Ever had that day-2 crash after stopping something cold turkey? Like quitting coffee or skipping your gym routine? Antidepressant withdrawal is real—and for some folks, it sticks around longer than you’d expect. Feelings of anxiety, electric shock sensations, nerve pain—you’ll read about those in a moment. The bottom line? If you’re thinking about stopping your meds, don’t do it alone. Talk to your doc, our experts agree. Because yeah, some surprises are better left unpacked.
Here’s the deal: Stopping antidepressants isn’t as simple as swapping your morning latte for herbal tea. Around 31% of patients report symptoms like dizziness, nausea, or brain zaps (yes, that’s a thing) after quitting, according to a Lancet study. And for people like Phillipa Munari—she stopped Effexor and landed in bed for two years dealing with severe nerve pain—the journey’s got nothing to do with the quick fixes you see on TikTok. Let’s break this down, no fluff. Just the stuff that matters.
What Are the Most Common Symptoms?
Plan on quitting Paxil or Lexapro? Please don’t do it blind. Short-term withdrawal symptoms usually show up in the first 1–4 days and last 1–2 weeks. But sometimes? They stick around longer than your ex’s hoodie in your closet. The Cleveland Clinic calls this antidepressant discontinuation syndrome, and it’s most common with medications like:
- Paroxetine (Paxil)
- Escitalopram (Lexapro)
- Venlafaxine (Effexor)
Even if you’re tapering slowly, don’t be shocked if your body fights back. That’s why we’re explaining the micro-details—so you’re not caught off guard.
How Soon Do Symptoms Appear?
Ever had a hangover the morning after? Think of withdrawal symptoms as your brain’s hangover from meds. They typically show up within 48–72 hours after your last dose. And here’s the twist: even placebos cause some similar effects, per the Mayo Clinic. But when you stop antidepressants?
The Cleveland Clinic shared data that’s hard to ignore. Of people who stopped their meds:
- 7% still felt symptoms at 2 months
- 6% at 1 year
- 2% longer than 3 years
Here’s the catch: If you’ve been on high-dose meds for years, your risk climbs. Think about it like your skin adjusting to a harsh facial—your body can do the same after antidepressants.
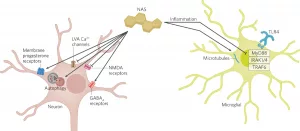
Flu-Like Symptoms: Your Immune System Isn’t Even Involved
You’re not catching a cold. That nausea, muscle aches, and feverish feeling? Purely your nerves rebelling. Our bodies get used to serotonin levels being artificially balanced. Cut the meds out and the system works overtime to find its new normal. The Cleveland Clinic calls this anticholinergic rebound, where your body’s dehydration and lost appetite set you up for fatigue you can’t blame on your sleep quality.
Here’s the kicker: 40% of return-to-work patients reported flu-like symptoms post-withdrawal. Keep reading—this isn’t just about drowsy days.
Brain Zaps and Electrical Sensations
Ever felt like your thoughts are getting zapped mid-frequency? Patients describe these weird electric tingles as “my brain hitting its reset button.” Sven Huber went through this with Lexapro, developing shooting pains akin to wired brains in his skull.
The scientific term is sensory disturbances, but let’s keep it real. It’s terrifying when you experience sudden zings that make you jerk your neck or feel like bugs crawling under your skin. Even milder brain hiccups like concentration issues or memory fog can haunt folks long after stopping Cymbalta or Prozac.
Emotional Whiplash: More Than Just Mood Swings
The Mayo Clinic dropped an essential truth: Your original depression symptoms might reappear before your brain chemistry recalibrates. But the real plot twist? Emotional numbness isn’t always the blues sneaking back. It’s your brain’s “catch me if you can” game with neurotransmitters.
Need proof science is on your side? Research from the Conversation shows long-term users report:
- Reduced emotional range: “I used to cry at a TV car ad. After stopping Effexor, I couldn’t feel my nephew’s laughter.”
- Heightened anxiety: “I stopped Venlafaxine last fall. By week three, I needed noise-canceling headphones just to survive dinner parties.”
