Hey there, friend. If you’ve ever wondered why getting a simple check‑up feels like a cross‑country road trip for many folks living outside the city, you’re in the right place. Rural healthcare access is a real, lived‑in challenge – one that touches everything from cancer survivorship to everyday family doctor visits. In the next few minutes, I’m going to walk you through what “access” really means, why it’s tougher out here, who feels it most, and, most importantly, what’s actually working to change the story.
Understanding Rural Access
How do experts define “access” in a rural context?
According to the National Academies of Sciences, “access” is the timely use of personal health services to achieve the best possible health outcomes. In plain English, it’s not just about having a clinic somewhere on the map; it’s about being able to get there when you need to, without jumping through endless hoops. The Rural Health Information Hub expands that definition, adding that access also hinges on financial means, transportation, health‑literacy, and the confidence that the care you receive is high‑quality.
Core numbers that paint the picture
| Metric | Rural | Urban | Source |
|---|---|---|---|
| Physicians per 100 k people | 68 | 80 | Rural Health Info Hub |
| Average distance to nearest hospital | 10.5 mi (≈ 17 min) | 5.6 mi (≈ 12 min) | Wellbeings.org |
| Percentage of population living rurally | 20 % | — | NIHCM infographic |
Who’s most affected?
While everyone in a remote county feels the pinch, a few groups feel it harder than others:
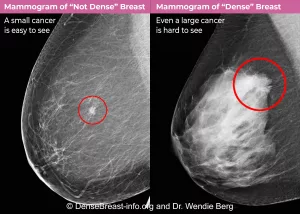
- Cancer survivors – they need regular imaging, labs, and counseling after treatment. Follow‑up gaps can mean missed recurrences.
- Older adults with chronic illness – juggling meds, specialist visits, and limited mobility.
- Low‑income families – often uninsured or underinsured and lacking reliable transport.
For a deeper dive into survivorship challenges, check out our piece on cancer survivors care. It’s full of practical tips you can share with loved ones.
Major Access Barriers
Workforce shortages
Only about 10 % of family physicians practice in rural areas, according to a recent NIHCM infographic. That shortage means longer wait times, fewer same‑day appointments, and sometimes no provider at all. Dr. Carrie Cochran‑McClain, Chief Policy Officer at the National Rural Health Association, emphasizes that “without a sustainable pipeline of providers, rural health will continue to lag.”
Transportation & distance
Imagine needing to drive 30 minutes on a winding backroad just to see a dentist. That’s a daily reality for many. The average rural resident travels 10.5 miles to the nearest hospital – a distance that balloons for specialty care. When public transit is scarce, a single broken car can mean missing vital treatment.
Insurance & financial hurdles
Rural communities have higher uninsurance rates. Medicaid remains a lifeline, especially after the 2024 ASPE report highlighted its critical role in keeping rural families covered. Yet, gaps persist: some plans don’t accept certain providers, and out‑of‑pocket costs still deter many from seeking care.
Health‑literacy & cultural barriers
Limited English proficiency, low health‑literacy scores, and deep‑rooted mistrust can make navigating the health system feel like decoding a foreign language. Community health workers (CHWs) often bridge this gap, translating medical jargon into everyday conversation.
Technology & broadband gaps
Tele‑health is a game‑changer, but only 58 % of rural households have reliable high‑speed internet (FCC, 2023). Without a stable connection, video visits turn into pixelated frustrations, leaving patients stuck with the old “drive‑the‑mile” model.
Impact on Specific Groups
Rural cancer survivors & follow‑up care
After curative treatment, survivors need routine scans and counseling. Yet, many travel over an hour for each appointment, leading to delayed detection of recurrence. Our guide on rural cancer care outlines how mobile oncology units and tele‑oncology are shrinking those distances.
Elderly patients with multiple chronic conditions
Picture Mrs. Jenkins, 78, managing diabetes, arthritis, and hypertension. Coordinating her primary doctor, a cardiologist, and a pharmacy means juggling appointments across three different towns. Missing one visit can trigger a cascade of complications.
Rural youth mental health
Isolation, limited school‑based counselors, and stigma combine into a perfect storm. Suicide rates in many rural counties outpace national averages, underscoring the urgency for mental‑health first‑aid programs and tele‑therapy.
