Hey there! If you’re taking spironolactone (or thinking about it) you’ve probably heard the word “interaction” tossed around a lot. The short answer? Yes—spironolactone can dance with a whole bunch of other meds, supplements, foods, and even that glass of wine you enjoy on the weekend. The good news is that you don’t have to quit the medication; you just need to know the steps that keep the dance safe and graceful.
Below you’ll find a friendly, down‑to‑earth guide that walks you through the most common spironolactone drug interactions, what to watch for, and simple habits that let you stay in control. Think of it as a chat with a knowledgeable friend who’s got your back.
Quick Overview
| Category | # of Interactions* | Typical Risk | When to Be Extra Careful |
|---|---|---|---|
| Prescription drugs | 382 (Drugs.com) | High potassium, reduced efficacy, toxicity | ACE inhibitors, ARBs, NSAIDs, lithium, digoxin |
| Supplements & vitamins | 7 (Drugs.com) + many OTC | Elevated potassium, altered drug levels | Potassium or magnesium supplements, CoQ10, fish oil |
| Alcohol & food | 1 (Drugs.com) | Increased hyper‑K risk, dizziness | Heavy drinking, salty‑free “potassium‑salt” swaps |
| Disease states | 7 (Drugs.com) | Impaired clearance | Kidney disease, heart failure |
*Numbers are taken from the Drugs.com interaction database (April 2025).
Prescription Pairings
Potassium‑Boosting Meds
Spironolactone is a potassium‑sparing diuretic, which means it already loves saving potassium for you. When you add another “potassium‑saving” medication, the result can be a literal potassium overload—something that can cause heart rhythm problems if it gets high enough.
- ACE inhibitors (e.g., lisinopril, enalapril)
- Angiotensin II receptor blockers (ARBs) (e.g., losartan, valsartan)
- Other potassium‑sparing agents (e.g., triamterene)
- NSAIDs – they can blunt the diuretic effect and raise potassium at the same time.
What should you do? Get a baseline potassium (K⁺) level before you start spironolactone, then repeat the test after one week, again at one month, and any time you change doses. If K⁺ creeps above 5.0 mmol/L, your doctor may lower the spironolactone dose or pause the other potassium‑saver.
Lithium Loops
If you’re on lithium for bipolar disorder, spironolactone can turn up the lithium dial without you even noticing. Why? The drug slows down the kidneys’ ability to clear lithium, making blood levels spike.
Here’s a quick safety recipe:
- Ask your prescriber to check lithium levels every 2–4 weeks after starting spironolactone.
- Look out for classic lithium toxicity signs—tremor, nausea, fatigue, or vague confusion.
- If levels rise, your physician may lower the lithium dose or suggest an alternative mood stabilizer.
Personal note: A friend of mine was on both drugs and felt “spaced out” after a weekend of extra karaoke. A simple blood test caught a lithium level that was too high, and a quick dose tweak saved the day.
Cardiac Meds That Need a Double‑Check
| Drug (Class) | Interaction | Monitoring Tip |
|---|---|---|
| Digoxin | Assay interference → falsely high digoxin levels | Ask for a digoxin‑specific assay if you’re on both. |
| Warfarin | Moderate interaction – possible ↑ INR | Check INR more often when starting or changing spironolactone. |
| Statins (atorvastatin, rosuvastatin) | Moderate – may increase CK if muscle pain appears | Report any unexplained muscle aches; consider CK check. |
In short, keep the dialogue open with your cardiologist or primary care doc. A quick lab tweak can keep everything humming smoothly.
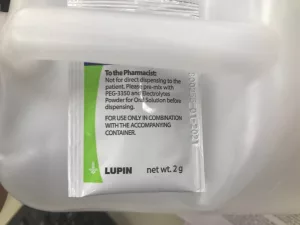
Over‑the‑Counter & Supplement Alerts
Even “natural” products can meddle with spironolactone. Some of the most common culprits are:
- CoQ10 – May affect blood‑pressure response.
- Fish oil (omega‑3) – Moderate interaction; watch for extra bleeding risk if you’re also on aspirin.
- Herbal potassium sources – kelp, dulse, or “seaweed” supplements.
My advice? Before you pop a new supplement, glance at the label for potassium, magnesium, or any “salt substitute” claims. If you’re unsure, a short chat with the pharmacist can clear things up fast.
Supplements & Alcohol
Do I Need to Quit Alcohol?
There’s officially just one alcohol/food interaction listed for spironolactone (again, from Drugs.com). Heavy drinking can raise potassium a bit and make you feel light‑headed, especially if you’re already prone to low blood pressure.
Bottom line: enjoy that glass of wine or beer, but keep it to one standard drink per day. Binge drinking? Best to wait until after you’ve stopped spironolactone for at least 48 hours.