Your Blood Sugar Doesn’t Care What You Take—Until You Stop
Where’s the weird stuff show up? Like your digestive system feeling queasy for no reason, or your nerves short-circuiting the second you stop. The Cleveland Clinic lists them as “NEW effects”—not remnants of old depression, just your brain chemistry freakout. Common ones include:
| System Affected | What You Might Feel | Literary Analogy |
|---|---|---|
| Serotonin system | Electric shocks | Like popping down a faulty extension cord |
| Sleep-wake cycle | Vivid nightmares | Channeling your cinematic stress |
Moving forward—the kind of stuff that lasts longer than a few weeks. Spoiler: what works in week two might not rescue you at month six. Keep those options open.
The Long Haul: Why Some Symptoms Stick Around
This part’s real messy. The Lancet stats looked only at study subjects treated 8–12 weeks. Meanwhile, new research from 2025 says symptoms often return when patients stop after years. Of those who used antidepressants over two years, 66% experienced movement disorders, chronic fatigue, and cognitive glitches. Let’s not make this a guessing game—let’s lay it all out based on those real-life survivor logs.
Nerve Pain and Movement Woes
The link between serotonin levels and nerve pain isn’t just some psych textbook theory. Phillipa Munari’s story: after stopping Effexor, she felt like she’d trained horses all day with her mobility
Beware warnings, folks.
Sexual Dysfunction: Not Just a Side Effect
Yes, sex drive drops are common. But long after stopping antidepressants? That numbness might linger. Sven Huber’s experience? Blurred vision, organ desensitization, even cognitive fog. The Lancet showed this in 18% of long-term Cymbalta survivors who attempted discontinuation. Keep those hormone levels curious—
Emotional Numbness: It’s Not Just In Your Head
Saying “emotional flatness” oversimplifies things. Huber from Germany put it like this: “One day, my feelings got unplugged. After six months off meds, I still feel like I left half my memories at the pharmacy counter.” That’s not depression returning post-med—
Smell, Sound, and Taste Overload
Ever walked in somewhere familiar, but everything smells… off? Sensory disturbances aren’t relegated to electric zaps. They seep into everyday life:
- Phantom smells like burnt toast during quiet moments
- Hypersensitivity to sounds
- Lopsided taste buds – like your favorite chocolate suddenly tastes bitter
They’re not just sci-fi side effects. Our minds adapt when serotonin’s steady rhythm gets tripped up. Strange dreams? Check. Sensory anomalies? Also check. Keep these long-term symptoms in mind…
Medications That Make Stopping Tricky
Does your SSRI have an “outta pocket” clause? Let’s unpack why.
- Paroxetine (Paxil): The number 1 medication triggering withdrawal effects across Europe.
- Venlafaxine (Effexor): Its short half-life’s like trying to steer a leaky kayak—
UK doctors started advising patients way back in 2019: If you’re stopping short-half-life meds like Zoloft or Cymbalta, dial in a slow taper. Harvard Health’s advice?
Differences Between Short-, Medium-, and Long-Half-Life Drugs
| Type | Examples | Timeframe | Keyword Terms |
|---|---|---|---|
| Short | Paxil, Effexor | Popular for quick action, but horrid for tapering | Sensory disturbances, dizziness |
| Medium | Zoloft, Lexapro | Balance act in half-life and withdrawal severity | Emotional numbness |
| Long | Prozac (Fluoxetine) | Low withdrawal risk vs. others, but fuck the half-life length | Severe side effects |
Why does this matter? Because getting off long-half-life meds like Prozac gives your brain time to adjust. Short ones? It’s a roulette wheel of symptoms. You don’t want dizziness sidelining your reboot plan. Never skip your taper schedule—
High-Risk vs. Low-Risk Antidepressants
Picture this: Ads with flashy side effect disclaimers, but the real story’s in tapering prescribed profiles. Cleveland Clinic’s rankings should guide you:
Venlafaxine vs. duloxetine? Both SNRIs, but one (Effexor) bites harder than the other. Why? Effexor’s molecule isn’t sentimental—it’ll rebound withdrawal if you cut it too fast. Don’t gamble with your brain’s equilibrium.
Hitchhiking Through Recovery: How to Taper Safely
Lace up for this part—it’s about pace. Because just like your average recovery timeline after a surgery, antidepressant withdrawal isn’t a sprint. It’s more like having your Wi-Fi disconnected for three months while trying to stream Netflix 4K.
Talking to Your Doctor: Cut Both Ways
You’ve done your homework—but docs might not be fully read in. The Telegraph blew the whistle on MDs missing nerve pain after withdrawal symptoms arise. “One UK specialist told me, ‘This isn’t real,’” Munari admitted. His note? “How can I taper off if the system ignores what’s happening?”
