Imagine a tiny gate in each brain cell that lets in a vital fuel—citrate. If that gate jams, the cell’s engine stalls, and the electrical storm that is epilepsy can erupt. That’s exactly what happens when the brain’s citrate‑shuttle, the SLC13A5 transporter, goes wrong. In just a few minutes you’ll see why a single protein defect can tip the balance from normal thinking to relentless seizures, and what science is doing to fix it.
Why should you care if you’re not a neurologist? Because the story of a faulty transport protein teaches us a universal lesson: even the smallest molecular glitch can reshape a whole organ system. By the end of this read you’ll understand the chemistry, the clinical reality, and the hope that new therapies bring—plus a few practical tips if you ever meet a family navigating this rare condition.
What is SLC13A5?
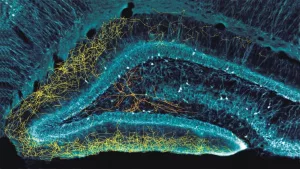
SLC13A5 belongs to the solute carrier family 13, a group of membrane proteins that move small molecules across the cell’s outer wall. Think of it as a diligent bouncer at a nightclub: it only lets citrate (bound to sodium) slip inside the neuron, while keeping the wrong crowd out.
The protein spans the membrane twelve times, forming a barrel‑like tunnel. Inside that tunnel, citrate rides on the sodium gradient, exiting the blood and entering the neuron where it can be turned into acetyl‑CoA—a building block for lipids, neurotransmitters, and energy.
When the brain transport protein works flawlessly, your neurons stay powered, membranes stay flexible, and the brain’s electrical chatter stays balanced.
How Faulty Protein Disrupts
Mutations in the SLC13A5 gene come in several flavors—missense changes that swap one amino‑acid for another, nonsense mutations that cut the protein short, and splice‑site glitches that scramble the instruction manual. The most common culprit is a missense variant that replaces a glycine with an arginine at position 460 (p.Gly460Arg). This change narrows the tunnel, lowering the maximum transport rate (Vmax) and sometimes preventing the protein from reaching the plasma membrane at all.
When the protein cannot find its way to the cell surface, it gets stuck inside the endoplasmic reticulum, a situation remarkably similar to what researchers observed in zinc‑transporter mutations that cause acrodermatitis enteropathica. A study showed that mis‑trafficking can be just as damaging as a broken gate.
Why does this matter for neuron metabolism? Citrate is the primary source of acetyl‑CoA in the brain. Without enough acetyl‑CoA, neurons can’t synthesize the fatty acids needed for myelin, nor can they produce the neurotransmitter GABA efficiently. The resulting deficit tilts the excitation‑inhibition balance toward excitability, making seizures more likely.
| Mutation Type | Effect on Protein | Metabolic Consequence |
|---|---|---|
| Missense (e.g., p.Gly460Arg) | Reduced transport velocity; occasional ER retention | Lower intracellular citrate → ↓ acetyl‑CoA |
| Nonsense (early stop) | Truncated protein, no membrane insertion | Complete loss of citrate import |
| Splice‑site | Aberrant exon skipping, misfolded protein | Variable loss, often mis‑trafficking |
Clinical Picture Explained
Kids with a broken SLC13A5 transporter usually present in the first weeks of life. The seizures are often tonic‑clonic bursts that can progress to status epilepticus—a life‑threatening condition where the brain refuses to ‘turn the lights off.’ Because citrate deficiency also hampers brain development, affected children typically show developmental delay, motor weakness, and speech impairment.
This constellation of early‑onset seizures and neurodevelopmental regression meets the definition of severe epileptic encephalopathy. In practice, the term signals that the seizures themselves are contributing to the ongoing brain injury, not just a symptom.
Electroencephalograms (EEGs) often reveal a “burst‑suppression” pattern—sharp spikes interspersed with flat lines—while brain MRIs may look normal early on, only to show delayed myelination later. The clinical story is heartbreaking, but knowing the underlying molecular cause gives families a roadmap for targeted testing and, eventually, precise therapy.
Diagnosis Made Simple
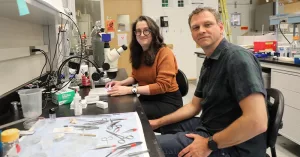
When a neonate has refractory seizures, the diagnostic algorithm should include a genetic work‑up early on. A gene panel that covers epilepsy‑related transporters, followed by whole‑exome sequencing if the panel is negative, will usually flag SLC13A5 variants.
