Why This Matters
Let’s just say it up front: getting an Epstein-Barr virus (EBV) diagnosis is… not the club you ever wanted to join. Maybe you feel exhausted all the time for no clear reason (and, no, drinking an extra coffee or walking the dog later isn’t fixing it). Maybe your joints are starting to hurt in new ways, or your bloodwork suddenly looks weird.
There’s this super subtle trap a lot of us fall into: We show up to our rheumatologist appointment a little nervous, maybe blanking out for a second, just nodding along while they do their doctor thing and the really important stuff—stuff about EBV, arthritis risk, immune craziness—kind of floats by. Then we leave, head spinning… still not totally sure what any of it means. (Been there? Same.)
But here’s a secret I wish someone had told me sooner: The right questions to ask rheumatologist after being diagnosed with epstein-barr virus can absolutely change your experience. Seriously. Let’s dig into what really matters—and why you should walk in ready to chat, not just listen.
EBV Isn’t Always “Just a Virus”
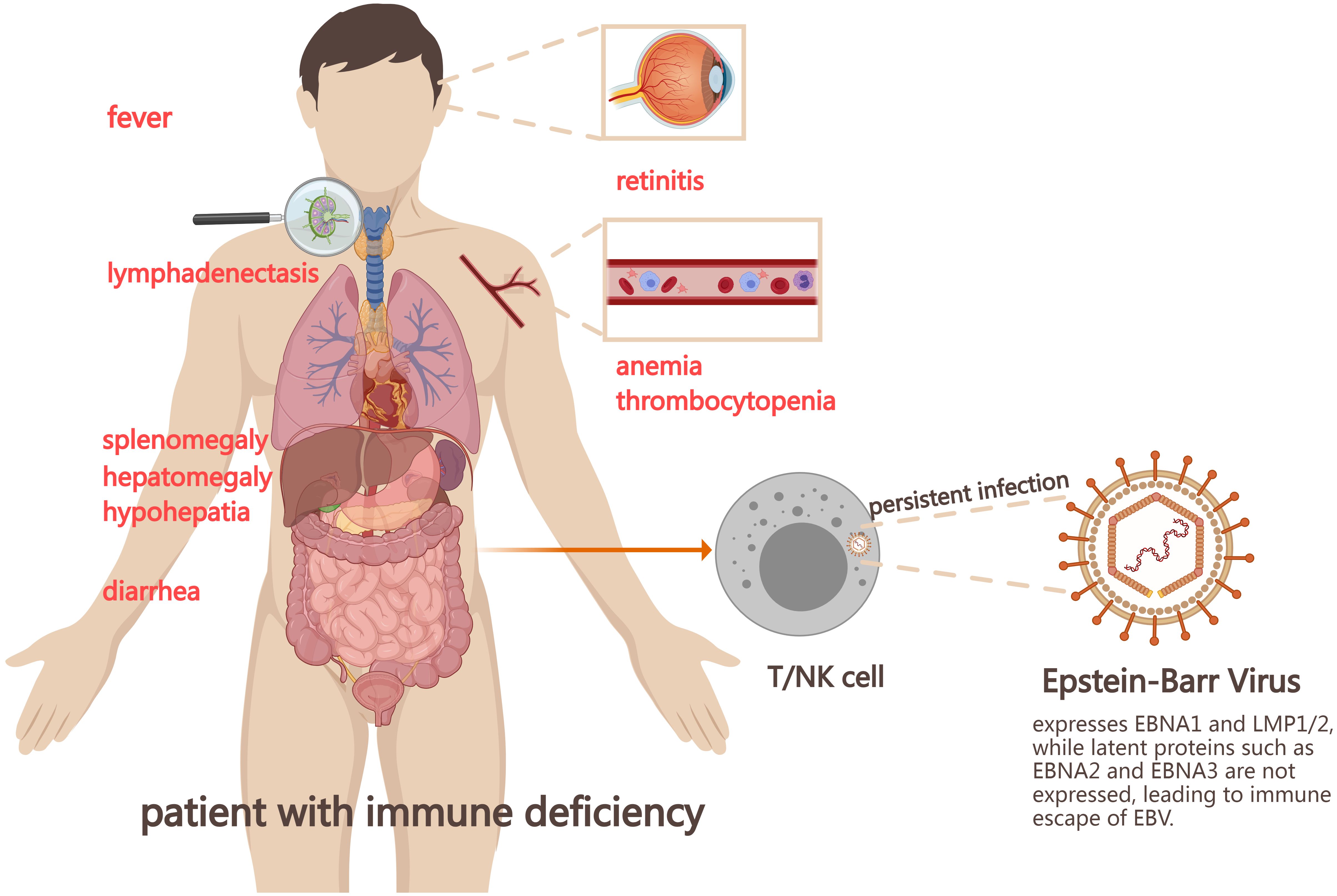
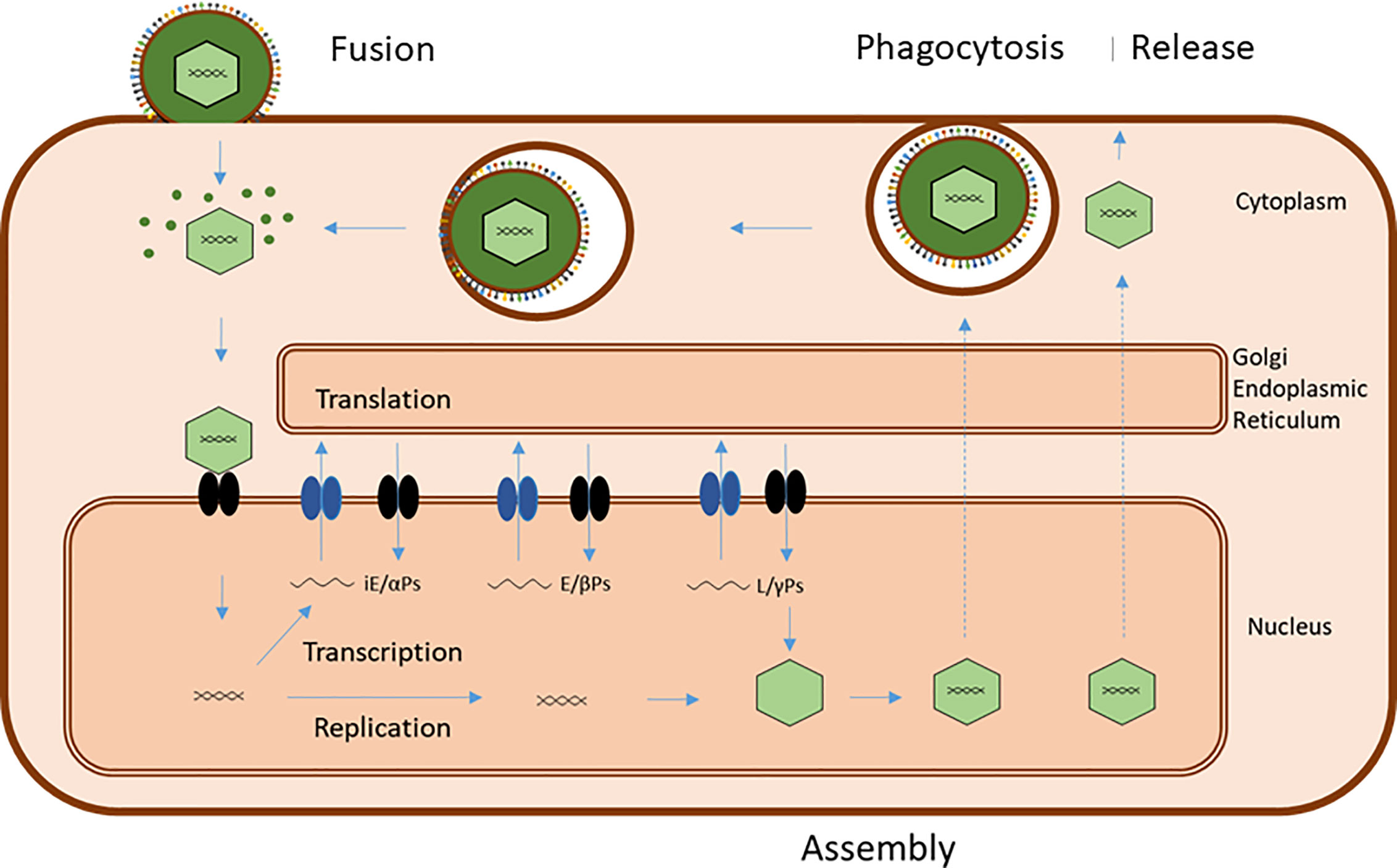
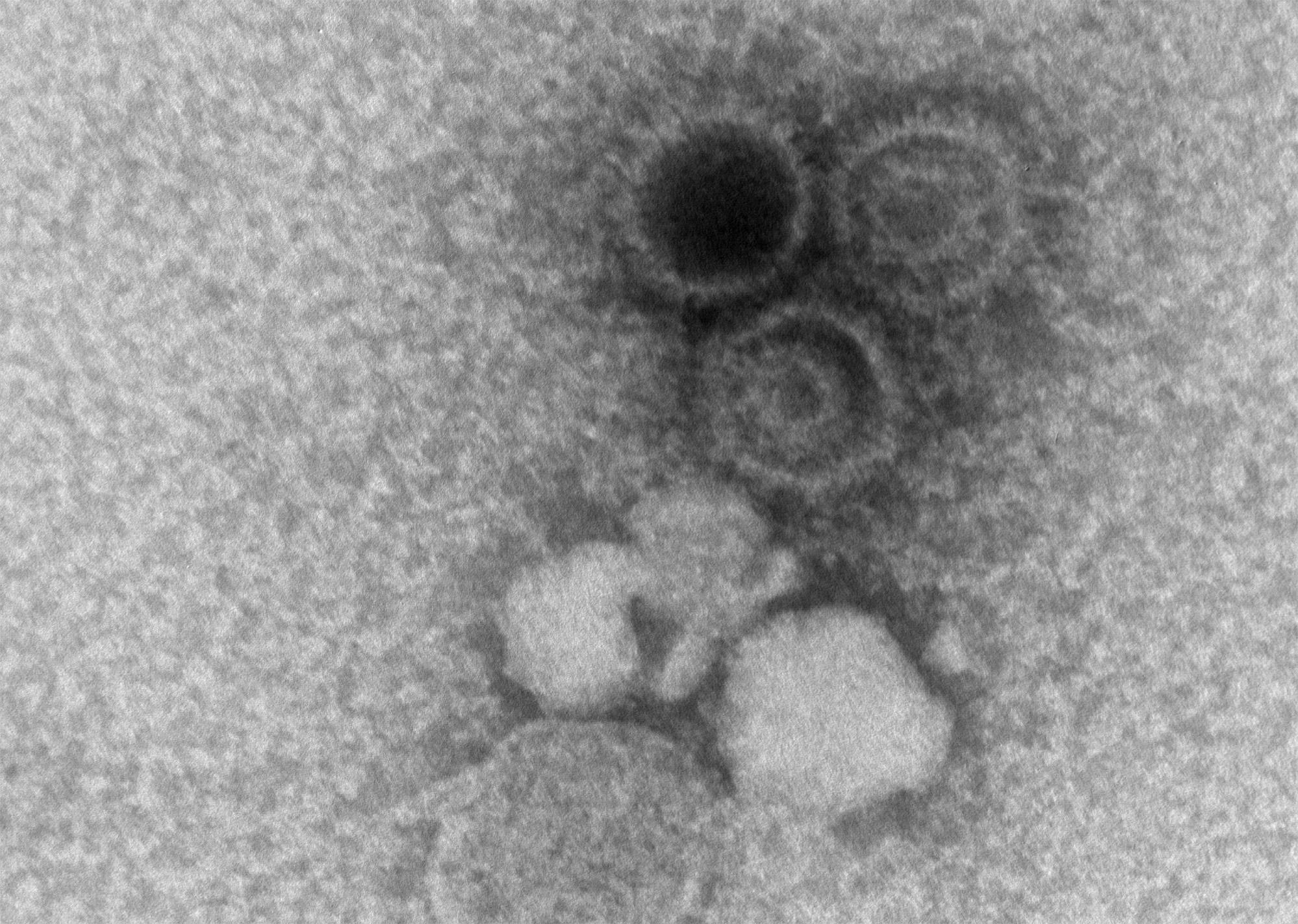
So, rewind: EBV is mostly famous for causing mono (“the kissing disease”… ugh, thanks, high school), but that’s far from its whole story. After the hit-and-run of the first infection, this virus likes to hang out in your body for good. Most of the time? No biggie. But every now and then, for reasons even scientists don’t always get, EBV wakes up again and starts messing with your immune system—all quiet-like at first.
The thing that freaked me out reading the science: According to big studies and rheumatology experts, for some folks, having high EBV antibodies in their blood (even when they don’t feel sick) might mean they’re more likely—not guaranteed,” but “more likely—to develop autoimmune problems down the line.research on lupus and EBV
And we’re not just talking lupus. Researchers have found that reactivation of EBV “could play a role in the pathogenesis of rheumatoid arthritis,” which is a fancy way of saying it might nudge your body towards those stiff, swollen joints Mark across the street keeps complaining about.VA research summary on autoimmune risk
Now’s a good time to pause… have you ever asked your doctor what those antibody results on your chart really mean? Or just assumed “Eh, nothing urgent, or they’d have told me”? It’s okay. Most of us do.
