Imagine sitting across from your oncologist, hearing the word “response” and wondering exactly what it means for you. Will the treatment shrink the tumor? Will it spare you from extra surgeries? Will it keep side‑effects manageable? The good news is that doctors have a toolbox full of ways to gauge how well chemotherapy is working, and science is getting better at forecasting the outcome before the first dose even lands. In this friendly, down‑to‑earth guide we’ll walk through why chemotherapy response matters, how it’s measured, what factors sway it, and what you can do if the early signs aren’t looking promising. Grab a cup of tea, relax, and let’s demystify the journey together.
Why It Matters
When we talk about chemotherapy response, we’re not just tossing around a clinical term – we’re talking about a compass that points toward survival, quality of life, and the next steps in your treatment plan. A strong response can mean a higher chance of cure, fewer surgeries, and a smoother road ahead. Conversely, a weak response may signal the need for a change in drugs, an addition of targeted therapy, or even a clinical‑trial option.
Balancing benefits and risks is at the heart of every oncology decision. The more precisely we can predict response, the better we can match a potent regimen with a patient’s unique health picture, sparing them unnecessary toxicity while maximizing the chance of success.
Measuring Response
Oncologists rely on several tried‑and‑true methods to determine whether the chemotherapy is doing its job. Below is a quick snapshot of the most common tools.
| Measure | When Used | What It Tells You | Key Study |
|---|---|---|---|
| RECIST / WHO Imaging | After 2–3 cycles (≈6–9 weeks) | Percentage change in tumor size | The Response to Neoadjuvant Chemotherapy |
| Pathologic Complete Response (pCR) | Post‑surgery (neoadjuvant setting) | No residual invasive cancer cells; predicts excellent survival | Li et al., 2019 |
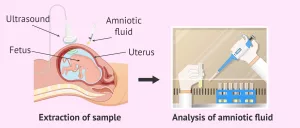
| Molecular Assays (CIN signatures, ctDNA) | Baseline or early‑treatment biopsy | Genomic clues that forecast sensitivity or resistance | CRUK Cambridge, 2023 |
| Ultrasound Spectrum Analysis | Pre‑clinical & early‑phase studies | Distinguishes responders from non‑responders using RF signal patterns | Li et al., 2019 |
Imaging Criteria (RECIST & WHO)
These are the workhorses of oncology. After a few cycles of chemo, a CT or MRI scan is taken, and the radiologist measures the longest tumor diameters. A 30 % shrinkage usually qualifies as a “partial response,” while a 20 % increase indicates progression. Imaging is quick, widely available, and gives a visual cue that both you and your doctor can see together.
Pathologic Complete Response (pCR)
If you’ve had chemotherapy before surgery (the so‑called neoadjuvant approach), the pathologist will examine the removed tissue under a microscope. When no invasive cancer cells are found, that’s a pCR – and studies show five‑year survival rates can soar up to 100 % in certain breast‑cancer subtypes.source
Chemo‑Response Assay Tests
Back in 2011, Lee et al. published a study where they cultured a patient’s tumor cells and exposed them to the same drugs planned for therapy. The assay correctly predicted who would benefit from anthracycline‑ and taxane‑based regimens in over 70 % of cases.source Though not yet routine everywhere, such functional tests are gaining traction as a personalized way to gauge response.
