Most people don’t realize that the sympathetic nervous system is buzzing in the background of almost everything you do—whether you’re sprinting up a hill, pulling an all‑night study session, or simply trying to stay calm during a busy day. In a nutshell, it’s the part of your autonomic nervous system that lights the “fight‑or‑flight” fire alarm when danger (or a deadline) shows up.
In this article we’ll break down the anatomy, the fast‑acting “sympathetic response,” why it’s both a superhero and a potential troublemaker, and what you can do to keep it in check. Grab a coffee, sit back, and let’s explore the nervous system that keeps you alive—and sometimes a little on edge.
What Is It?
Definition in Plain English
The sympathetic nervous system (SNS) is a branch of the autonomic nervous system that automatically regulates vital functions without you having to think about them. Think of it as your body’s built‑in emergency response team: when a threat is perceived, the SNS flips a switch that ramps up heart rate, widens airways, releases glucose, and sharpens your senses.
Core Purpose: The “Fight‑or‑Flight” Engine
When you hear a sudden bark or see a speeding car, your brain sends a rapid signal down the spinal cord to the SNS. Within seconds you feel your heart pound, your pupils widen, and you become ready to either “fight” the danger or “flight” from it. This cascade, often called the sympathetic response, is essential for survival and is beautifully coordinated by a handful of neurotransmitters—primarily norepinephrine and epinephrine.
Baseline Role: Everyday Homeostasis
Even when you’re lounging on the couch, the SNS isn’t completely asleep. It maintains a low‑level baseline tone that keeps organs primed and ready. This subtle, continuous activity helps regulate blood pressure, body temperature, and even your metabolism—essentially keeping the engine idling smoothly.
Where Is It?
Thoracolumbar Outflow: The Spinal Birthplace
The SNS originates in the lateral horns of the thoracic (T1–T12) and upper lumbar (L1–L3) segments of the spinal cord—a region doctors call the “thoracolumbar outflow.” From there, short pre‑ganglionic fibers shoot out through the ventral roots and synapse in a chain of sympathetic ganglia that line the spine.
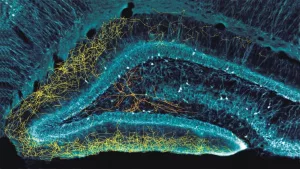
Preganglionic vs. Postganglionic Neurons
Two‑step wiring keeps the signal precise:
- Preganglionic fibers are short, myelinated axons that travel from the spinal cord to a nearby ganglion.
- Postganglionic fibers are longer, unmyelinated nerves that leave the ganglion and head straight to target organs—heart, lungs, eyes, liver, sweat glands, and more.
Major Ganglion Chains & Target Organs
These ganglia form three main trunks: cervical, thoracic, and lumbar. From each trunk, fibers branch out to specific organs. For example, fibers from the upper thoracic ganglia go to the heart, while those from lumbar ganglia influence the kidneys and bladder.
Neurotransmitters That Drive the Response
The SNS mainly uses norepinephrine as its primary post‑ganglionic messenger. The adrenal medulla releases epinephrine (adrenaline) into the bloodstream for a systemic boost. Acetylcholine also appears in the short pre‑ganglionic step.
How It Reacts
Signal Cascade: Brain → Spinal Cord → Body
1. Amygdala spots a threat (real or imagined).
2. It alerts the hypothalamus, which activates descending pathways.
3. Signals travel down the spinal cord to the thoracolumbar outflow, igniting the SNS.
4. Preganglionic neurons release acetylcholine onto ganglia; postganglionic neurons release norepinephrine onto organs.
5. The adrenal medulla dumps epinephrine into the blood for a whole‑body surge.
Physiological Changes in Real Time
Here’s the quick‑fire checklist your body runs through in less than a second:
| System | Change | Why It Helps |
|---|---|---|
| Cardiovascular | Heart rate ↑, cardiac output ↑ | More oxygen‑rich blood reaches muscles fast. |
| Respiratory | Bronchi dilate, breathing rate ↑ | Airflow improves, delivering extra oxygen. |
| Eyes | Pupils dilate | Better vision, especially in low light. |
| Metabolism | Glucose release from liver ↑ | Quick energy for muscles. |
| Digestive | Motility ↓ | Energy is diverted away from non‑essential tasks. |
| Skin | Sweat production ↑, piloerection | Thermoregulation and a “bigger” appearance. |
Short‑Term Benefits
Imagine you’re hiking and spot a rattlesnake. Within a heartbeat you’re sharper, faster, and more alert—thanks to the SNS. This surge can improve reaction time, increase strength, and sharpen focus—perfect for sports, emergencies, or even an intense presentation.
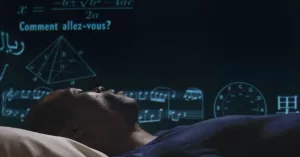
When the Response Sticks: Chronic Stress
If the “alarm” stays on for days, weeks, or months, the system begins to wear out. Persistent elevation of cortisol and catecholamines (epinephrine, norepinephrine) leads to:
- High blood pressure and increased risk of heart disease (Britannica).
