If you or someone you love has lupus, the very first thing you’ll want is a doctor who really gets it. A lupus doctor isn’t just any physician – it’s a specialist who knows how to read the body’s cryptic warning signs, balance powerful medicines, and keep you feeling like yourself again. Below you’ll discover who those doctors are, how to tell if they’re the real deal, what to expect at your first visit, and practical steps to pick the perfect partner for your health journey.
Who Treats Lupus?
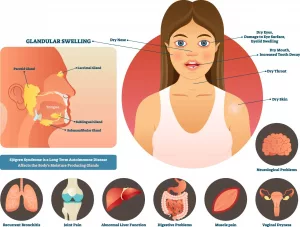
Lupus is a master of disguise. One day it’s aching joints, the next it’s a rash on your cheek, and later it might be a silent kidney flare. Because of that, you’ll often need a team of providers, all working together like a well‑rehearsed band.
What does a rheumatologist do for lupus patients?
A rheumatologist is the captain of the lupus‑care ship. They specialize in autoimmune diseases, run the lab tests that confirm lupus, write the long‑term medication plans, and watch for flares. Most people refer to them simply as “the lupus doctor.”
Which other specialists handle organ‑specific complications?
- Nephrologist – monitors kidneys, especially if you develop lupus nephritis.
- Dermatologist – treats the classic butterfly rash and other skin manifestations.
- Ob‑GYN / Maternal‑Fetal Medicine – guides pregnancy planning, because lupus can affect both mom and baby.
- Cardiologist – watches for heart inflammation and blood‑clot risks.
When do you need a dermatologist, nephrologist, or OB‑GYN?
Think of it like a road trip. The rheumatologist plots the route; if you hit a bump (kidney pain) you pull over to see the nephrologist. If a rash appears, the dermatologist steps in. When you’re ready to start a family, the OB‑GYN becomes your co‑pilot. All of these specialists are part of the broader lupus care network.
Multidisciplinary Lupus Centers – Real‑World Examples
Many top hospitals house dedicated Lupus Centers where these experts sit under one roof. For instance, Hospital for Special Surgery’s Lupus & APS Center of Excellence, led by Dr. Kyriakos A. Kirou, MD, offers rheumatology, nephrology, and pregnancy counseling all in one place. Such centers make coordination smoother and reduce the “passing the baton” frustration many patients feel.
Spot Qualified Doctors
Not every doctor who calls themselves a “rheumatologist” has the depth of experience needed for complex lupus cases. Here’s how to separate the truly qualified from the merely qualified.
What board certifications should a lupus doctor have?
Look for board certification in rheumatology (American Board of Internal Medicine). Extra certifications in nephrology, dermatology, or maternal‑fetal medicine are a plus when you have organ‑specific involvement.
How many clinical trials or publications indicate expertise?
Doctors who regularly publish in peer‑reviewed journals or lead clinical trials stay on the cutting edge of lupus treatment. Dr. Jill P. Buyon, MD at NYU Langone, for example, has led dozens of pregnancy‑focused lupus studies and is widely cited in the field.
Are awards such as “Top Doctor” or “Castle Connolly” meaningful?
Yes, but treat them as a supporting data point. Awards show peer recognition, yet the real proof lies in patient outcomes and the doctor’s communication style.
Red‑Flag vs. Green‑Flag Credentials
| Red‑Flag (Proceed with Caution) | Green‑Flag (Confidence Builder) |
|---|---|
| Missing board certification in rheumatology | Board‑certified rheumatologist (ABIM) |
| Limited experience with lupus (≤ 5 years) | ≥ 10 years treating lupus patients |
| No affiliation with a Lupus Center or academic program | Affiliated with a university‑run Lupus Clinic (e.g., Yale Lupus Program) |
| Only general internal‑medicine practice | Published lupus research or clinical‑trial leadership |
Real‑World Example: Dr. Anca Askanase
Dr. Anca Askanase, MD, is listed on ColumbiaDoctors as a board‑certified rheumatologist who accepts new patients and offers virtual visits. Her profile includes Castle Connolly Top Doctor badges and Super Doctors recognition, making her a solid candidate for anyone seeking a lupus specialist in New York.
First Lupus Appointment
Walking into a new doctor’s office can feel like stepping onto a stage you’ve never rehearsed for. Knowing what to expect can calm those nerves.
What tests will the doctor order on day 1?
- Complete blood count (CBC) – checks for anemia or low white cells.
- Comprehensive metabolic panel – looks at kidney and liver function.
- Antinuclear antibody (ANA) panel – the classic lupus screen.
- Urinalysis – early sign of kidney involvement.
- Complement levels (C3, C4) – often dip during flares.
How long will the initial consult last?
Usually 45–60 minutes. That might feel long, but a thorough history (symptom diary, medication list, family history) is essential for accurate diagnosis.
What information should you bring?
- List of every medication and supplement you take.
- Recent lab reports (if you’ve been tested elsewhere).
- A simple symptom log – dates, triggers, severity.
- Insurance card and a photo ID.
Patient Perspective
Maria, a 28‑year‑old teacher, shared: “I was terrified the first time I sat down with my rheumatologist. I brought a notebook with three pages of symptom notes. The doctor smiled, thanked me for the detail, and we built a treatment plan together in that hour. It felt like teamwork, not a lecture.”