Emerging Precision Biomarkers
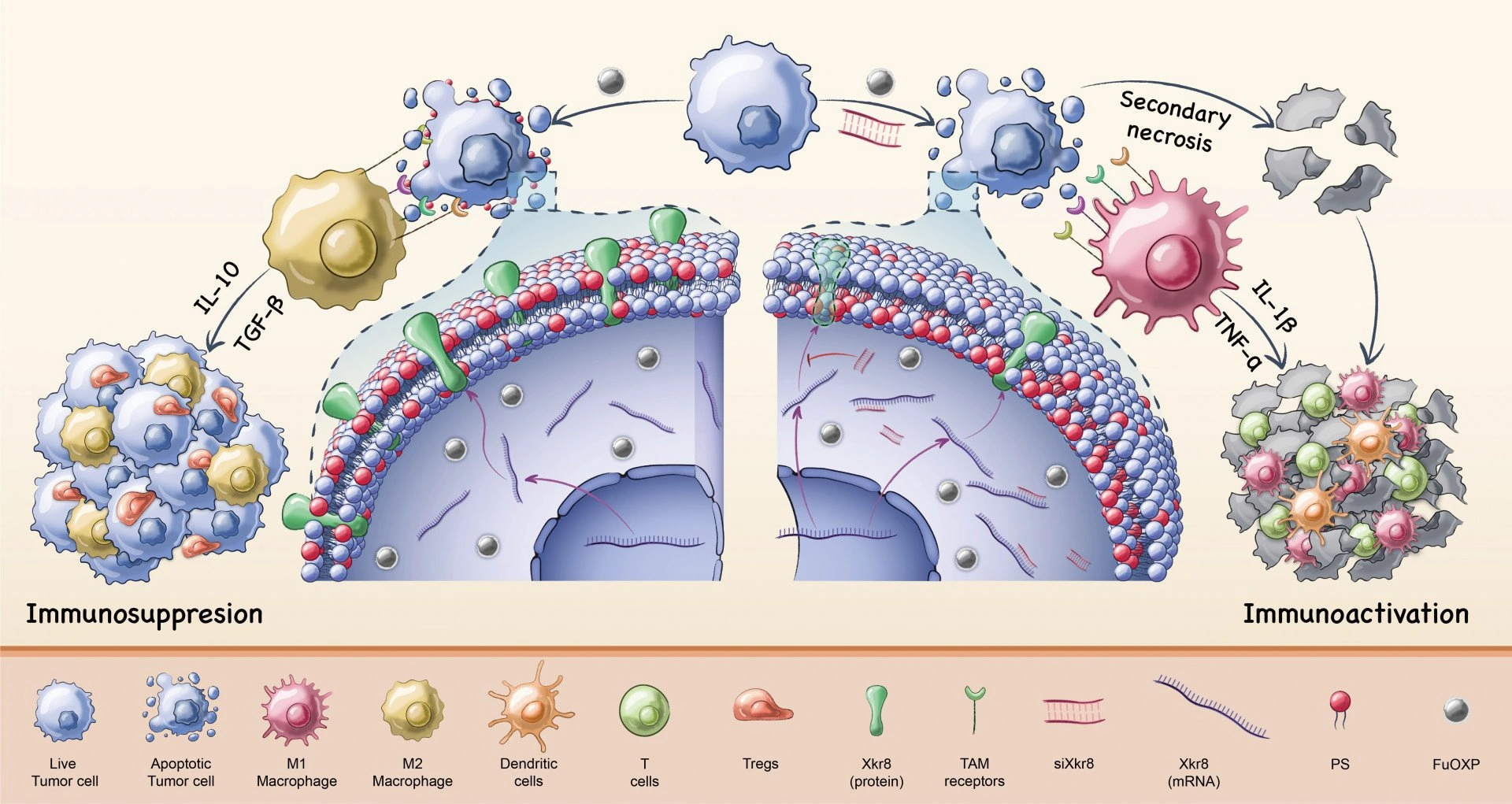
Scientists at the Cancer Research UK Cambridge Institute recently unveiled chromosomal‑instability (CIN) signatures that can be read from a single genomic test. These signatures predict sensitivity to platins, taxanes, and anthracyclines with impressive accuracy, hinting at a future where a simple blood draw could tell you whether a drug will work.source
Real‑World Factors
Even the best‑crafted test can’t capture everything. Real‑life biology, patient health, and treatment logistics all sway chemotherapy response.
Tumor Biology
Hormone‑receptor status (ER/PR), HER2 amplification, and genetic mutations each paint a different picture. For example, ER‑negative/HER2‑negative (triple‑negative) cancers often respond dramatically to taxane‑based regimens, while ER‑positive/HER2‑negative tumors may be more modest responders.
Patient‑Specific Variables
Age, kidney or liver function, and overall fitness influence how much chemo you can tolerate. A frail, elderly patient may need a reduced dose or a single‑agent regimen, which could affect the odds of a robust response.
Treatment‑Related Variables
Drug dose intensity, scheduling, and whether the drugs are given together or sequentially can tip the scales. Sometimes a slight tweak—like adding a biologic agent—makes a non‑responder into a responder.
