Most people don’t realize that protecting yourself from HIV doesn’t have to mean taking a daily pill or even monthly injections anymore. There’s a new option—lenacapavir, given just twice a year, that’s showing up to 99.9% effectiveness in clinical studies. It’s a big deal, and the World Health Organization (WHO) just added it to their official prevention guidelines. But here’s the real question: why does this matter to you, and what should you know before asking your care provider about it? Let’s break it down.
P.S. If you’re thinking, “Whoa, $28,000/year in the U.S. even?” Yeah, that number’s hitting hard. UNAIDS says generic versions could cost as low as $25 per person annually. So, let’s talk about real-world access, not just the headlines.
The Science Behind Lenacapavir
You might be wondering, “Is this seriously the next big thing?” That’s exactly what Dr. Carlos del Rio, an infectious disease expert from Emory University, said when the FDA approved Yeztugo (lenacapavir) last June after 20 years of research. The breakthrough? This injection isn’t just a once-a-year sprinkle of hope—it’s a two-dose protection shield, every six months. No more monthly appointments. No more peeling open pill bottles like you’re on a vitamin routine. Just two moments and you’re set for another six months.
How effective is it? In the PHASE 3 PURPOSE trials, 99.9% of people who got lenacapavir stayed HIV-negative. 99.9! That’s not just “meh—better than nothing.” This is the equivalent of training wheels with a 99.9% guarantee against tumbles. And for folks in under-resourced communities—like the 36% of Americans who didn’t get PrEP in 2022 due to treatment gaps or stigma? This could reshape the game.
Who’s It For And Why Now?
When HIV Prevention Feels Out of Reach
Look, here’s the real messy truth: HIV prevention hasn’t grown evenly. In parts of the US South, Black and Latino communities, and LGBTQ+ circles, access keeps falling behind. You ever tried finding a clinic in a rural town during peak farm season? Good luck getting time off.
So WHO’s recommendation isn’t just medical policy. It’s a call to action. As they put it during the 2025 AIDS Conference, “We have the tools to end the AIDS epidemic. What’s missing is bold implementation rooted in equity.” For high-risk folks—sex workers, gay and bisexual men, transgender people—the issue isn’t always the virus itself but battling scores of other roadblocks to prevention. Lengthy insurance forms, clinic visits, fear of judgment…the list goes on.
It’s Not Just for the US
In many parts of sub-Saharan Africa, where over 60% of global new HIV cases land, pills and frequent follow-ups feel like a luxury. Yeah, condoms and regular testing still matter. But when you’re a young woman living where clinics are 30 miles away and your nearest pharmacy barely stocks malaria meds? Injectable lenacapavir feels like a lifeline. That’s why WHO and Gilead cut a deal to supply two million doses for free to low-income countries at cost (so, zero profit margins), kickstarting global equity talks. Not charity. Just frank logistical help.
How Does This Compare to Other Prevention Tools?
Before you say, “Wait—a shot? But I thought daily pills were the norm,” let’s compare. Lenacapavir joins a growing prevention toolbox, but it’s not just another option. It’s a pathway to more personalized protection. Think of it as this: – Oral PrEP (like Truvada) = training yourself to remember a daily routine. – Apretude (bi-monthly shot) = clinic loyalty, maximum six cocktails a year. – Lenacapavir = only two investment pieces. That’s it.
| Method | Dosage | Efficacy | Price (U.S. private insurance) |
| Lenacapavir (Yeztugo™) | 2x per year injection | 99.9% | $28,218/yr (but under negotiation in global agreement) |
| Oral PrEP (Truvada/Descovy) | Daily | ~99% (if perfect adherence) | $2,500/yr (with co-pay programs) |
| Apretude (CAB-LA) | 1 starter injection monthly, then every 2 months | ~90% in studies | $27,000/yr in private coverage |
*Still confused? Here’s the deal: Daily pills work, but life’s messy. Two shots a year? Feels more like vaccines, or birth control jabs. Free, reliable—but only if you actually can get to the clinic. Let’s not sweep that part under the rug.
HIV Treatment Options: Prevention or Cure?
You’re probably thinking, “So what if I already got HIV?” Yep. This blog’s not magic—it doesn’t cure infections. That’s what current HIV treatments like ART (antiretroviral therapy) are for. The benefit of all this prevention buzz? It opens doors for treatment advancements. If more people avoid facing HIV risks, we lower global infection pressure—and treatment access improves over time. In some areas, ART access went from 43% in 2015 to 88% in 2024. No guarantees, but reducing new cases pushes us toward better community care for people already positive.
The Kinks in the Armor
Side Effects and Hidden Costs
Okay, let’s get real here. If you’ve ever taken HIV meds, you know: no drug works like magic without trade-offs. The main side effects of lenacapavir follow the rule of any injection—the discomfort at the jab site, or bumps and rashes. Most subsides within a few days. The emotional piece? Doctors are required to screen you for depression, as linked CAB-based PrEP injections showed a few red flags—nothing definitive yet, but they’re studying it closely.
But cost? That’s the elephant in the clinic. Gilead says biotech manufacturing isn’t cheap, and you can’t just “make ten thousand doses tomorrow.” Fair point. Still, UNAIDS did the math and says generic versions set free could slash access costs by 99%. That’s less about fairness and more about urgency. If you’ve ever priced out insurance deductibles in the U.S. before, you’re nodding right now. “$28,218 a year? Pass.”
Real-World Implementation Isn’t a Switch
Okay, let’s get practical. WHO just endorsed lenacapavir, but real life isn’t clinical trial smooth. Let’s say you live in Georgia. Yep, the US state—not the country. Clinics may say, “We don’t carry that FDA option yet.” Gilead’s only recently shipped to pharmacies. In many countries? It’ll take years for approvals and generic rollout. And for folks from lower-income brackets, even free access through the Global Fund isn’t a guaranteed pipeline. “We’ve seen health inequities before,” said Dr. Meg Doherty recently on UN news. “What we need now is bold action empowered by communities, not just governments.”