Lupus Treatment Options
Now that you’ve met the right doctor, the next step is understanding the medicines they might suggest. Lupus treatment is a balancing act: we aim for disease control while minimizing side‑effects.
Which FDA‑approved drugs are first‑line vs. second‑line?
First‑line agents typically include hydroxychloroquine (Plaquenil) and low‑dose steroids for acute flares. If those aren’t enough, doctors move to immunosuppressants like azathioprine, mycophenolate, or methotrexate. Biologics such as belimumab (Benlysta) are reserved for patients who need a stronger push.
When do doctors recommend biologics or clinical‑trial enrollment?
Biologics become an option when conventional drugs fail to keep disease activity low after 6–12 months, or when organ damage (e.g., kidneys) is progressing. Many top centers, like the Yale Lupus Program led by Dr. Fotios Koumpouras, MD, regularly enroll patients in trials for newer agents, giving you early access to cutting‑edge therapy.
How do specialists balance benefits vs. risks?
Every medication carries a risk profile. Steroids, for instance, tame inflammation quickly but can cause weight gain, bone loss, and mood swings. Biologics may increase infection risk. Your doctor should discuss monitoring plans (regular blood work, bone density scans) and lifestyle tweaks (diet, exercise) to offset those risks.
Lupus Medication Overview
| Medication Class | Typical Indication | Major Risk | Prescribed By |
|---|---|---|---|
| Antimalarial (Hydroxychloroquine) | Baseline disease control, skin rash, joint pain | Retinal toxicity (rare, requires yearly eye exam) | Rheumatologist |
| Low‑dose Corticosteroid | Acute flare, organ involvement | Weight gain, osteoporosis, mood changes | Rheumatologist |
| Immunosuppressant (Mycophenolate) | Lupus nephritis, severe skin disease | Infection, GI upset, liver enzyme elevation | Rheumatologist or Nephrologist |
| Biologic (Belimumab) | Persistent activity despite other meds | Injection site reactions, infection risk | Rheumatologist (often in specialty center) |
Expert Insight
According to Dr. Donald Thomas, MD, author of The Lupus Encyclopedia, “Shared decision‑making is the cornerstone of modern lupus care. When patients understand why a drug is chosen and how it will be monitored, adherence improves dramatically.”
Choosing Your Doctor
Now that you know who to look for and what they do, let’s turn that knowledge into action. Picking a lupus doctor is a personal decision, and a systematic approach can make it feel less overwhelming.
How to verify if a doctor is part of a Lupus Center of Excellence?
Visit the hospital’s website and look for a dedicated “Lupus Clinic” or “Lupus Center of Excellence.” These programs often list their leadership team, research activities, and patient‑education resources. Verify that the physician you’re considering is named in that team.
What insurance or tele‑health options should you prioritize?
Many top rheumatology practices now offer virtual follow‑ups for stable patients. Check whether your insurer covers tele‑medicine visits and whether the doctor’s office accepts your plan. For example, ColumbiaDoctors’ Dr. Askanase provides both in‑person and virtual appointments, making access easier for busy patients.
When is traveling for a high‑volume lupus specialist worth it?
If you have complex organ involvement (e.g., lupus nephritis) or need enrollment in a clinical trial, a specialist who sees hundreds of lupus patients a year may offer more nuanced care. A patient in rural Texas chose to travel to Dr. Kirou’s Lupus Nephritis Program because of the center’s advanced kidney‑protective protocols, and she reported a dramatic reduction in flare frequency.
Step‑by‑Step Checklist
- Ask your primary‑care doctor for a referral to a board‑certified rheumatologist.
- Search the doctor’s name on the hospital’s Lupus Center page.
- Confirm board certification, years of lupus experience, and any published research.
- Check insurance acceptance and tele‑health availability.
- Read patient reviews (look for mentions of communication style and empathy).
- Schedule a 60‑minute introductory visit and bring your symptom log.
- After the visit, assess how comfortable you felt; trust your gut.
Putting It All Together
Finding the right lupus doctors is a journey, not a one‑time task. You’ll likely meet several specialists before you land on the team that feels like a perfect fit. Remember these core ideas:
- Teamwork matters. A rheumatologist leads, but nephrologists, dermatologists, and OB‑GYNs may join the crew.
- Credentials count. Look for board certification, research leadership, and recognitions like “Top Doctor.”
- First visit preparation. Bring a symptom diary, medication list, and your questions – the more you share, the better the plan.
- Treatment is personalized. Your doctor will weigh benefits and risks, and may suggest clinical‑trial participation for cutting‑edge options.
- Practical logistics. Insurance, tele‑health, and travel considerations can shape your final choice.
Most importantly, choose a doctor who listens, explains things in plain language, and treats you as a partner rather than a case number. When you feel heard, adherence improves, flares lessen, and life regains its rhythm.
What’s your experience with lupus specialists? Have you found a doctor who truly makes a difference? Share your story in the comments below – your insight could guide someone else on the same path. And if you have any lingering questions, don’t hesitate to ask – we’re all in this together.






















Leave a Reply
You must be logged in to post a comment.