- Elevated blood glucose, nudging you toward type‑2 diabetes.
- Digestive woes such as constipation or “butterflies.”
- Sleep disturbances and heightened anxiety.
In other words, the very system that protects you can become a silent saboteur when we let modern stressors hijack it.
Balancing The System
Opposing Forces: Parasympathetic Counterpart
The parasympathetic nervous system (PNS) is the calm‑down crew. While the SNS presses the accelerator, the PNS hits the brakes. Here’s a quick visual comparison:
| Function | Sympathetic (SNS) | Parasympathetic (PNS) |
|---|---|---|
| Heart Rate | Increase | Decrease |
| Pupil Size | Dilate | Constrict |
| Digestive Activity | Inhibit | Stimulate |
| Bronchial Tone | Relax (open) | Constrict |
Why Balance Matters
Both systems work together like a seesaw—too much weight on one side throws you off‑balance. A well‑tuned autonomic nervous system keeps blood pressure steady, supports proper digestion, and helps you transition smoothly from “alert” to “relaxed” states.
Boosting Parasympathetic Tone
Simple habits can nudge the PNS into gear:
- Deep breathing—slow, diaphragmatic breaths activate the vagus nerve.
- Mindful movement—yoga, tai chi, or gentle stretching.
- Consistent sleep schedule—restful nights let the body reset.
- Nature exposure—green spaces reduce sympathetic overdrive (Healthline).
Red Flags: When the SNS Dominates
If you notice any of these lingering, it might be time to talk to a professional:
- Resting heart rate > 100 bpm.
- Persistent anxiety or panic attacks.
- Unexplained high blood pressure.
- Frequent digestive disturbances.
Real Life Uses
Athletic Performance
Elite athletes deliberately tap into their sympathetic drive to boost power output during sprints or weight‑lifting sets. However, they also schedule cool‑down periods to let the parasympathetic system restore balance, preventing over‑training syndromes (sports‑medicine study).
Stress‑Related Disorders
Conditions such as generalized anxiety disorder, panic disorder, and hypertension are closely linked to chronic sympathetic overactivity. Medications like beta‑blockers silence parts of the SNS, easing tremors and rapid heartbeats (Mayo Clinic).
Everyday Stress Management
Even if you’re not an athlete, you can harness the SNS wisely. For a big presentation, a short burst of sympathetic activation (a quick walk, a few jumping jacks) can sharpen focus. Afterward, switch to a calming routine—deep breathing or a brief meditation—to bring the system back to baseline.
How To Track
Heart‑Rate Variability (HRV)
HRV is the gold‑standard metric for autonomic balance. Higher variability usually means a strong parasympathetic tone, while low variability signals sympathetic dominance. Many wearables now give you a daily HRV score; tracking trends over weeks can reveal stress patterns.
Pupil‑Light Reflex Test
In a dim room, shine a flashlight briefly into one eye. A healthy autonomic system produces a quick constriction and dilation. Persistent sluggishness can hint at chronic sympathetic overdrive.
Blood Pressure Monitoring
Regularly checking your resting blood pressure is a simple way to gauge long‑term SNS activity. Consistently elevated numbers (>130/80 mmHg) merit a conversation with your doctor.
When to Seek Professional Help
If any of the following pop up, consider scheduling an appointment:
- Unexplained palpitations.
- Recurring anxiety that disrupts daily life.
- Sudden, severe headaches with visual changes.
- Persistent digestive issues despite diet changes.
Clinicians can run autonomic function tests and tailor interventions—whether lifestyle tweaks or medication.
How To Keep It Friendly
Now that you’ve met the sympathetic nervous system, think of it as a helpful (though sometimes over‑eager) friend. Let’s treat it with respect:
- Give it reason to activate—exercise, challenges, adventure.
- Offer it downtime—sleep, relaxation, laughter.
- Listen to its signals—if your chest feels like a drum, maybe it’s time to breathe.
By honoring both the drive and the calm, you’ll enjoy the energy of the SNS without the burnout.
Takeaway
The sympathetic nervous system is the body’s built‑in alarm clock, primed to protect you, pump you up, and keep you ready for anything. Its anatomy springs from the thoracolumbar spinal cord, travels through a network of ganglia, and releases norepinephrine and epinephrine to fire up heart, lungs, eyes, and more. While that “fight‑or‑flight” burst can be a super‑power in the right moment, chronic activation can sneak in health risks like hypertension, high blood sugar, and anxiety.
Balancing the SNS with its quieter sibling—the parasympathetic nervous system—through breathing, movement, sleep, and nature, is the secret sauce for long‑term wellness. Track your heart‑rate variability, keep an eye on blood pressure, and don’t hesitate to ask a professional for help when red flags appear.
What’s your experience with that nervous‑system buzz? Have you ever felt the “rush” before a big event, and then noticed how hard it was to wind down afterward? Share your story in the comments, ask questions, or tell a friend who might need a friendly reminder that their body is trying to look out for them. We’re all in this nervous‑system adventure together!




















Leave a Reply
You must be logged in to post a comment.