Effective Access Solutions
Tele‑health expansion
HRSA data shows a 45 % jump in rural tele‑health visits in 2023 alone. When patients can pop into a virtual office from their kitchen, missed appointments drop by nearly a third. The key is pairing broadband grants with user‑friendly platforms.
Mobile clinics & community health workers
Mobile units—think vans equipped with X‑ray machines—bring specialty care right to town squares. In Montana, a mobile oncology program slashed travel distance for patients by 70 %. Meanwhile, CHWs conduct home visits, check meds, and translate discharge instructions, improving medication adherence by up to 25 %.
Medical student initiatives
Students aren’t just learning; they’re serving. In Appalachia, a group of medical students runs weekly vaccination clinics, health‑education workshops, and even helps local farms set up on‑site wellness checks. Curious about the details? Dive into our article on medical student initiatives.
Policy & funding levers
Medicaid expansion, American Rescue Plan (ARP) grants, and HRSA’s Rural Health Clinic (RHC) designation have poured billions into underserved areas. These funds support everything from tele‑health infrastructure to loan‑repayment programs that entice providers to set up practice in small towns.
Transportation assistance programs
Ride‑share partnerships, like Lyft Rural Ride, subsidize trips to appointments for low‑income riders. Some states also offer voucher programs that cover fuel costs for patients traveling over 30 miles.
Example: Follow‑up Care Solutions
Our follow‑up care solutions guide demonstrates how coordinated scheduling apps, automated reminder texts, and community health navigator “check‑ins” keep patients on track after discharge—especially vital for cancer survivors and chronic‑illness patients.
Practical Action Steps
Step‑by‑step checklist for patients
- Confirm your insurance status (Medicaid, Marketplace, or employer plan).
- Register on your health system’s patient portal for tele‑health appointments.
- Use the HRSA Rural Health Clinic locator to find the nearest provider.
- Explore transportation vouchers through your county health department.
- Ask your provider about community health workers or patient navigators.
Free resources & toolkits
Many states publish “Rural Health Navigator” apps that map clinics, tele‑health options, and even roadside assistance. The Telehealth Resource Center (HRSA) offers free guides on setting up a secure video visit—even on a simple tablet.
When to call 911 vs. schedule a tele‑visit
If you’re experiencing chest pain, severe shortness of breath, or uncontrolled bleeding, dial 911. For non‑urgent concerns—like a mild rash, medication refill, or a follow‑up question—start a tele‑visit. A quick decision‑tree graphic (feel free to sketch it on paper) can help you decide in a heartbeat.
Future Measurement Outlook
Key performance indicators (KPIs) to watch
| KPI | Target for 2026 |
|---|---|
| Rural primary‑care physicians per 100 k | 75 |
| Average travel time to nearest hospital | ≤ 8 mi |
| Tele‑health utilization among rural adults | ≥ 40 % |
Emerging research & technology
Artificial‑intelligence triage bots are being piloted in low‑bandwidth settings, offering symptom checks via text. Wearable remote‑monitoring devices—think cheap pulse‑oxometers—are already helping rural heart‑failure patients catch warning signs before a hospital visit becomes inevitable.
Conclusion
Rural healthcare access isn’t just a statistic; it’s the story of families who drive hours for a check‑up, survivors who fear missing a follow‑up scan, and young doctors who dream of making a difference far from big‑city hospitals. The numbers—68 physicians per 100 k, 10.5 miles to the nearest hospital, and high uninsurance rates—show the challenge, but they also point to where we can intervene.
By supporting workforce pipelines, expanding tele‑health, leveraging mobile clinics, and empowering community health workers, we can turn those miles into minutes and those gaps into bridges. Use the checklist above, share the resources with a neighbor, and if you’re a provider, consider a short‑term stint in a rural clinic—it could be the most rewarding chapter of your career.
We’re all in this together. If you’ve faced any of these hurdles or found a clever work‑around, I’d love to hear your story. Let’s keep the conversation going and keep building healthier, more connected rural communities.




















Leave a Reply
You must be logged in to post a comment.