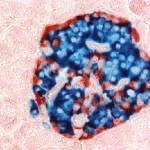
There’s a key difference between the two. The obstructive type is when your airway literally collapses while you snooze—like a soda straw getting kinked. Central? It’s your brain hitting snooze on the breathing button. But in the military, OSA dominates. Why? Simple: physical training, weight gain, and the “just power through” attitude often lead to those signature symptoms like loud snoring and daytime exhaustion.
PTSD and Sleep Apnea: A Ticking Time Bomb
You’ve probably heard PTSD and trauma responses are linked to sleeping issues. But what if your trauma isn’t just keeping your eyes open at night—it’s actively poisoning your sleep depth? A 2025 joint study from the Uniformed Services University and University of Maryland found that Soldiers with OSA are four times more likely to develop PTSD and three times as likely to suffer a traumatic brain injury compared to peers without the condition. Why? Sleep fragmentation from apnea episodes messes with memory consolidation, emotional regulation, and reaction time.
Translation? If you’re a Soldier dragging after a sleepless night, you’re not just groggy—you’re wired for anxiety, irritability, and you guessed it—another round of choking during sleep. It’s a loop, but the good news? The Army’s been quietly deploying oral appliances that make a real difference. We’ll get to those later.
Time Zones, Black Coffee, and Sleep Zombies
Military life’s nonstop time-zoner is a sleep apnea dream team member. Take shift changes: you’re up for a night patrol, asleep by 10 AM, and expected to function like a war machine by noon. Oh, and caffeine? Sure—it’ll keep you wired during guard duty. But when it’s time to crash? That’s when all hell breaks loose. Stimulants/sedatives near daily? Big fat risk factor. Add chronic stress, and yeah… even your jaw tightens up, partly restricting airflow.
The Sneaky Health Debacle: Heart Issues, Mental Health, and More
Here’s the kicker: sleep apnea in the military isn’t just about choking yourself awake 60 times a night. It’s about blood pressure spiking, relationships fraying, and deployments going sideways because someone’s mentally checked out. Let’s get into it:
Sleep Apnea and Heart Disease – What Do Soldiers Risk?
Think OSA is just noisy? Think again. Your cardiovascular system takes a major hit. Obstructive sleep apnea causes intermittent hypoxia (translation: your blood gets low on oxygen, even if you’re unaware). Over time, that means vasoconstriction, higher cortisol, and… heart failure. Ominous, I know. But the military health units aren’t sleeping on this either. In fact, conditions like OSA have been tied to 28% of recorded aviation waivers, where pilots need near-perfect AHI (Apnea Hypopnea Index) scores to fly.
Mood Swings, Depressions, and That “Empty” Feeling
Soldiers: You’re not alone if your usual mood feels like Mr. Hyde after yer “sleep”. A 2020 Army health study found that those clocking less than 6 hours of sleep were 10-15% less productive… and way more likely to report depression or anxiety. Obstruct sleep apnea creates a unique kind of exhaustion. It’s not just physical fatigue—it’s mental fog. You’re running on empty. And it shows.
Real talk: Some Soldiers I’ve spoken to describe it like they’re sleepwalking through their missions. They’ll be on patrol, but their brain feels misty. Or they’re sharing a tent, and their buddy’s snoring sounds like an F-16… and they don’t say a word because “talking about it feels weak.”
How Many More Emergency Room Trips Wait for Untreated Sleep Apnea?
A lot, according to the latest Military Health System data. Soldiers with untreated OSA had 1,852 more ER visits per year and 66 additional hospitalizations. And it’s not a fluke—the figures are staggering across multiple studies… and decades. The numbers don’t lie, even if rank-and-file personnel ignore them.
Diagnosing and Treating Sleep Apnea in the Field
You can’t exactly book a luxury sleep study in a combat zone. But the military’s getting creative. Let’s take a look at how OSA gets diagnosed and patched in the U.S. military.
PSG vs. Home Sleep Tests – What Do Medics Use?
For the record, Polysomnogram (PSG) is military jargon for the gold standard test. But in the field, that’s not always an option. That’s where home sleep apnea tests (HSATs) come in. Can you imagine? Setting up six sensors in a desert base and still getting accurate results on the spot? Yep, new military tech makes it possible—and data-driven.
CPAP or Oral Appliance? What’s the Military Using Now?