Dosing, Shots, and Sticking to the Plan
So… What Do 2 Shots a Year Actually Look Like?
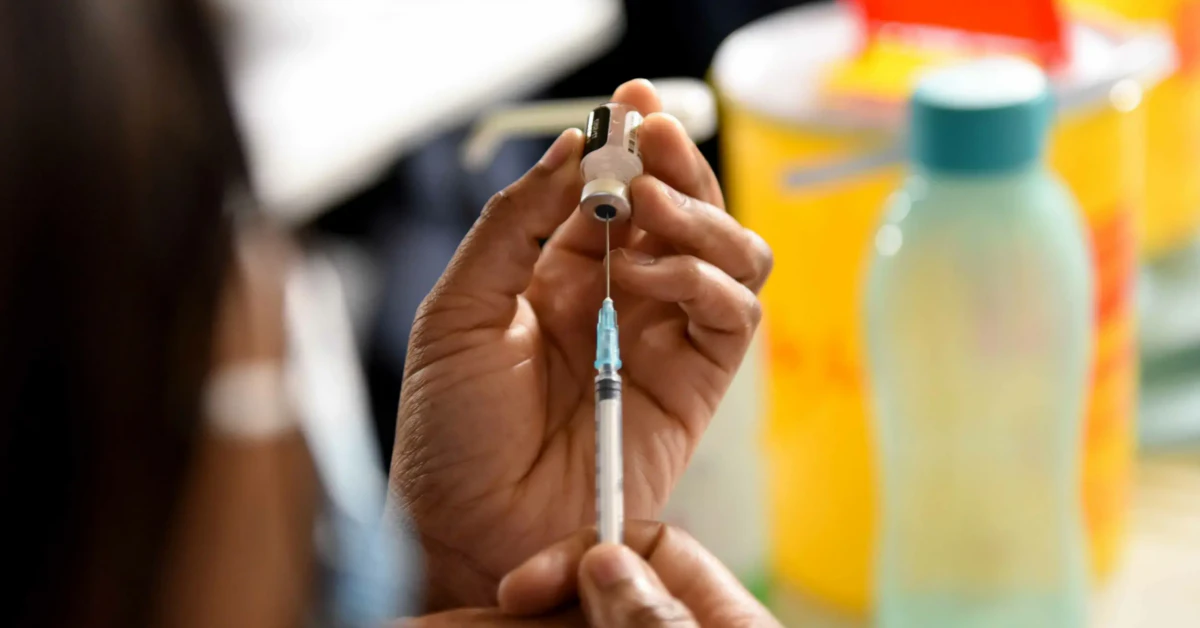
You walk into the doctor’s office twice. The nurse draws your blood for an HIV test before the injection (important—remember, you can’t start if already positive). Then, a quick jab in the arm or leg. Not in the back, not timed with yoga breaths. It’s not dramatic.
Sticking to this? Here’s the mental leap: 99.9% efficacy with high adherence. If someone skips a shot, protections fade—like skipping your birth control shot and getting pregnant on accident. But here’s the upside: skipping once doesn’t scream “You’re at risk now.” Under lenacapavir, your timelines stay safe for weeks after the due date. Unlike Truvada, where even three skipped days show drops in shielding, lenacapavir makes a few mistakes less deadly. That’s a relief for busy people or parents working double shifts—no guilt for occasional slip-ups.
Prioritizing High-Risk Groups
If you’re looking at this and thinking, “Should I start it or wait for cheaper generics?” Keep watching. Gilead’s commitment to high-risk communities is where this shines. Studies showed transgender women had 72% + higher odds of forgetting to redose under daily medication compared to injections. But the core issue remains: the 2025 cost in some countries remains $28,218 per person annually.
UNAIDS isn’t sugarcoating it. Winnie Byanyima, their Director, flat-out said, “It’s beyond comprehension how Gilead can price it like this.” It’s not just ethics—it’s equity. If a injection holds the potential to stop 1.3 million new cases yearly but costs like a Tesla, chains will crack in accessibility. But here’s the pro tip: push for Global Fund advocacy. It worked for cabotegravir—why not lenacapavir?
Final Thoughts: How ‘HIV prevention injection’ Changes the Fight
This might be the first time you’re seeing it on maps, but here’s what health departments and clinics nationwide are thinking: “We now have options.” That’s huge. For years, the HIV prevention debate was like comparing Dial-Up internet to LTE. You had oral pills and vaginal rings, both useful—but not inclusive. Now injectable lenacapavir bridges the gap for folks who want less frequent clinic interactions and can’t load up on daily routines.
But here’s the thing—this isn’t just numbers on a chart. It’s also about stories. Carlos del Rio gave an interview earlier this year where he shared therapy insights from Atlanta: “I asked one local transgender patient—’Why do you prefer this?’ She said, ‘I don’t want to explain to my roommate why I’m taking medicine again, even when they don’t.’ That’s grounding, real stuff.”
All this to say: 2025’s biggest public health catalyst isn’t just medicine moving—it’s people-first progress. It’s balancing the heady numbers with the emotional, messy, and lived experiences. It’s getting PrEP into the arms—not the wallets—of those who want it.
If you’re >= 35 kg (77 lbs), at risk, and looking at this twice-a-year shot, reach out to your provider. For folks outside the U.S., Gilead’s working with WHO to roll out guidelines that balance equity, affordability, and availability. So, take this with you: questions are normal. Doubts are human. But in 2025, prevention is getting as flexible as life itself.























Leave a Reply
You must be logged in to post a comment.