Symptoms Sneak Up on You?
Let’s be honest for a second… who actually expects dry eyes and achy joints to signal something more serious? I sure didn’t, and neither did my friend Mia, who dismissed her gritty eyes as “just allergy season” every spring. Flash forward a couple years—fatigue that wouldn’t quit, random mouth sores, and suddenly, her rheumatologist drops a new word on her: Sjögren’s syndrome.
If you’re reading this, you might be stuck in that foggy place too, wondering: Am I overthinking this, or is my body genuinely waving a red flag? Let’s chat about those all-too-real questions you should ask at your rheumatologist appointment. Not a lecture—just the stuff that cuts through confusion and helps you own your next steps.
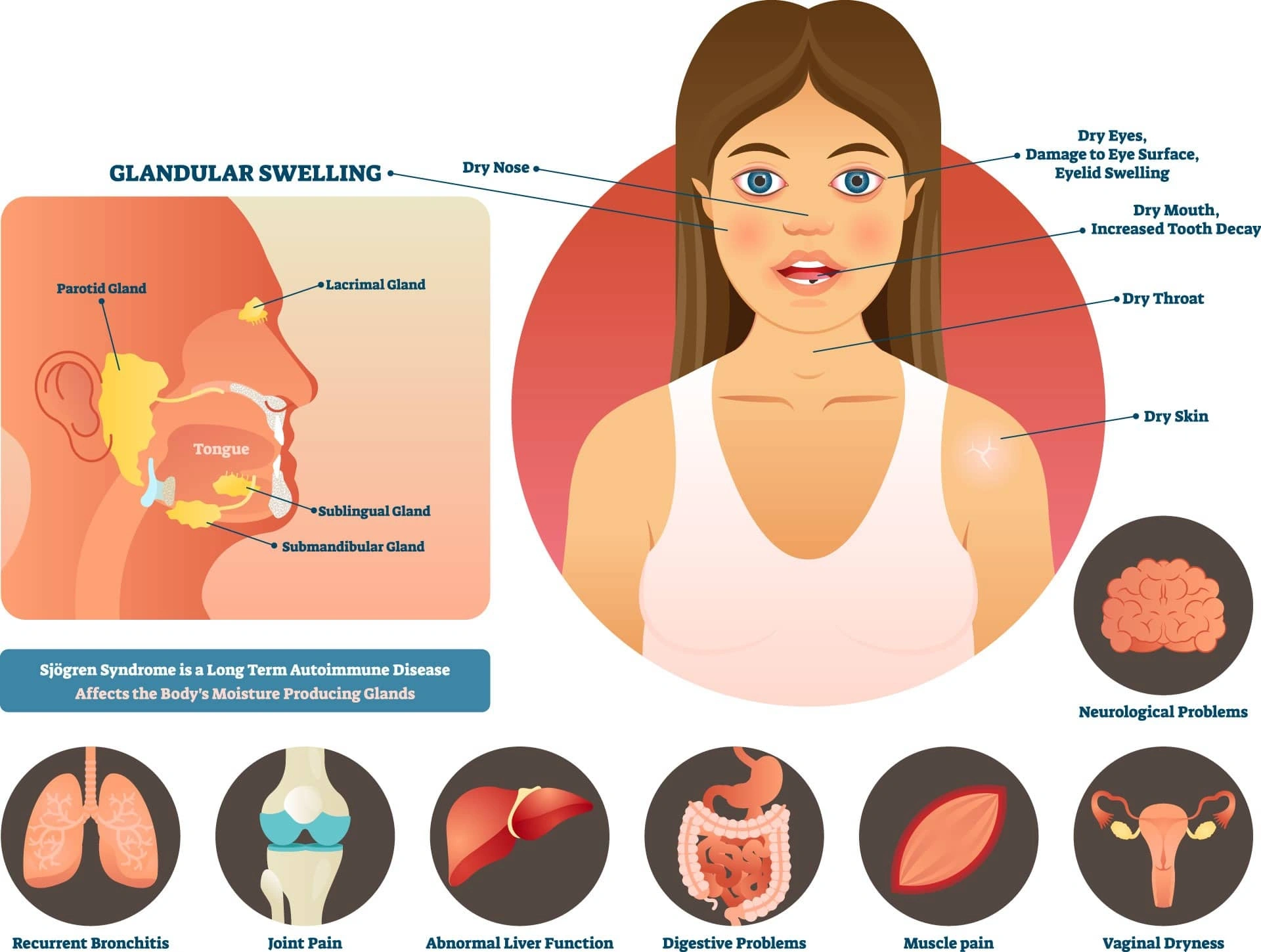
What’s Really Happening in My Body?