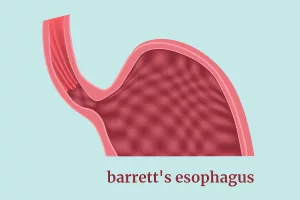
Neoadjuvant Chemotherapy Resistance
In some cancers, especially neoadjuvant chemotherapy resistance, the tumor simply refuses to shrink. This can happen in esophageal adenocarcinoma, where dense fibrosis and poor drug penetration blunt the effect of standard regimens. When resistance shows up early, clinicians often pivot to a different drug class or enroll the patient in a trial.
Precision Oncology Platform
Imagine a dashboard where your tumor’s DNA, RNA, and protein data are fed into an algorithm that suggests the most likely effective drugs. That’s the promise of a precision oncology platform. By aligning therapy with the tumor’s molecular quirks, the platform improves the odds of a favorable response while sparing you from unnecessary toxicity.
Predicting Before Treatment
Wouldn’t it be wonderful to know weeks—or even months—before starting chemo whether it will work? That’s the holy grail of oncology, and we’re getting closer.
Biomarker‑Driven Prediction
Chromosomal‑instability signatures, circulating tumor DNA (ctDNA) levels, and gene‑expression panels can flag likely responders. For instance, a high CIN score in a breast‑cancer biopsy often predicts sensitivity to taxanes.source
Artificial‑Intelligence Models
Machine‑learning systems now blend imaging features with genomic data to output a “response probability” score. Early pilots have shown AUC values above 0.80, meaning the model can correctly differentiate responders from non‑responders 80 % of the time.
Clinical Decision‑Support Tools
When a physician opens the precision oncology platform, the system may suggest adding a PARP inhibitor for a BRCA‑mutated ovarian tumor, because data show that such tumors are especially chemosensitive when paired with that drug. This kind of real‑time guidance is reshaping how we think about “one size fits all” chemotherapy.
Limitations & False Positives
Predictive tools are not crystal balls. Tumor heterogeneity, sampling bias, and evolving resistance mechanisms can lead to mis‑classification. That’s why doctors always pair a prediction with close monitoring—imaging after a few cycles, blood tests, and symptom checks—to confirm reality.
If Response Is Poor
Finding out early that the tumor isn’t shrinking can feel like a punch to the gut. But it’s also an opportunity to pivot, re‑evaluate, and keep moving forward.
Re‑Assess the Regimen
Switching to a different class—say, from an anthracycline to a taxane—or adding a targeted agent (like trastuzumab for HER2‑positive disease) can revive the fight. Clinical trials often explore combinations that are not yet standard, so ask your oncologist about eligibility.
Discuss Surgical Options
Even a modest response can downstage a tumor enough to make breast‑conserving surgery possible, or to avoid an extensive esophagectomy in esophageal adenocarcinoma. A multidisciplinary tumor board will weigh the imaging, pathology, and patient preferences to chart the next move.
Supportive Care & Quality of Life
When chemo isn’t delivering, the focus may shift toward symptom control, nutrition, and mental‑health support. Staying hydrated, maintaining a protein‑rich diet, and leaning on friends and caregivers can make a huge difference in stamina and outlook.
When “Watch‑and‑Wait” Makes Sense
For some indolent tumors or in patients with limited life expectancy, aggressive chemotherapy may do more harm than good. In such cases, clinicians might recommend observation, palliative radiation, or simply comfort‑focused care. The decision is deeply personal and should align with your values.
Takeaway Summary
Understanding chemotherapy response is like having a GPS for your cancer journey. It tells you when you’re on the right road, when to take a detour, and when a new route might be better altogether. Here are the three big take‑aways:
- Response matters. A strong response often predicts better survival and can spare you from extra surgery.
- We can measure it in many ways. From classic scans to cutting‑edge genomic signatures, doctors have a growing toolbox to assess and predict response.
- Don’t lose hope if the early signs aren’t great. There are numerous strategies—new drugs, clinical trials, surgery tweaks, and supportive care—that can still lead to a positive outcome.
Next time you sit down with your oncology team, ask about the specific methods they use to monitor response, whether a precision‑oncology platform is part of your care, and what the plan looks like if the cancer isn’t behaving as expected. Knowledge empowers you, and together you can navigate the twists and turns of treatment with confidence.
Curious about how these concepts play out in real‑world cases? Explore more on cancer treatment outcomes or dive deeper into esophageal adenocarcinoma treatment. Remember, you’re not alone on this road—your medical team, friends, and a growing body of science are all here to help you reach the best possible destination.


















Leave a Reply
You must be logged in to post a comment.