Supplements You Can’t Pair Safely
Below is a quick “no‑go” list for potassium‑rich or potassium‑altering supplements:
| Supplement | Why it’s risky | Safer alternative |
|---|---|---|
| Potassium chloride tablets | Directly adds potassium → hyper‑K | Magnesium glycinate (if you need a mineral) |
| Salt‑free seasonings (often potassium‑based) | Hidden potassium boost | Herb blends without KCl (e.g., garlic powder) |
| High‑dose vitamin D | May increase calcium → affect kidney handling of potassium | Stick to 800–1,000 IU daily unless prescribed higher |
When in doubt, pick a supplement that lists “no added potassium” and remember to tell your doctor about every vitamin, herb, or protein powder you take.
Food & Diet Tips
What Foods Raise Potassium?
Most of us know bananas are potassium‑rich, but there are plenty of sneaky sources that can add up quickly.
| Food | Potassium (mg/serving) | Serving size |
|---|---|---|
| Banana | 420 | 1 medium |
| Orange | 240 | 1 medium |
| Potato (baked, skin) | 610 | 1 medium |
| Tomato sauce | 540 | 1 cup |
| Spinach (cooked) | 540 | 1 cup |
If you love these foods, don’t panic—just be mindful of portion sizes. For most people, staying under 2,500 mg of total potassium per day (including what’s in any supplements) keeps blood levels in the safe zone.
The Salt‑Swap Mistake
Many low‑sodium products replace regular salt with potassium chloride (“K‑salt”). While the idea is great for blood‑pressure control, it can be a nightmare for spironolactone users.
Tip: read the fine print. If the ingredient list mentions “potassium chloride,” reach for a regular herb blend or a sodium‑based seasoning instead.
Balanced Diet Checklist
- Focus on lean proteins, whole grains, and colorful veggies—just watch the portions of the high‑potassium ones.
- Stay hydrated; adequate water helps kidneys excrete excess potassium.
- Keep a light food diary for the first two weeks; you’ll spot patterns like “extra banana after dinner” in no time.
How to Stay Safe
Use an Interaction Checker
There are free tools that let you type in every medication, supplement, and even herbal product you take. I love the Drugs.com Interaction Checker. It flags “major” alerts (52 of them for spironolactone) and gives a short description of what to watch.
Here’s a simple workflow:
- Gather a complete list of everything you’re currently ingesting (prescriptions, OTC, vitamins, herbal teas).
- Enter each item into the checker.
- Note any “major” warnings and discuss them with your prescriber.
- Feel confident that you’ve covered the most risky combos.
When to Pause Spirono‑lactone
In a handful of scenarios you might need to stop the medication temporarily:
- Serum potassium climbs above 5.5 mmol/L (or you develop an arrhythmia).
- Acute kidney injury or a sudden rise in creatinine.
- Pregnancy, if your OB‑GYN advises against it.
- Planning major surgery—do not take it the day of the operation unless your surgeon says otherwise.
If any of these happen, your doctor will likely swap spironolactone for a different diuretic or adjust the dose. Never quit on your own; a brief pause can be lifesaving.
Talking to Your Provider
Good communication is the secret sauce. Here’s a quick script you can copy‑paste into your next appointment note:
“I’m currently on spironolactone 25 mg daily. I also take lisinopril, occasional ibuprofen, a multivitamin, and I enjoy a glass of red wine on weekends. Could we review potential interactions and whether any labs (especially potassium) need a tighter schedule?”
Most clinicians appreciate the specificity—it saves time and gives them a clear picture of your regimen.
Bottom Line
Spironolactone is a fantastic medication for conditions ranging from high blood pressure to stubborn acne, but like any good friend, it has quirks. The biggest ones involve potassium overload, lithium toxicity, and a handful of drugs that can throw your lab numbers out of balance. By staying aware of the major culprits—ACE inhibitors, ARBs, NSAIDs, certain supplements, and those tempting salt‑free seasonings—you can keep the benefits while sidestepping the risks.
Remember these three takeaways:
- Know your potassium budget. Regular blood checks and mindful food choices keep you safe.
- Check every new medication or supplement. A quick interaction checker or a pharmacist call can save a lot of worry.
- Keep an open line with your healthcare team. Simple lab updates and honest conversations are the backbone of safe therapy.
If you’ve ever felt confused about a new prescription or wondered whether that new protein powder was okay, drop a comment below. I’m here to help, and sharing experiences makes the whole community stronger. Stay healthy, stay curious, and enjoy the journey—one mindful step at a time!






















Leave a Reply
You must be logged in to post a comment.