“Does This Sound Like Sjögren’s to You?”
It’s practically impossible to figure this out on your own because the early symptoms—dry eyes, dry mouth, crushing fatigue, maybe some joint pain—are, well, annoyingly common in life. Menopause, hay fever, an old antihistamine you forgot you were taking… they all cause similar things.
So at your next visit, try leading off with something blunt: “Doc, do my symptoms fit what’s typical for Sjögren’s?” This gives your rheumatologist an opening to explain what she’s seeing and thinking, not just what she isn’t saying. Bonus: it can calm those late-night “what if” Google spirals. (Trust me, we’ve all been there.)
Add a personal layer:
When Mia finally mentioned to her doctor how she had to stop wearing contacts because her eyes were so dry, things started to click. Her doctor explained that in classic Sjögren’s, these symptoms just keep stacking—like a really bad Jenga game you never asked to play.
“What Tests Pin Down the Diagnosis?”
This one’s a must. Diagnosing Sjögren’s isn’t one-and-done—it’s like solving a slow-moving mystery. There’s no single “yes or no” test, but, as outlined by the Sjögren’s Foundation, your doctor will run a combo of the following:
| Test Type | What It Checks | Why It Matters |
|---|---|---|
| Blood Tests | Antibodies (SSA/Ro and SSB/La), inflammation, organ function | Catches 60–80% of cases; rules out mimics like lupus or rheumatoid arthritis |
| Eye Tests | Schirmer test, dye tests for eye surface | Measures dryness, finds damage you might not notice yet |
| Salivary Tests | Saliva measurements, scans (sialogram or scintigraphy) | Checks how your glands are really working, not just how they feel |
| Biopsy | Small sample from lip gland | Gold standard when diagnosis is uncertain |
Tip: Jot down anything that stands out to you before your appointment. If you want a jump-start on gathering your thoughts, try the Do I have Sjögren’s syndrome quiz. You might spot patterns you’d missed.
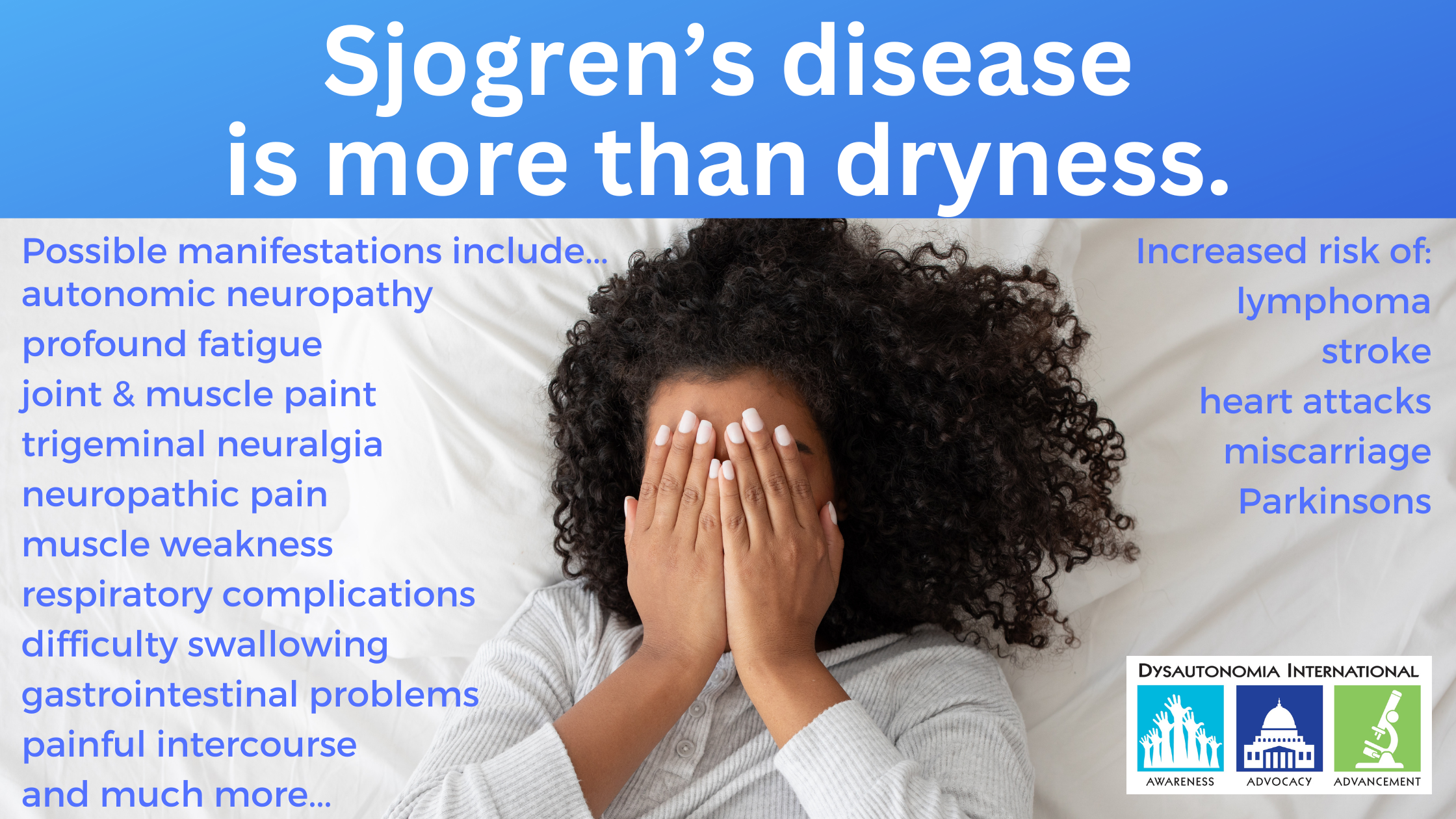
Should I Worry About More Than Dryness?
“Is This Only Glands, or Can It Go Beyond?”