Once a variant is found, confirmation by Sanger sequencing ensures it isn’t a sequencing artefact. Then, the laboratory may perform a functional assay—expressing the mutant protein in cultured cells to see whether citrate uptake is reduced.
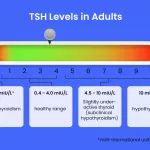
Blood tests can provide supportive clues. While serum citrate is typically normal (because most citrate lives intracellularly), cerebrospinal fluid (CSF) may show reduced citrate levels. A comparative table helps clinicians visualize these differences:
| Parameter | Normal | Typical in SLC13A5 Deficiency |
|---|---|---|
| Serum Citrate | 0.2–0.5 mmol/L | Within normal range |
| CSF Citrate | 0.3–0.7 mmol/L | ↓ (often < 0.3 mmol/L) |
| GABA Levels (CSF) | Normal | ↓ due to reduced acetyl‑CoA |
When you see these red flags, think “faulty transport protein” and order the test. Early diagnosis not only guides treatment but also connects families with support groups and clinical trials.
Treatment Landscape Today
Right now, no drug can directly repair a broken SLC13A5 transporter. Management therefore focuses on two fronts: controlling seizures and supporting neuronal metabolism.
Seizure control: First‑line antiepileptic drugs (ASDs) such as phenobarbital, levetiracetam, and topiramate are commonly used. Some families report modest benefit from the ketogenic diet, which supplies alternative fuels (ketone bodies) that bypass the citrate block. However, the diet is demanding and must be supervised by a dietitian.
Metabolic support: Researchers are testing citrate analogues that can cross the membrane without needing SLC13A5. Early animal models suggest these molecules raise intracellular acetyl‑CoA and improve GABA synthesis. The neuron metabolism angle is a hot topic, especially after a 2022 Science paper highlighted the signal‑peptidase complex as a quality‑control enzyme for membrane proteins—showing that the cell already has backup strategies for faulty transporters.
Emerging therapies: Gene‑replacement using adeno‑associated viruses (AAV) is progressing in mouse models. By delivering a functional copy of SLC13A5 directly to the brain, researchers have restored citrate uptake and reduced seizure frequency. Human trials are still in the pre‑clinical phase, but the momentum is encouraging.
In parallel, small‑molecule chaperones that help misfolded SLC13A5 reach the plasma membrane are under investigation. If successful, they could convert a non‑functional protein into a partially functional one, buying valuable time for patients.
Real‑World Experiences
Meet Maya, a bright‑eyes toddler who began having seizures at three days old. Her parents thought the “cry‑and‑stop” pattern was just colic—until a neurologist ordered rapid‑gene sequencing and uncovered a homozygous p.Gly460Arg variant. Within weeks, Maya was started on levetiracetam and a carefully monitored ketogenic diet. While her seizures lessened, her developmental milestones still lag. Maya’s family now participates in a clinical trial testing an AAV‑SLC13A5 construct, and they say the hope of a “real cure” keeps them moving forward.
Dr. Lina Hoffman, a pediatric neurologist at a major academic center, explains, “When you have a concrete genetic answer, you can stop the endless trial‑and‑error with medications and instead focus on targeted strategies and supportive care. It changes the conversation from ‘what’s wrong?’ to ‘what can we do?’”
Support groups, both online and in‑person, provide a lifeline. Families share tips on seizure‑action plans, feeding regimens, and navigating insurance for experimental therapies. Knowing you’re not alone turns the isolated feeling of a rare disease into a community of advocates.
Final Thoughts & Next Steps
In a nutshell, a faulty transport protein like SLC13A5 can cascade from a single molecular gate failure to severe epilepsy, developmental delay, and a whole family’s emotional roller‑coaster. Yet the story is also one of scientific ingenuity: from pinpointing the mutation to designing gene‑therapy vectors, researchers are turning a formidable obstacle into a solvable problem.
If you or someone you love is facing this diagnosis, remember that early genetic testing, a multidisciplinary care team, and staying informed about clinical trials are your best tools. And if you’re curious to dive deeper, explore our dedicated pages on SLC13A5 epilepsy, the broader class of brain transport proteins, and how they shape neuron metabolism.
What’s your take on the promise of gene therapy for rare neurological disorders? Do you have questions about managing seizures at home? Feel free to reach out—knowledge shared is power multiplied.


















Leave a Reply
You must be logged in to post a comment.