Here’s your pep talk: Bring your stats, stories, and templates into that meeting room. Share your worries alongside your medical history. A doc yelling “relapse” without evaluating your timeline? Google them for a second opinion or a new approach.
Starting the Taper: What’s the Timeline?
How slow should your tapering go? Most guidelines suggest:
- 10% reduction every 2 weeks for meds like Lexapro
- Gradual tapering for at least three months for Effexor
If you’ve been on meds long-term (think 10+ years), don’t follow generic paths. Your plan might even shift from SSRI to SNRI reviewers like fluoxetine. Harvard Health’s feedback loop? “We often suggest patients go back to Prozac during tapering if others drop out too fast.”
Why’s this important? Your meds might’ve reset your biochemistry, and you need smoother roadways to reclaim ground without dizziness or depressive relapse.
Severe Symptoms: What Helps?
When you’re losing sleep and don’t know if it’s withdrawal or getting your soul back—some people need hospital reinforcements. Eating disorders aren’t the only risks. One patient let his anxiety snowball until driving felt too risky in motion.
Two emergency rules apply:
- Never reintroduce meds solo – talk to specialists before ); However, the second piece of advice is a mixed bag: bringing medications back up risks re-introducing withdrawal again. Make sure you’re tapering at the doc’s pace—and not rushing pressure from fiscal deadlines.
Documenting Symptoms at Home
Do you track your sugar levels when resuming diabetes meds? Same here. Keep a journal:
- Daily symptoms
- Hours since last dose
- Energy vs. fatigue scores
Here’s what real people track: Huber kept a sexual function journal with ratings from 1–10. If things felt worse each week? He mentioned it at follow-up appointments. Get yours in order…
What Now? Joining Support Communities
Your gym buddy supports biceps, but your emotional recovery deserves Tribe ties. Meet the people who can hold your hand (figuratively). Cleveland Clinic’s data shows 85% of long-term users need adjustments just to get back on their feet.
Online Forums vs. Medical Advice
Here’s the catch: Your doctor might say “nope” to YouTube tapering protocols. But secret TikTok groups? Some have helped real folks get back into work. Meanwhile, Massachusetts General Hospital recommends psychiatrist involvement for those over 50… suggesting professional oversight isn’t optional.
Key takeaway? Blend trust in patient narratives with medical need for documentation. The Mind.org guidelines say to cross-reference symptoms with your stages:
- Keep tracking records via the Yellow Card Scheme
- Ask about proven tapering schedules at follow-ups
Support Beyond Medication: Therapy and Counseling
Now for the real stuff: What if your meds got you healthy—but your brain needs a morning reboot every Sunday post-discontinuation? Cognitive skills, coping resources, and social support networks really do work. Harvard Health says “Therapy during tapering will lower the risk of relapse.”
Here’s the deal—if you walk this road without support, you’ll head down the wilderness. Voice lessons, breathing techniques—find your inner reset button. Because dependence on meds is medical, not moral failure.
Final Words
Antidepressants changed thousands of lives, but getting off them leaves no shortcuts. From anxiety and nerve pain to emotional numbness and insomnia, your journey’s unique.
So what should you do now? Don’t panic. Do…private Long-Term Brain Zaps Nearly zero ‘RED BRAIN’ syndrome Aka “I feel like I’m short-circuiting every hour”
Tell your friends that everyone was shocked by NPR’s revealing report, as many patients reported that their doctors did not warn them about these symptoms and were unable to offer solutions. While stopping antidepressants may produce short-term withdrawal symptoms, experts emphasize that long-term use can lead to more severe neuropathic pain or emotional paralysis, and when neurotransmitters are greatly reduced (such as with long-term use of SSRIs), the process of restoring neurotransmitters is much longer than normal withdrawal symptoms. The bottom line is that patients need longer tapering periods, especially when there is not enough scientific support to guide doctors.
While you’re not “addicted” (antidepressants don’t hit your reward cente)
Now for the real deal: Your body and brain adapted to having these meds. They’re not betraying you now—they’re simply recalibrating. So whether you’re on your third week or third year post-discontinuation, the keyword isn’t ‘survivor’—it’s patience.
Can we end on a hope-filled note? Yes. When someone like Huber reconnects with their emotional range after two years? They’re not alone. Others are on the same rollercoaster, vetting what works viscosity section or half-life time.




















Leave a Reply
You must be logged in to post a comment.