Here’s the big one nobody talks about when you first hear about Sjögren’s: it’s not just about parched eyes or a mouth that feels like the Sahara. This thing can quietly mess with your lungs, kidneys, nerves… even your liver or thyroid. That’s called “extraglandular involvement,” and your doc should be checking for hints of it, even if you don’t feel anything weird yet.
Questions that nudge the conversation forward:
- “Any signs this is affecting my organs, not just my mouth or eyes?”
- “Should we do imaging or bloodwork now, or wait for new symptoms?”
Quick anecdote:
I’ll never forget the story of Sam—his only sign was random bouts of coughing, which he chalked up to seasonal allergies for months. Turns out, it was early lung involvement. Getting proactive checks made a world of difference. Catching these things early is key.
“Should I Be Screened for Lymphoma?”
It’s a scary thought, but in reality, people with Sjögren’s have a higher risk of a certain type of lymphoma—8 to 15% over 10-20 years, according to research on what your rheumatologist should be monitoring for. Early on, this might look like swollen glands, weird fevers, or longtime fatigue that feels just a notch different.
Go into appointments ready to ask:
- “Am I at higher risk for lymphoma? What are the warning signs?”
- “How often do you check for changes that might hint at this?”
Your doctor might suggest a simple serum protein blood test every six months—sounds boring, but seriously, that $30 test can catch things before they get complicated.
Could It Be Another Autoimmune Too?
“Is There Overlap With Other Conditions?”
Sjögren’s loves company. I know, rude! It doesn’t always show up by itself—up to half of folks diagnosed also have another autoimmune illness like lupus, rheumatoid arthritis, or thyroid disease. Suddenly that “grab bag” of symptoms makes sense.
Sometimes symptoms overlap so much that your doctor needs to be a detective. Asking the right questions clears things up:
- “Could my pain/skin changes/thyroid issues be another autoimmune condition too?”
- “Would extra tests help us tell what’s Sjögren’s and what’s something else?”