Start With: “What Does My EBV Status Mean For Me… Personally?”
Never be afraid to make it about you. Try this at your next visit: “So, given my high EBV antibodies, how worried should I be about developing something like rheumatoid arthritis? And… are there things I can do now so I don’t end up there?”
A little story here: My friend Jen (nails always perfect, yoga gear always brand new, never used) showed her doctor a test printout with EBV numbers all over. Her doc blinked, said, “Interesting readings, but let’s track it.” Jen almost didn’t ask any more… but she pushed herself: “But what does that actually mean? Should I change anything?” That five-minute back-and-forth led to more tests, a plan, and—get this—a feeling of control she hadn’t had in months.
That’s the crux. EBV might be an old “guest” in your system, but when things start getting weird, don’t let it be a silent one.
Table: EBV vs. Rheumatoid Arthritis Symptoms—Spot the Overlap
| Symptom | EBV Reactivation | Rheumatoid Arthritis |
|---|---|---|
| Fatigue | Sudden, intense, viral-feeling | Persistent, slow-burning, inflammatory |
| Joint Pain | Achy, migratory, sometimes subtle | Stiff, swollen, especially in mornings |
| Fever | Common (esp. during reactivation) | Possible (low-grade, chronic cases) |
| Swelling | Not typical unless severe | Very common, with visible joint changes |
Testing: The Detective Work (And Why It’s Tricky)
Here’s a quirky fact from a rheumatologist’s real-life detective story: sometimes the right diagnosis is like one of those hidden pictures in a puzzle book—you stare and stare, and at first, all you see is noise.told by The Rheumatologist as Detective Doctors run through symptoms, check all your lab results, rule out everything… and it still might take a while.
For EBV, there are lots of different “flavors”—chronic active, chronic reactivated, classic acute—each with their own drama. (Honestly, I wish the virus would pick a vibe and stick with it.) Chronic reactivated EBV means the virus from way back is acting up again, and it’s tough for docs, too, because it’s often less dangerous than “chronic active,” but way more common.according to patient stories on Mayo Clinic Connect
So, next time? Try this: “Can you walk me through my bloodwork? Are these antibodies a sign of chronic reactivated EBV, or just leftover from my past mono? Should we check anything else, or is it just ‘wait and see’ for now?”
And here’s a pro tip: Take notes or ask for a copy. That way you’re in the loop, not just along for the ride.
Diagnostics Deep Dive: What Next?
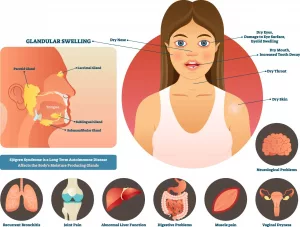
If your doc seems unsure or says “Well, let’s just monitor,” it’s perfectly okay to pause and say, “Can you explain why? Is there a risk I might develop something more serious—like rheumatoid arthritis, or even Sjogren’s?”
By the way, EBV sometimes overlaps with other syndromes (life just loves a combo meal, right?), so dropping the phrase Questions to ask rheumatologist about Sjogren’s syndrome into the conversation can really open things up. Even if you don’t have all the symptoms, showing your doc you’re proactive changes the whole vibe. Trust me.
Table: Typical Follow-Up Tests
| Test | What It Checks | Why It Matters |
|---|---|---|
| EBV IgG/IgM Antibodies | Past infection vs. recent activity | Determining if your virus is firing up again |
| ANA, Rheumatoid Factor | Autoimmunity signals | Checking for early warning signs of lupus, RA, or similar |
| CRP, ESR | General inflammation | Whether your body’s getting fired up, virus or not |
| Salivary gland testing | Dry mouth/eyes evaluation | Early Sjogren’s clues, sometimes linked with EBV |
Treatment Talks: What If EBV Really Is The Culprit?
Alright, let’s be honest… even the “experts” disagree about what to do if EBV shows up in your labs and your joints feel like rusty hinges. The virus itself doesn’t have a magic-bullet cure. Usually, it’s all about rest, letting your immune system chill out, and playing the waiting game.
But here’s a curveball: If EBV causes major issues (like, say, triggering hemophagocytic lymphohistiocytosis—what a mouthful), doctors sometimes reach into their bag for aggressive treatments like anti-CD20 therapies.case report on EBV-induced complications
This doesn’t mean everyone with EBV needs heavy-duty meds—most don’t—but it’s another reason to ask: “If my immune system starts acting out, are there treatments we’d consider to keep things in check? Is there anything I can do now, naturally, that helps tamp down this whole storm?”