Let’s get real. Smacking a loud, jelly-hose CPAP into a bunk during a blackhole blackout? No joy. That’s why the Army’s been quietly investing in custom oral appliances. Think mouthguard—but it’s not just custom. It’s crazy effective for mild to moderate OSA and costs less than 1/3 of a CPAP’s annual upkeep. I spoke to one paratrooper who laughed about how “the only injury I’ve ever prevented was with jaw technology.”
CPAP vs. Oral Appliance – Pros and Within-Budget Comparisons
| CPAP Machine | Oral Appliance |
|---|---|
| Mild sedation + OSA sufferers: often switch to this | Frequent deployments—easier to pack and portable |
| Effective, but low compliance in field settings | Expert-fitted, but sometimes stigmatized as “snoring goggles” |
| Cost: $500–$2,000 + maintenance fees | Cost: ~$200 per flight, reusable with fewer replacements |
| Risk for Emergency docs: 30% of untreated Soldiers end up there | Risk if ignored: same, but cheaper upfront—and less gear in the way |
Sleep Apnea and Military Service: What You Can Do
Many of you may have more gear than gear painted on your skin, but what about the big question: Can you still serve with this madness? Spoiler: You might. But success isn’t about pretending you’re fine.
Deployment Waivers – How to Stay Mission-Ready with OSA
If you’ve battled through deployments with undiagnosed fatigue, congrats—they’re not discharging you for that YET. But a waiver requires one thing: proof you can control your AHI (Apnea Hypopnea Index) to below 5 events/hour—especially if you’re an aviator. The Aeromedical Policy Letters from the Army are pretty strict about ensuring pilots and crew are awake and oxygenated. And if you’re a driver or gunner? It might mean saving lives vs. endangering them.
VA Benefits and Claims
Veterans: If you drummed up OSA while on active duty, you’re eligible to file a claim. PTSD and undiagnosed obstructive sleep apnea in medical records + combat exposure = better case. Check with your VA liaison. And don’t shrug it off with a “so what?”—this condition affects long-term benefits, especially for heart problems years down the road.
Military’s Fight Against Sleep Apnea – And Why it Still Misses the Mark
Rearranging sleep missions… and remote health options. The military’s not sitting idle. Let’s talk turkey on their progress.
Tele-Sleep OSA: Online Treatment Triage
Does this study ever sound like it came from the Pentagon? Because it’s real and straight off a 2025 CHEST study. The University of Maryland and USU teamed up for a clinical trial called “Tele-Sleep OSA” to assess virtual care for OSA in the field. Why? Because sleep specialists in active-duty units are rarer than shovels on a firing range. Less than 40 active-duty sleep physicians exist to serve an entire Army.
Dental Therapy: Army’s Undercover Solution
Remember that “snore guard” in the mouth? It’s not an inside joke—it’s a calculated move by dental and command units. At one U.S. Army Dental Lab, over 400 custom devices were made in 2023 alone, with Soldiers citing better sleep, fewer musculoskeletal injuries, and improved mood. It’s not groundbreaking tech… but adaptation matters a ton.
The Stigma That Still Exists
Let’s keep it real. Talking about sleep fatigue in the military? Can feel like confessing weakness to your drill sergeant. (Soldiers told me they hid snoring to avoid being labeled “the sleepy one.”) This stigma is quiet but potent—and our poker face when discussing health risks needs some revising.
The Final Word: You’re Not Alone… And Sleep Matters
So what does this all boil down to? Your health, sleep, and bravery shouldn’t come at the cost of staying silent about apnea. Untreated sleep apnea in the military robs Soldiers of energy, elevates heart problems, and, yeah, even messes with aviators and shooters. But more than that: it’s solvable. If you’re being woken by your own choking… or you’re catching extra naps because you’re in survival mode? Don’t walk away. Arm yourself with knowledge—and maybe a custom oral appliance.
And here’s the real message: OSA isn’t exclusive to generals or grunts. It affects moms and majors alike. If you’ve got dark circles under your eyes, you’re not the only one. The military’s getting better at approaching this sleep disorder—from more HSAT options to updated medical care costs for dental appliances—but we’re not home free. Talking gets you there faster than silence.
At the end of the day: Your mission lives and dies on how well-rested you are. Make sure you’re not half-dead from sleep chaos.
























Leave a Reply
You must be logged in to post a comment.