Personal note:
My cousin Sarah got her diagnosis after months of bouncing between doctors thinking she just had “quirky allergies” and unexplained fatigue. She finally got clear answers when her rheumatologist looked at the whole puzzle, not just one symptom at a time. If this sounds familiar, don’t be shy—ask about the bigger picture.
If you’re wondering how to talk through these overlaps, the questions to ask rheumatologist about autoimmune disease article has plenty more talking points.
What’s the Game Plan for My Symptoms?
“How Do We Treat The Tough Stuff?”
Newsflash: There’s no official cure for Sjögren’s yet. (I know. I wish I had better news.) But that doesn’t mean you have to just suffer. Treatments are all about reducing symptoms, preventing damage, and improving quality of life. And they are as individual as you are.
Ask your doctor to walk you through options:
- “What meds are best for my symptoms, and how do we decide when to try something new?”
- “Are there side effects I should watch out for?”
- “How do we balance meds for multiple symptoms or conditions without making dryness worse?”
Add everyday examples:
My mom switches between three kinds of eye drops and finally found one that didn’t make her vision blurry for hours. Her secret sauce? Explaining her exact routine to her doc so they could tweak it. The answer is rarely one-size-fits-all.
| Symptom | Common Fixes | Questions to Ask |
|---|---|---|
| Dry Eyes/Dry Mouth | Artificial tears, prescription drops, saliva stimulants | “What if OTC products aren’t enough?” |
| Joint Pain/Fatigue | Hydroxychloroquine, checking for overlap syndromes | “Could this be linked to another condition?” |
| Systemic Issues | Immunosuppressants, steroids (rare), specialist referral | “How do we monitor major organs over time?” |
Don’t forget: some medications (for blood pressure, allergies, or depression) can worsen dryness. Always tell your doctor everything you’re taking—even that innocent-looking sleep aid or allergy pill.
If you’re feeling unsure about autoimmune symptoms in general, the questions to ask rheumatologist about autoimmune disease guide is super handy for prepping before your next visit.
How Should I Monitor Myself Between Visits?
“How Often Do We Check In?”
After that first big conversation… what comes next? Regular monitoring matters, especially since Sjögren’s has a reputation for being “sneaky.” You’ll want to ask:
- “How often should we do bloodwork or office visits?”
- “What should I watch for on my own?”
- “Should I get checkups with specialists like eye doctors or dentists too?”
Your doctor might recommend a schedule that ebbs and flows depending on how stable your symptoms are (think every 3–6 months at first). Write down what matters most to you—there’s no “dumb” question here.
Reflection time:
I started journaling little things at night—like when eating felt weird or my eyes got redder than usual after a long day. Turns out, showing those notes to my doctor helped catch a tiny thyroid issue before it spiraled. Being your own “body detective” is surprisingly powerful!
Want a gut check on dryness? The Do I have Sjögren’s syndrome quiz is a seriously easy way to track changes and spark better appointment convos.
Let’s Wrap This Up: You, Your Questions, and Your Health
Whew… that was a lot, wasn’t it? If you’ve stuck with me this long, you already get that managing Sjögren’s syndrome isn’t about memorizing medical trivia—it’s about knowing the right questions to ask your rheumatologist about Sjögren’s syndrome, sharing everything (even the weirdest symptoms), and teaming up for care that feels personal.
Your appointment isn’t just “checklist medicine”—think of it as a two-way street: you bring your real life, your doctor brings their toolbox. Even if a question feels silly, or you need to pause, laugh, or share one of those “no one gets it but me” stories… do it. It’s your health.
If you need a cheat sheet or want to prep for overlaps, grab inspiration from the questions to ask rheumatologist about autoimmune disease. Feeling nervous or overwhelmed? You can anchor yourself with the Do I have Sjögren’s syndrome quiz—it’s quick and gives you language for your next conversation.
Bottom line: You’re not just “one more Sjögren’s patient.” You’re you. So ask, laugh, cry, vent, and keep moving forward. What’s one question you want answered at your next visit? Seriously—write it down right now. You’ve got this. I’m rooting for you.



















Leave a Reply
You must be logged in to post a comment.