Some rheumatologists recommend keeping a close eye… not just on the virus, but on how your whole system’s feeling. Because the boundary between “random EBV symptoms” and “early autoimmune flare” is, honestly, kind of squishy.
Oh, and if you notice dry mouth, dry eyes, or skin issues? Mention it. EBV sometimes overlaps with Questions to ask rheumatologist about Sjogren’s syndrome. The docs appreciate the heads up, and you might get answers sooner.
What About Lifestyle, Nutrition… Anything Else I Can Do?
If you’re anything like me, you hear “just rest and hydrate” and want to throw a pillow at the advice. Sure, it helps… but what else?
So, here’s what’s working for some people (again, not medical advice…but real stories matter):
- Gentle movement, like yoga or long walks, keeps stiffness from taking over. One friend swears her little five-minute yoga stretches changed her flare days entirely (she used to think yoga was just fancy stretching… she was right, but also, it works).
- Tracking symptoms—energy, pain, mood—in a journal. You don’t realize how much better (or worse) things are until you look back and spot trends. When I did this with my own health blips, I actually caught a pattern my doc had missed. Turns out, some bad days really were linked with stress… or cheese (sad, but true).
- Asking about anti-inflammatory diets, sleep, and supplements. A good doc will talk to you about what’s “woo” and what’s evidence-based. Don’t be shy.
Bonus: If you’re tracking symptoms and some days it feels suspiciously like Sjogren’s (dry mouth, gritty eyes), check out Questions to ask rheumatologist about Sjogren’s syndrome for tips on what to ask. Getting a head start never hurts.
Who’s On Your Team (And Why That Matters)
So here’s a plot twist you might not expect. Sometimes it’s not just your rheumatologist who should be in the loop. EBV, autoimmunity, fatigue—they can blur the lines between different specialties.
If your case is tricky (maybe your immune system just won’t behave), it’s 100% fair to ask, “Should we rope in an infectious disease specialist, too? Or maybe another expert if my symptoms get complicated?” Sometimes having an extra set of eyes—somebody who geeks out over viral mysteries—can catch what others might miss.EBV research on systemic autoimmune disease
If all this has you feeling overwhelmed, by the way, know you’re not alone. People on patient forums often say they feel less “crazy” just by asking pointed questions—knowing what to ask keeps you from feeling lost in the weeds. (And, sometimes, just hearing your rheumatologist say, “That’s a great question!” is oddly healing. It means you’re on the right track.)
Keep Resources—and Company—Close
Quick tip: Bookmark patient advocacy groups, or even questions to ask rheumatologist after being diagnosed with epstein-barr virus for checklists and more articles like this. Sometimes you just need to see that someone else out there, in the wild, has wondered the same things.
The whole “what’s wrong with me?” loop can feel endless—especially if you’re new to the world of unpredictable symptoms, vague lab results, and doctor lingo. Don’t hesitate to bring in family or friends for support, or ask your care team for mental health resources. You’re allowed.
So… Now What? (Your Game Plan!)
Look, I get it—this is all a lot. Just because you have EBV (or even high antibody levels), it doesn’t mean you’re doomed for arthritis, exhaustion, or immune drama forever. But it does mean you get to be proactive—super proactive, if you want.
Let’s recap (for those of us with brain fog right now):
- Getting clear on your EBV antibody status—and what that means for arthritis risk—is crucial. Don’t leave the office until it makes sense.
- Ask brave, detailed questions. Use the phrase questions to ask rheumatologist after being diagnosed with epstein-barr virus as your secret power move. It shows you’re prepared, and lets your doc dig deeper with you.
- If you spot dry mouth, gritty eyes, or odd symptoms, mention Questions to ask rheumatologist about Sjogren’s syndrome. It puts the whole picture together faster.
- Keep a notebook—or your phone—handy for test results, questions, weird happenings, anything. Small details matter.
- Remember: You deserve to be heard, to get answers, and to feel like a partner in your own care. Don’t settle for less.
The big thing? Honestly, just showing up and being curious already sets you apart. That’s how you turn this weird, stressful moment into a chance to take charge of your health story. We’re rooting for you. Now… go scribble that question list in your notebook.
And if you stumble upon advice, stories, or wins about EBV and autoimmune mix-ups? Share them. Chances are, you’ll help someone else who’s just as confused as you were last week. Isn’t that what this is all about?




















Leave a Reply
You must be logged in to post a comment.